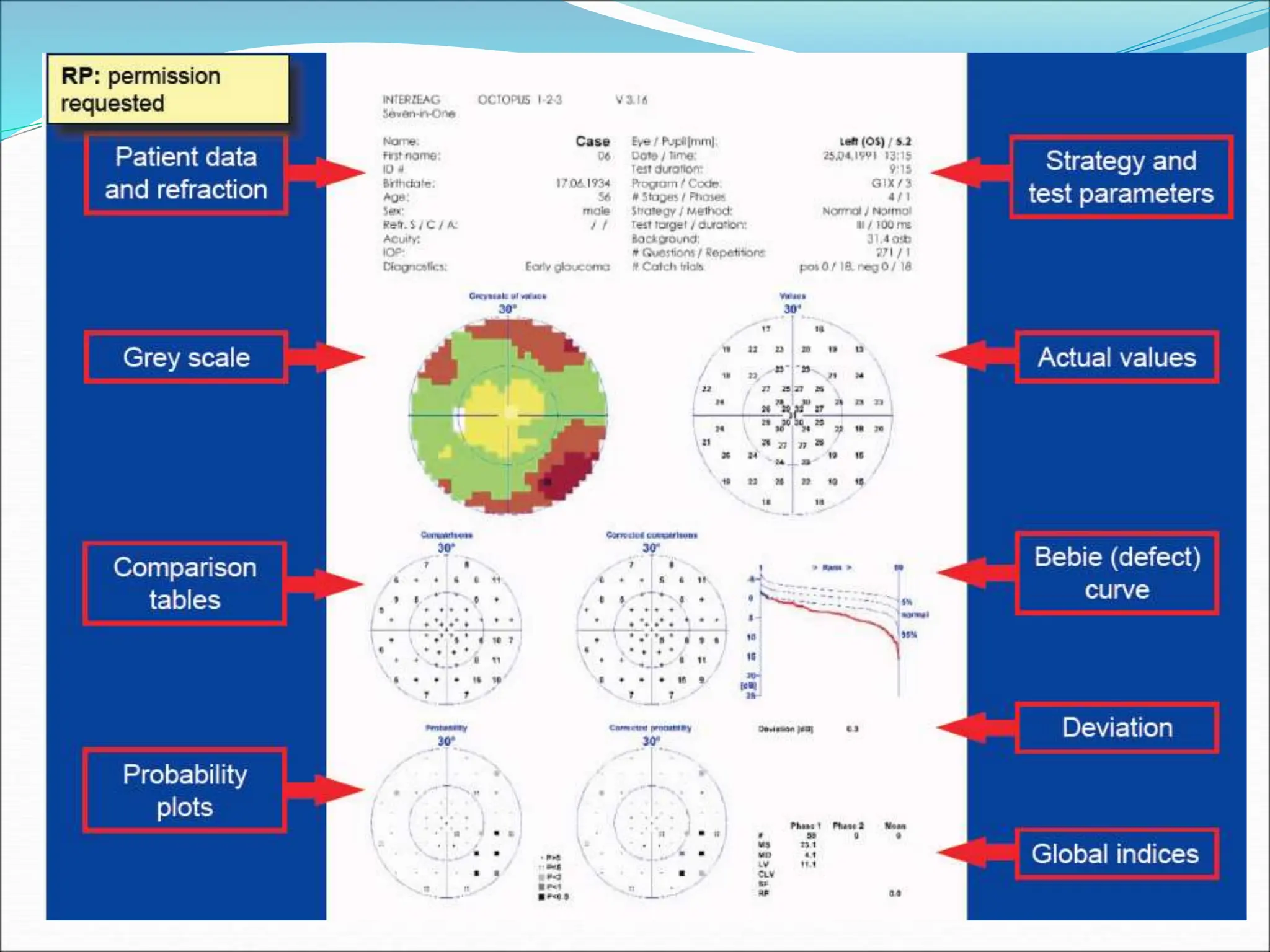
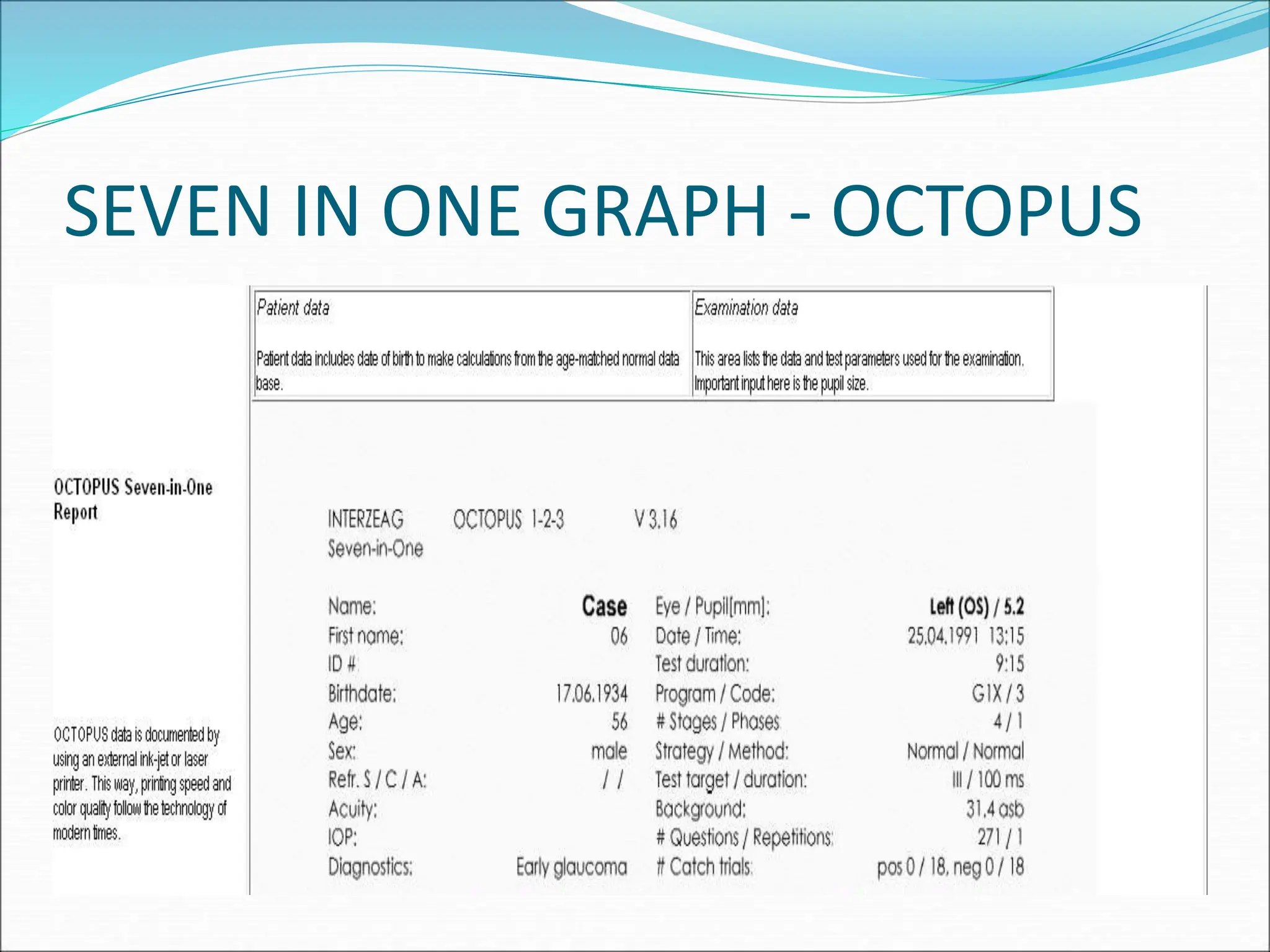
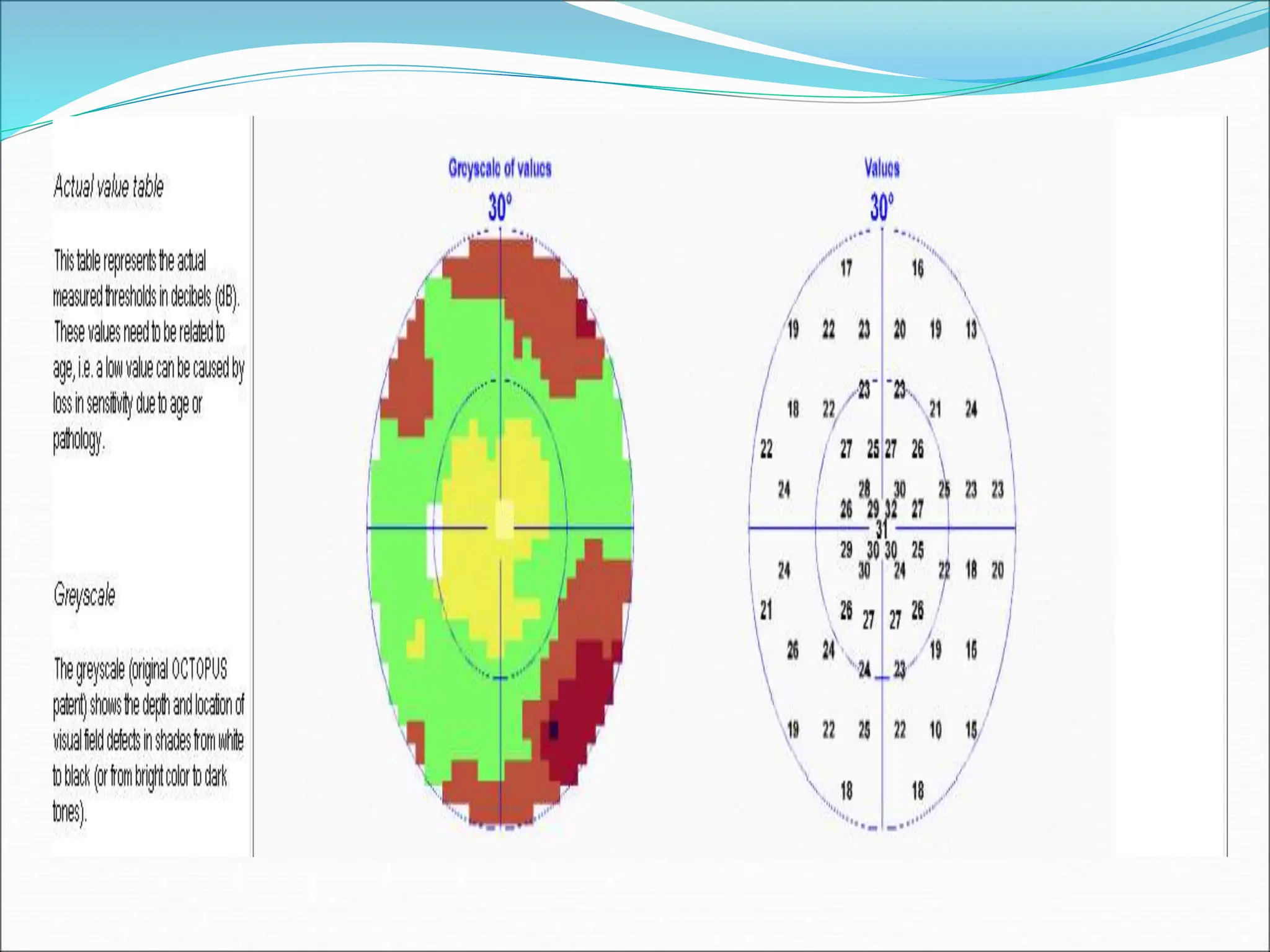
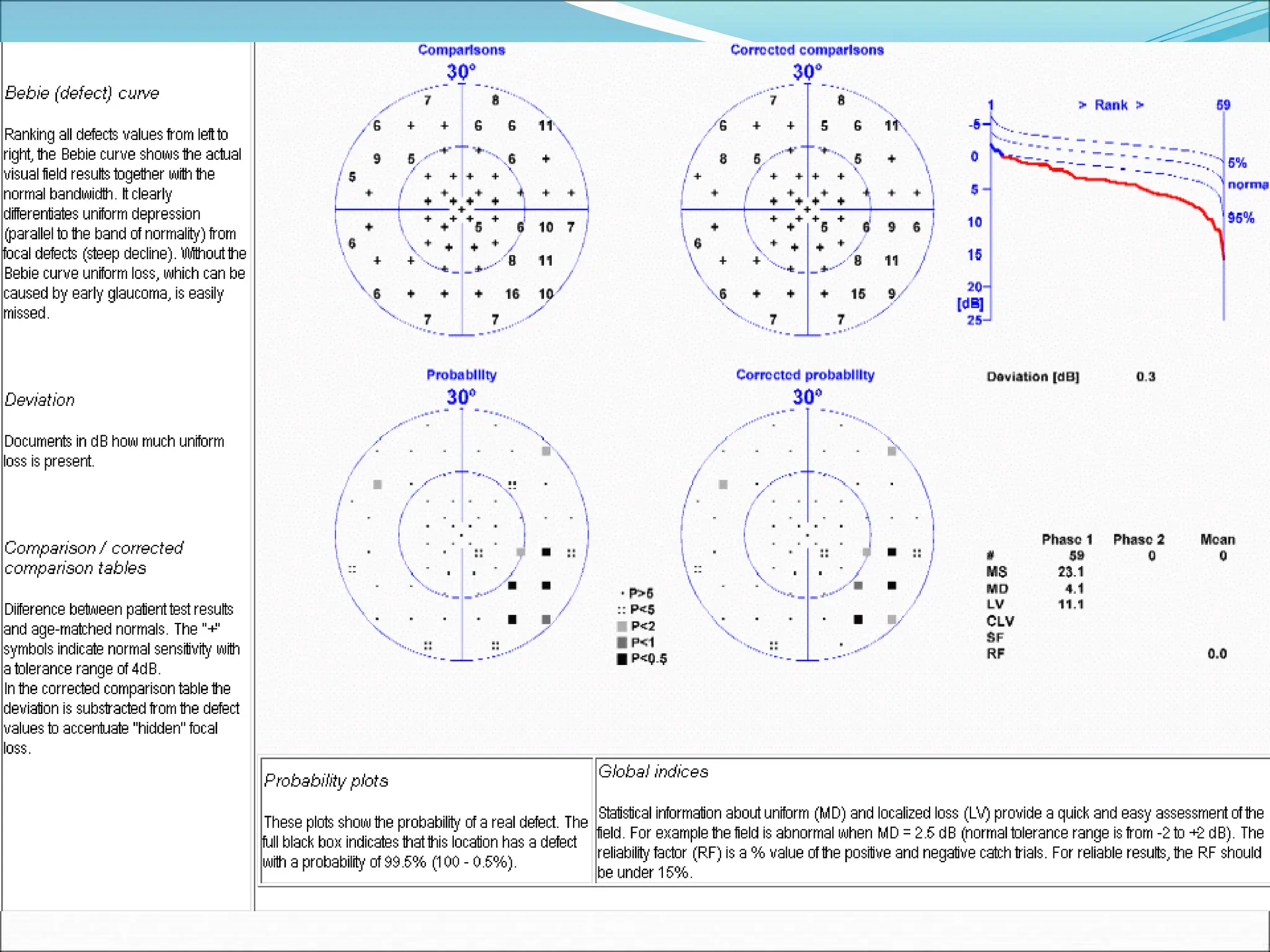
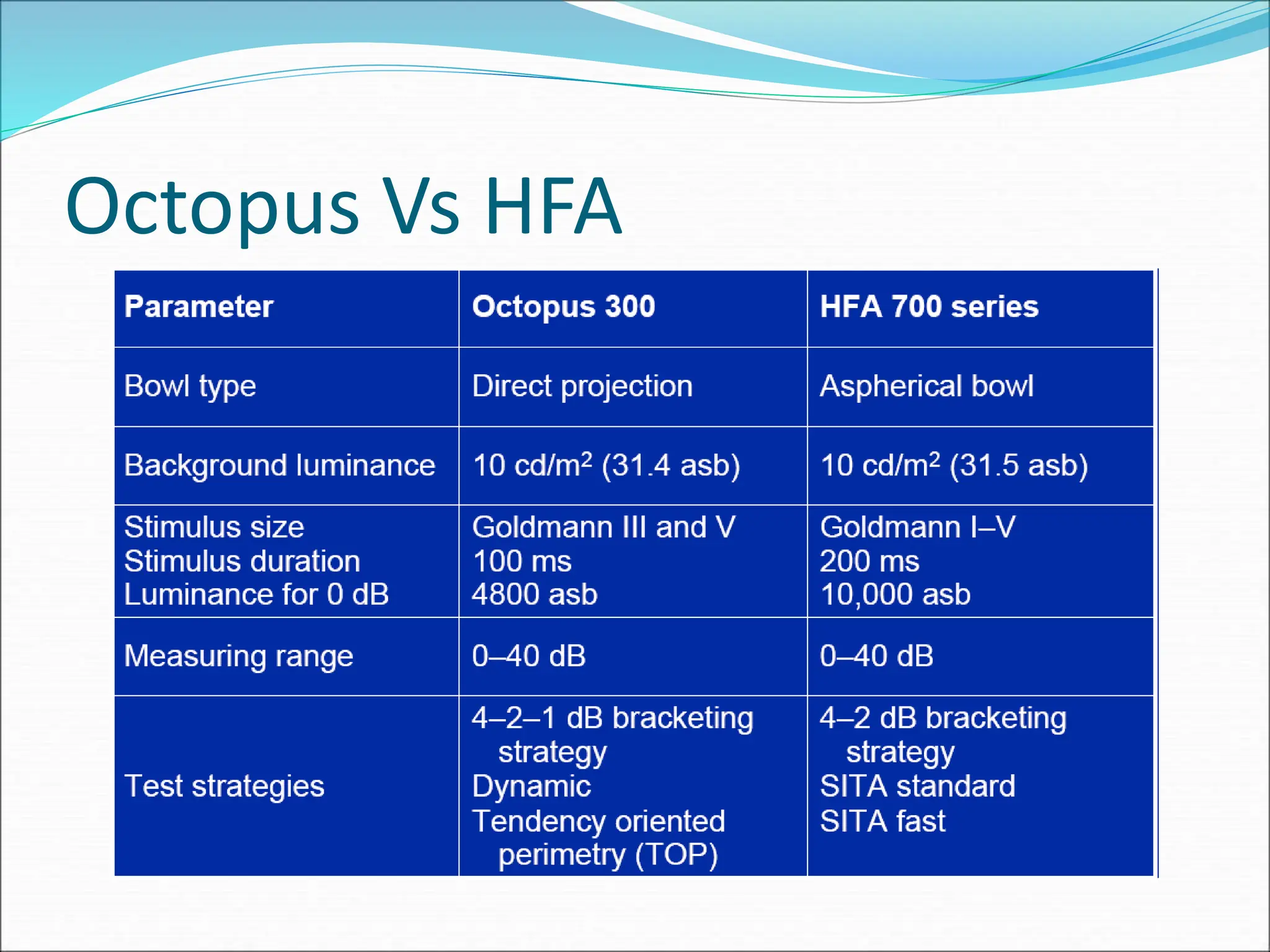
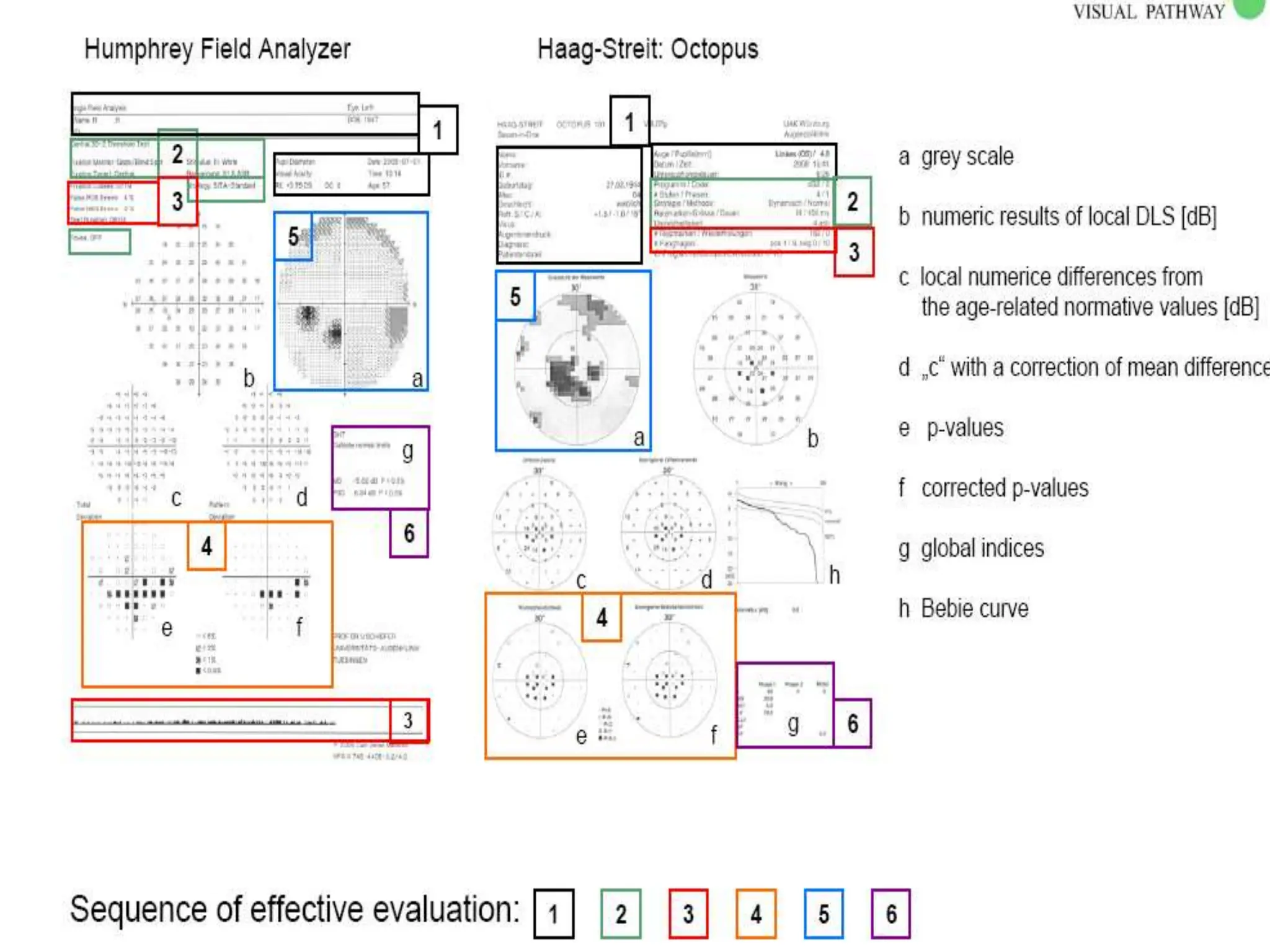
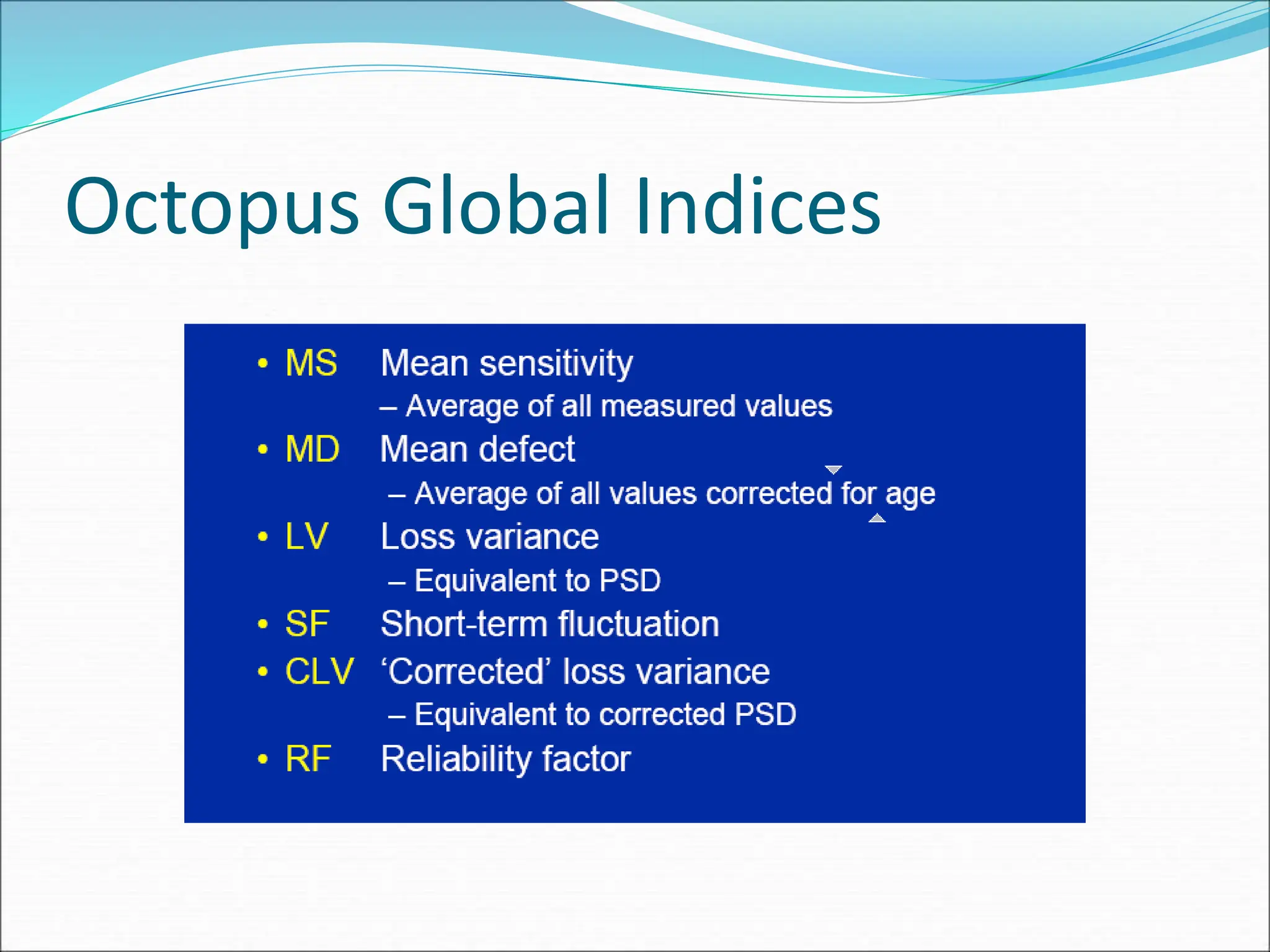
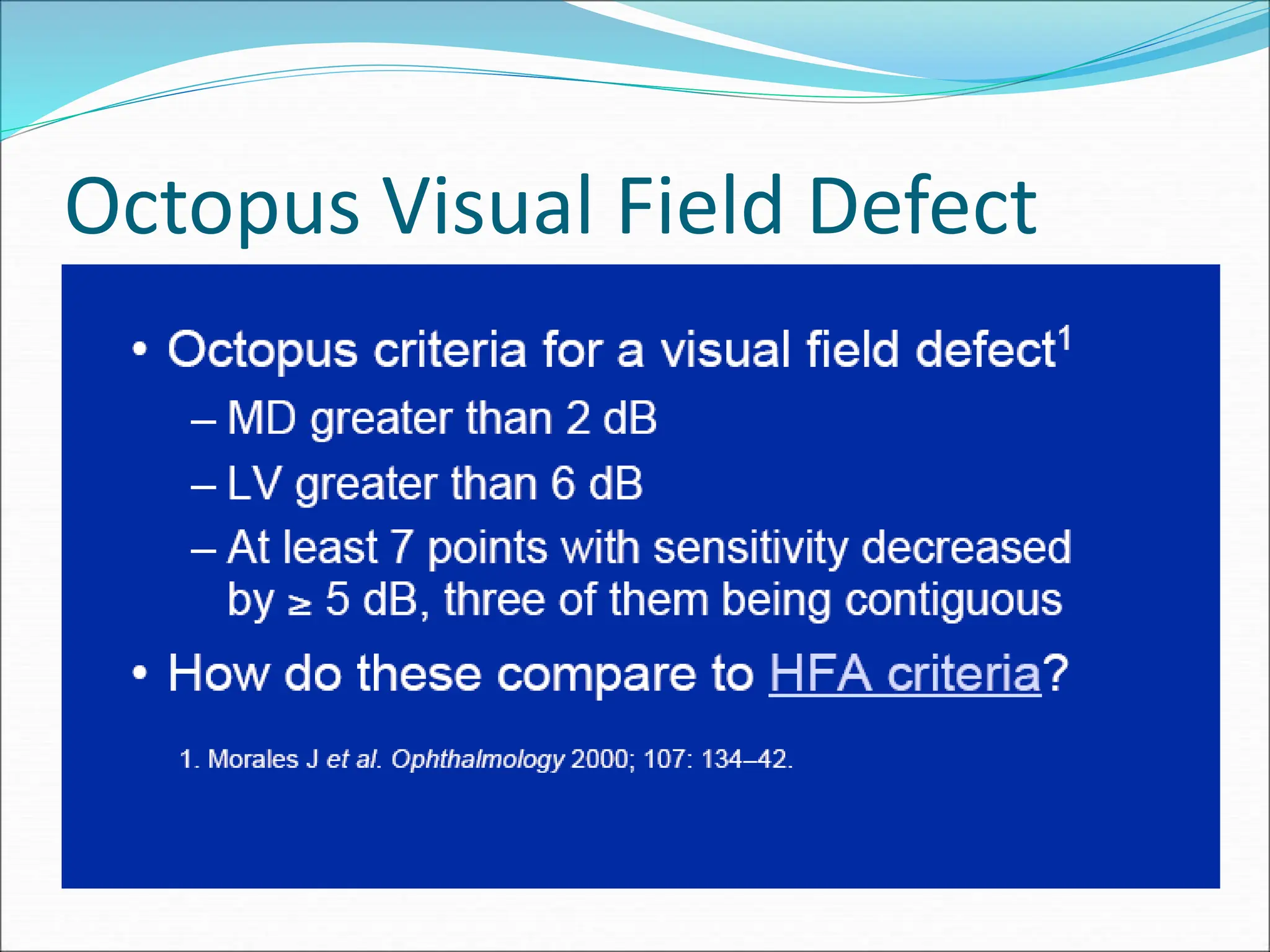
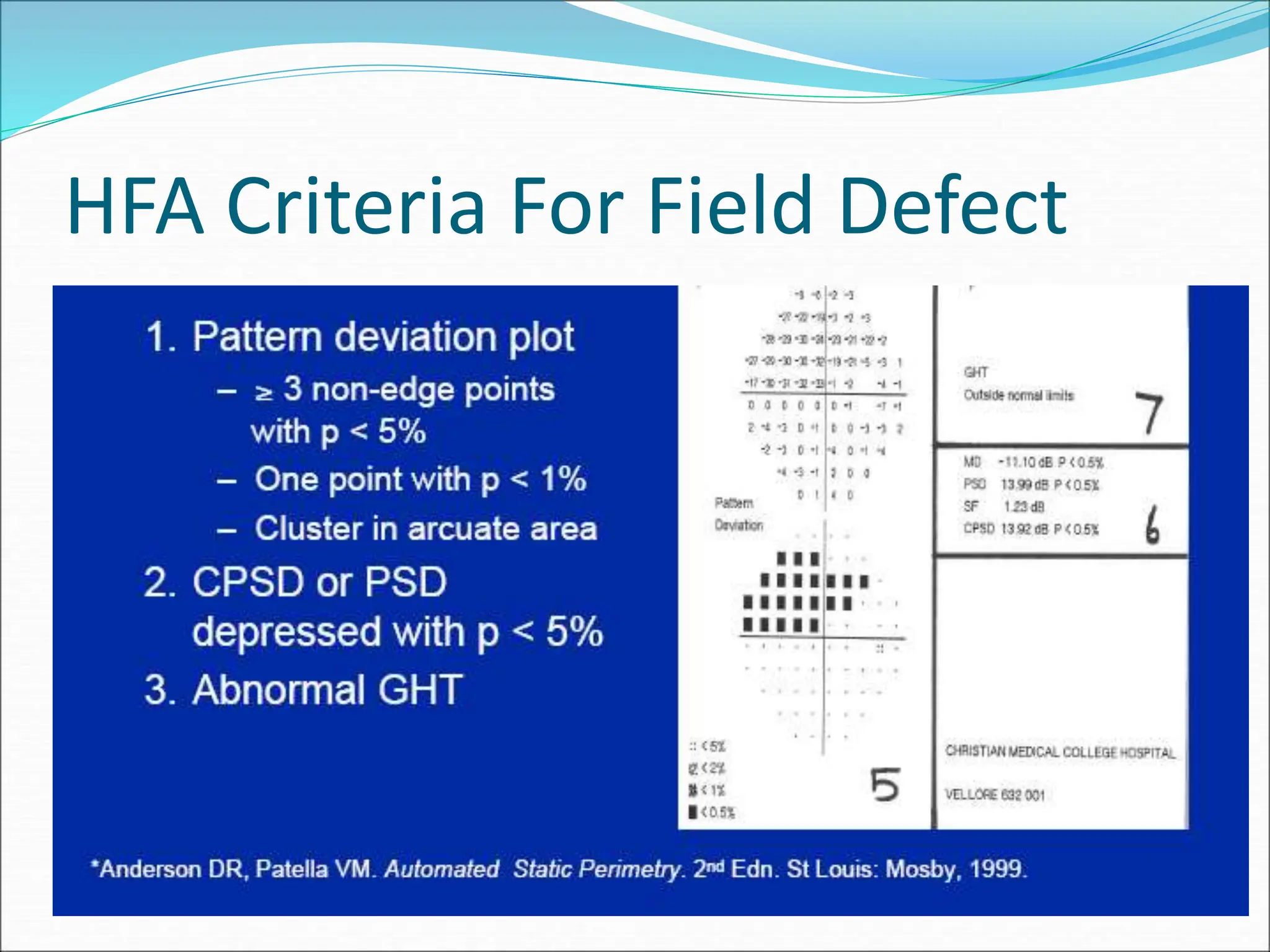
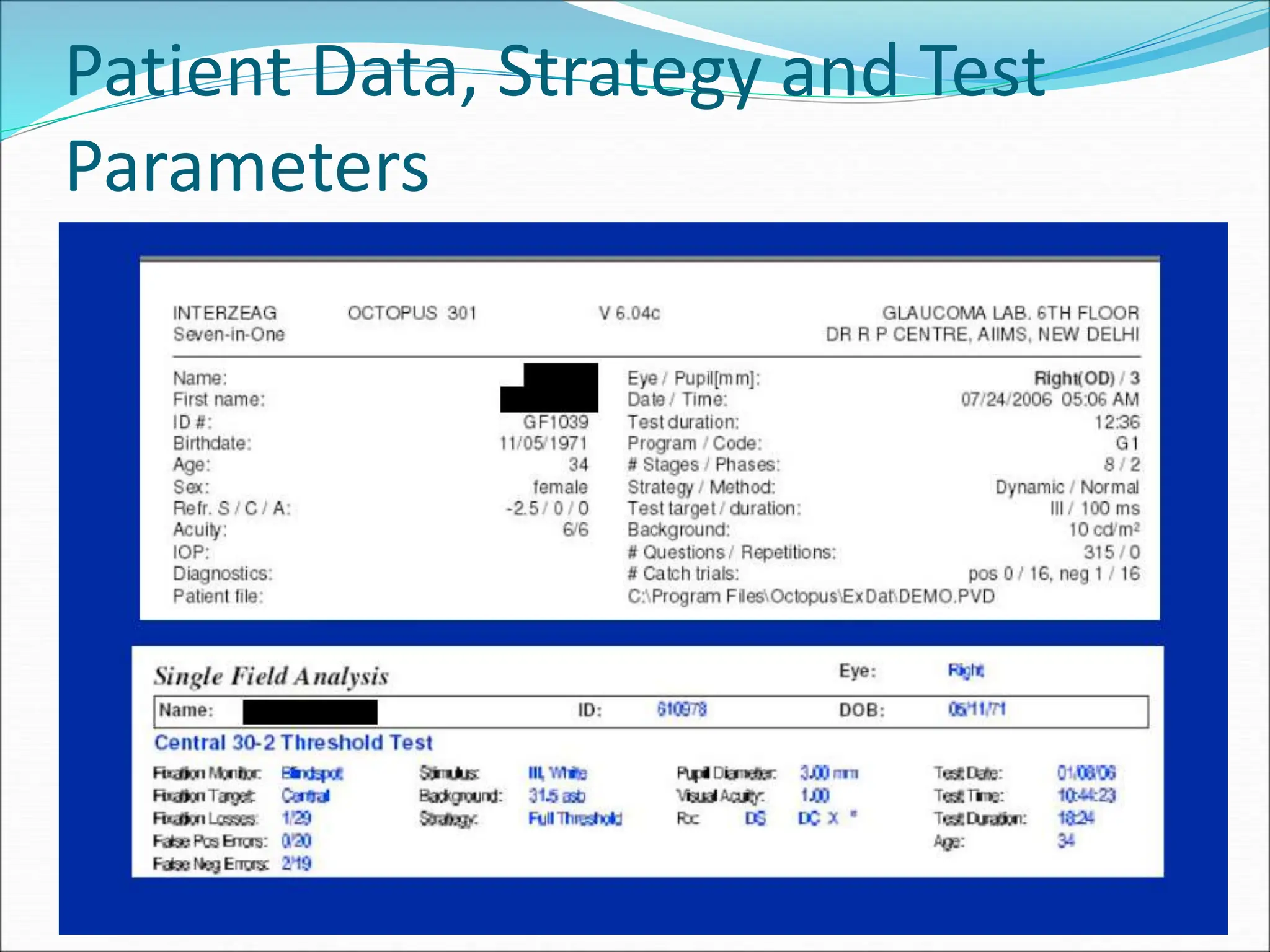
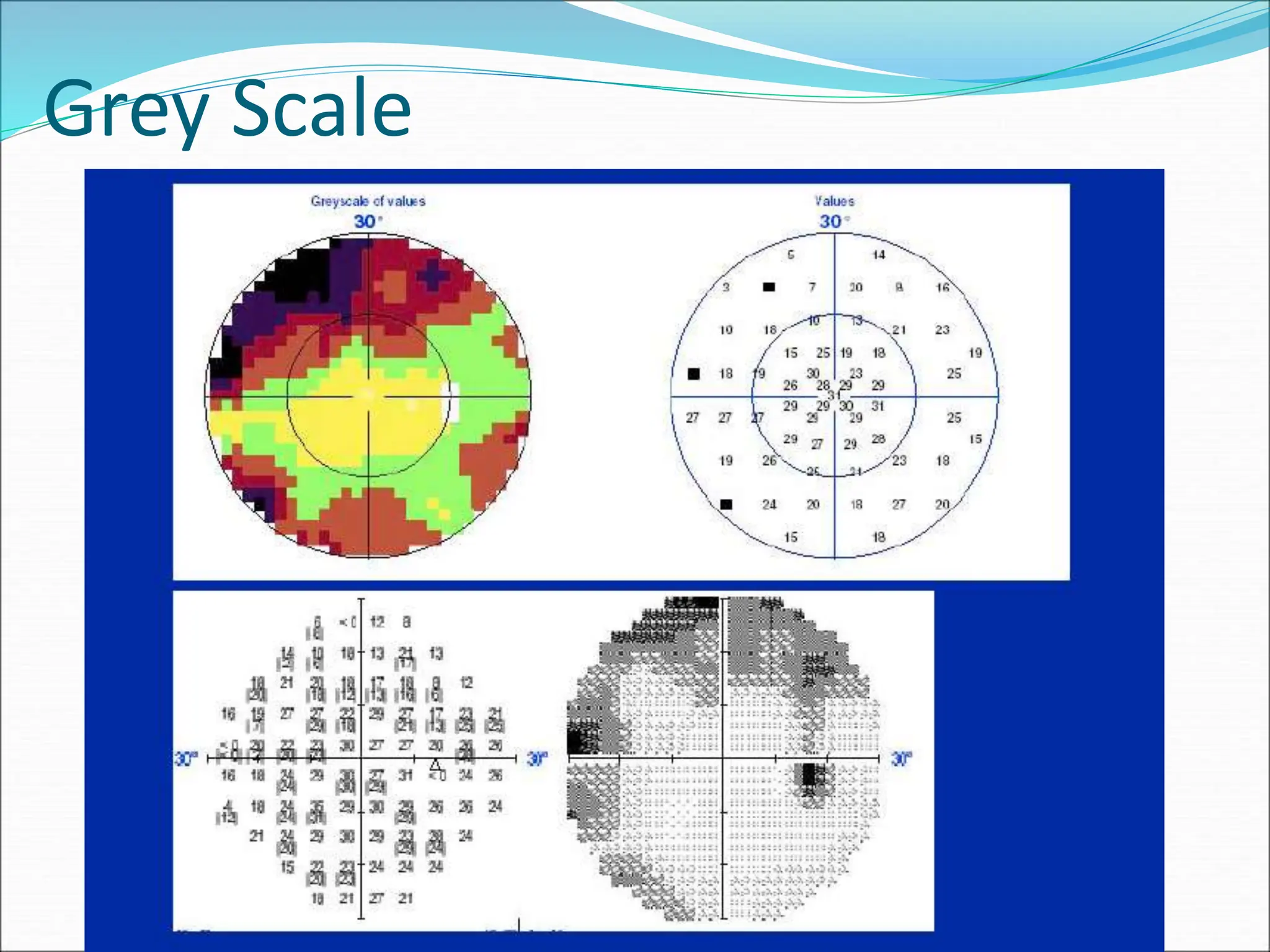
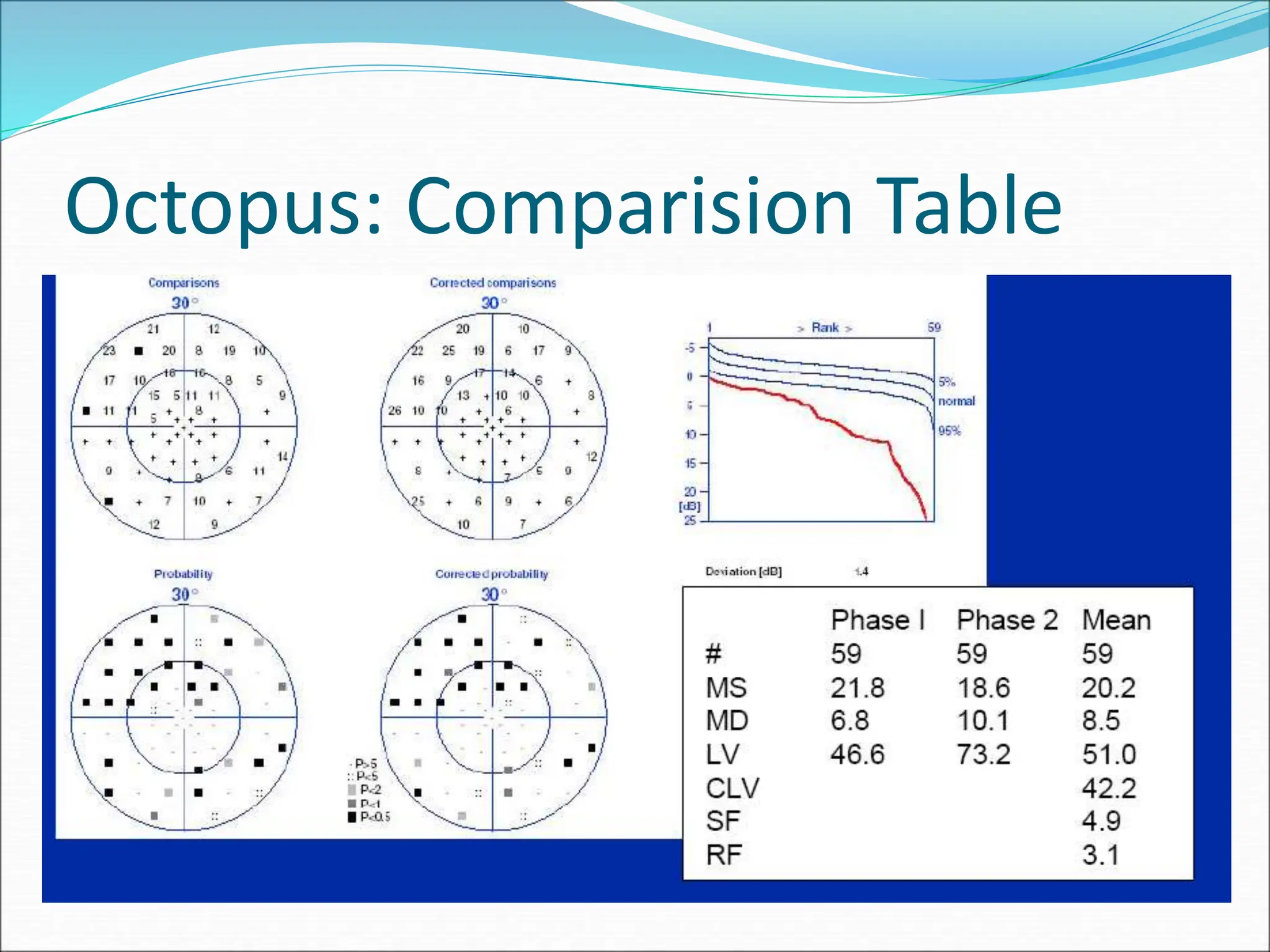
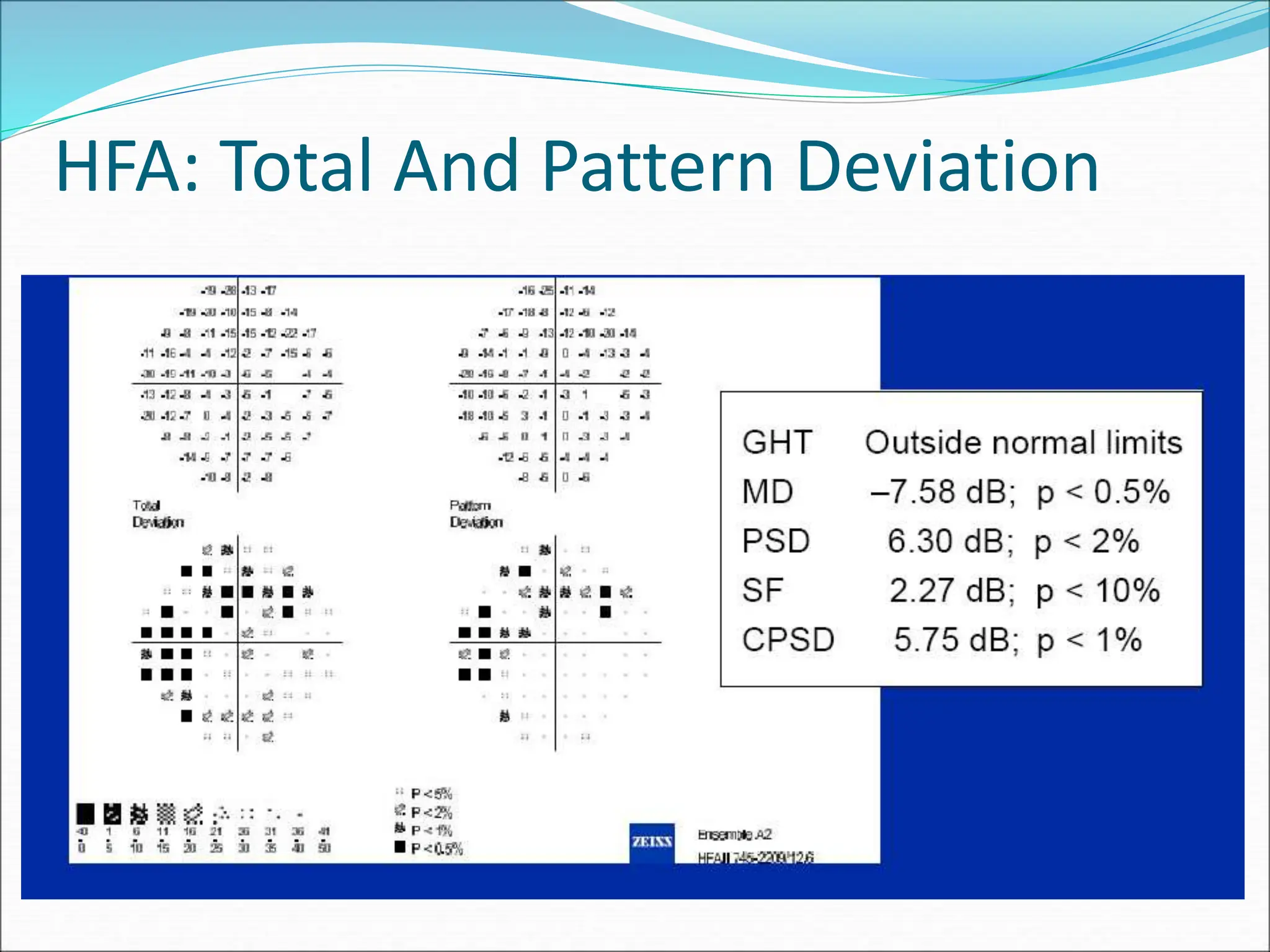
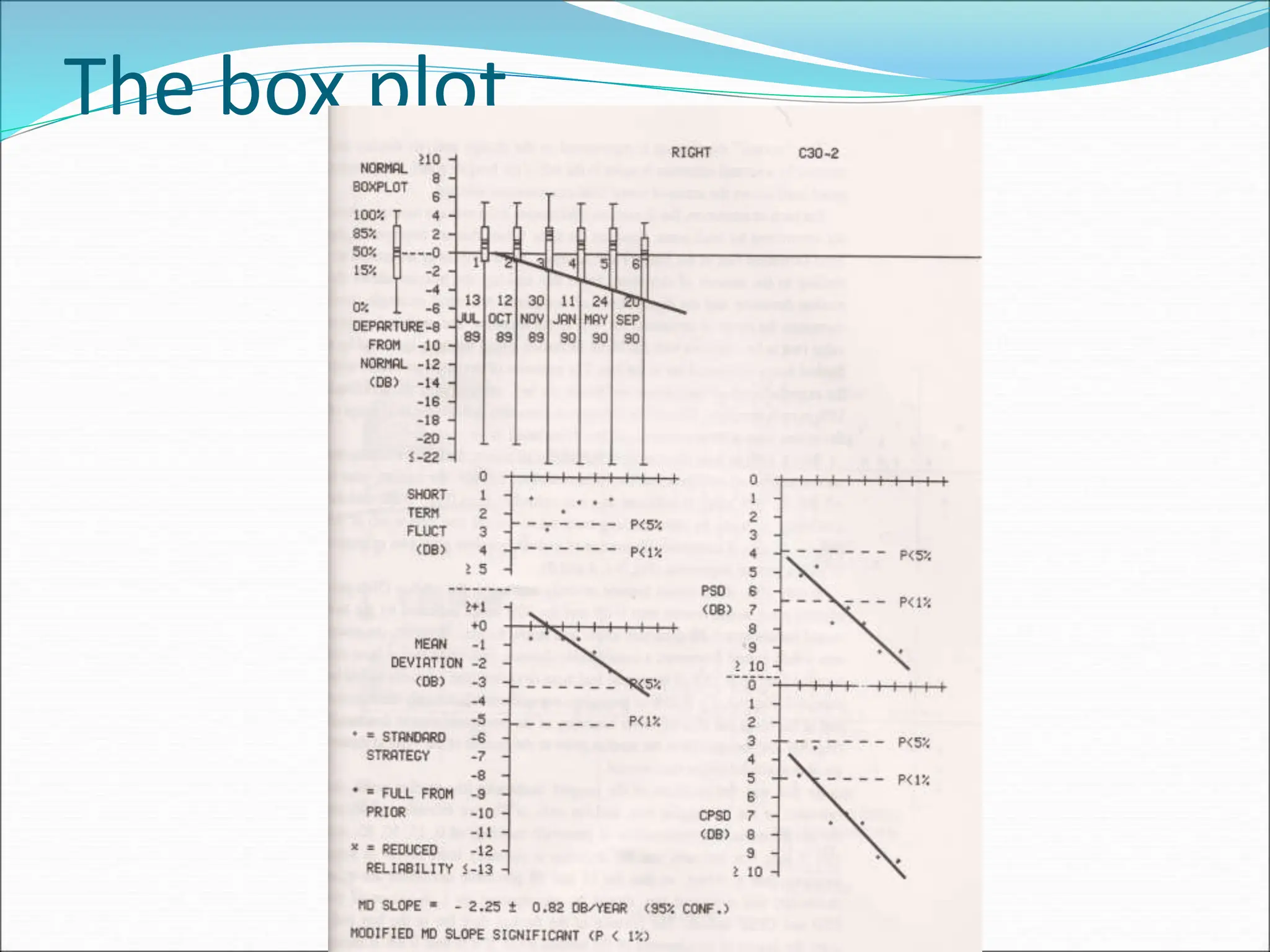
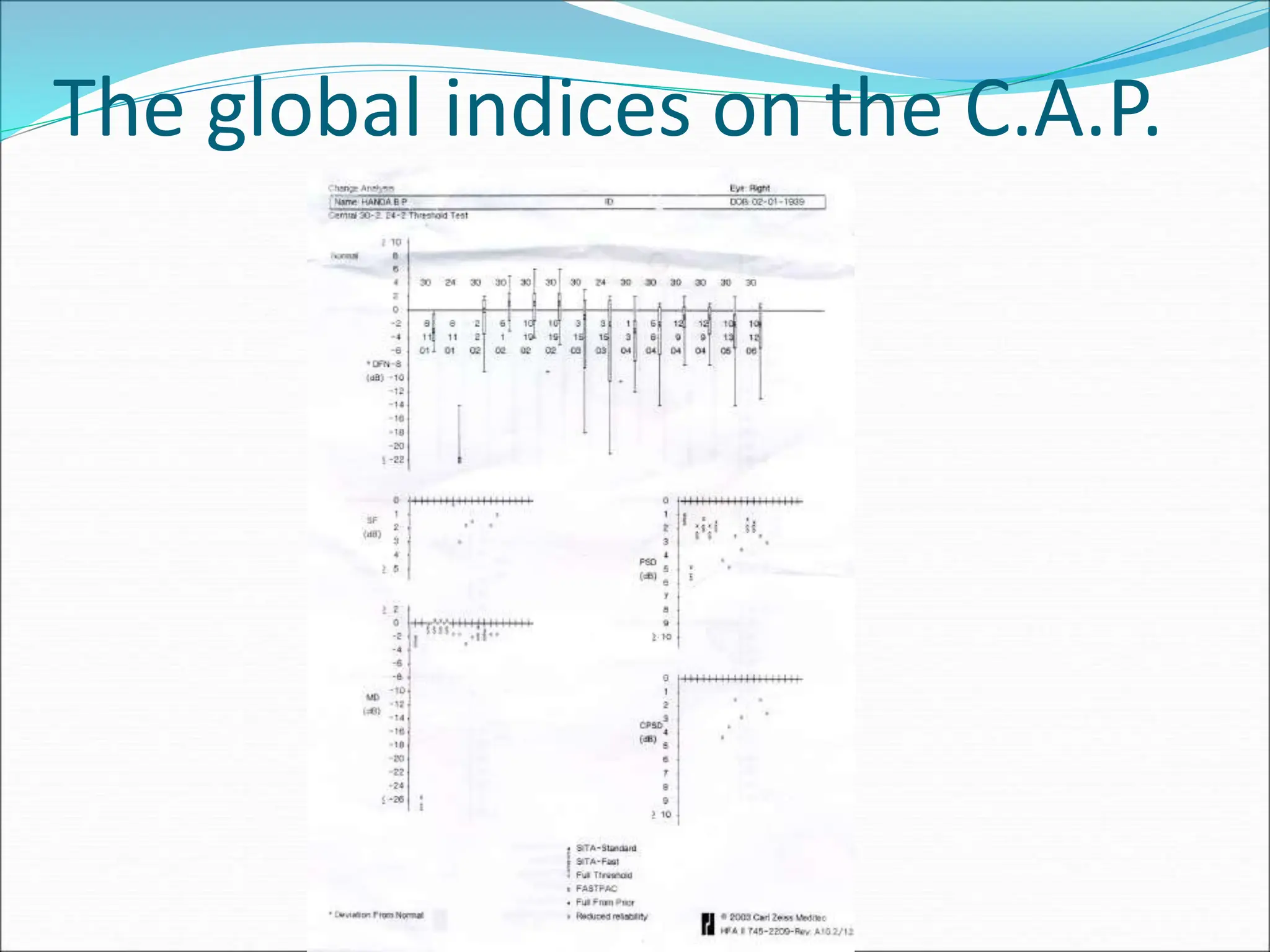
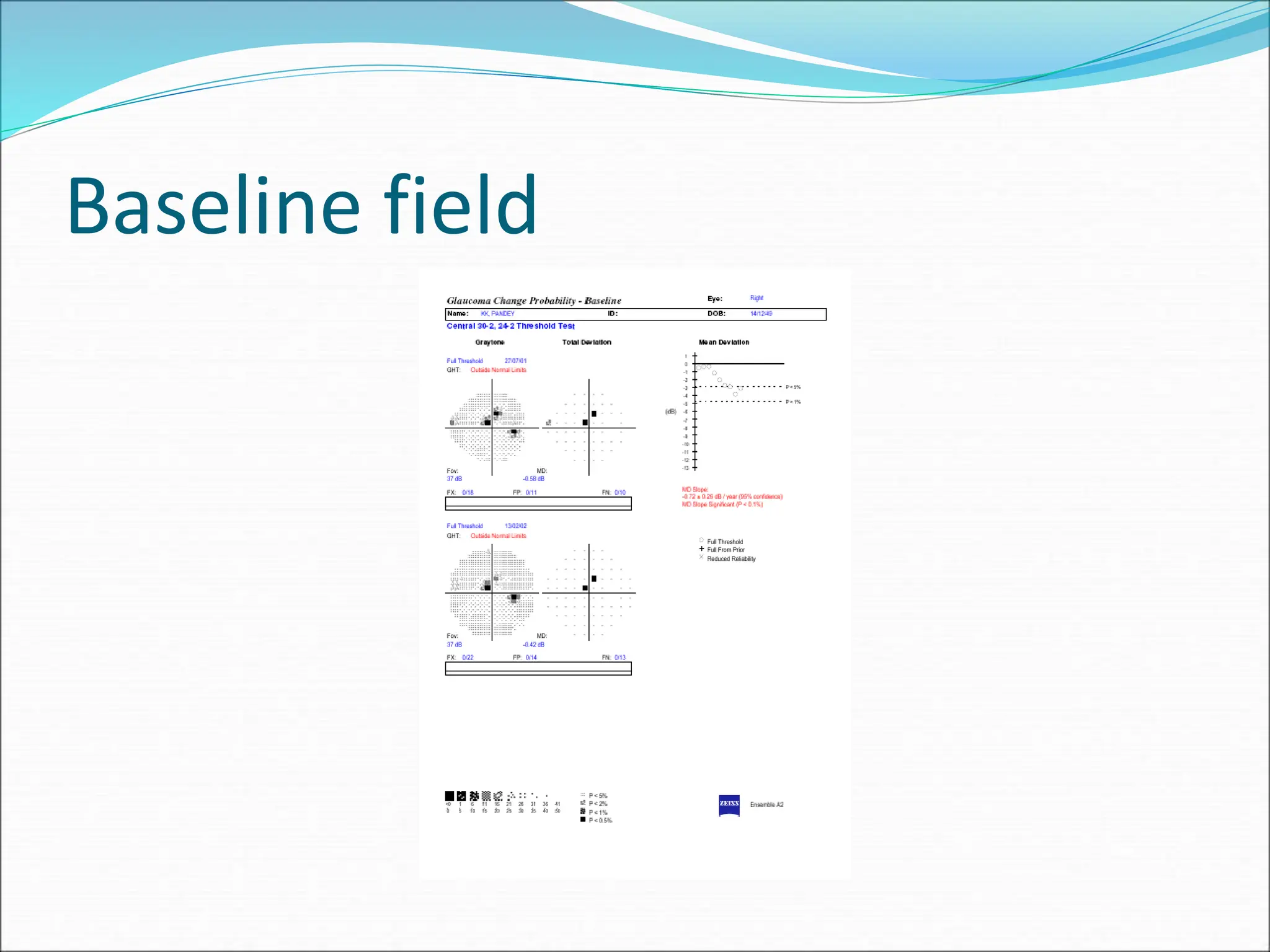
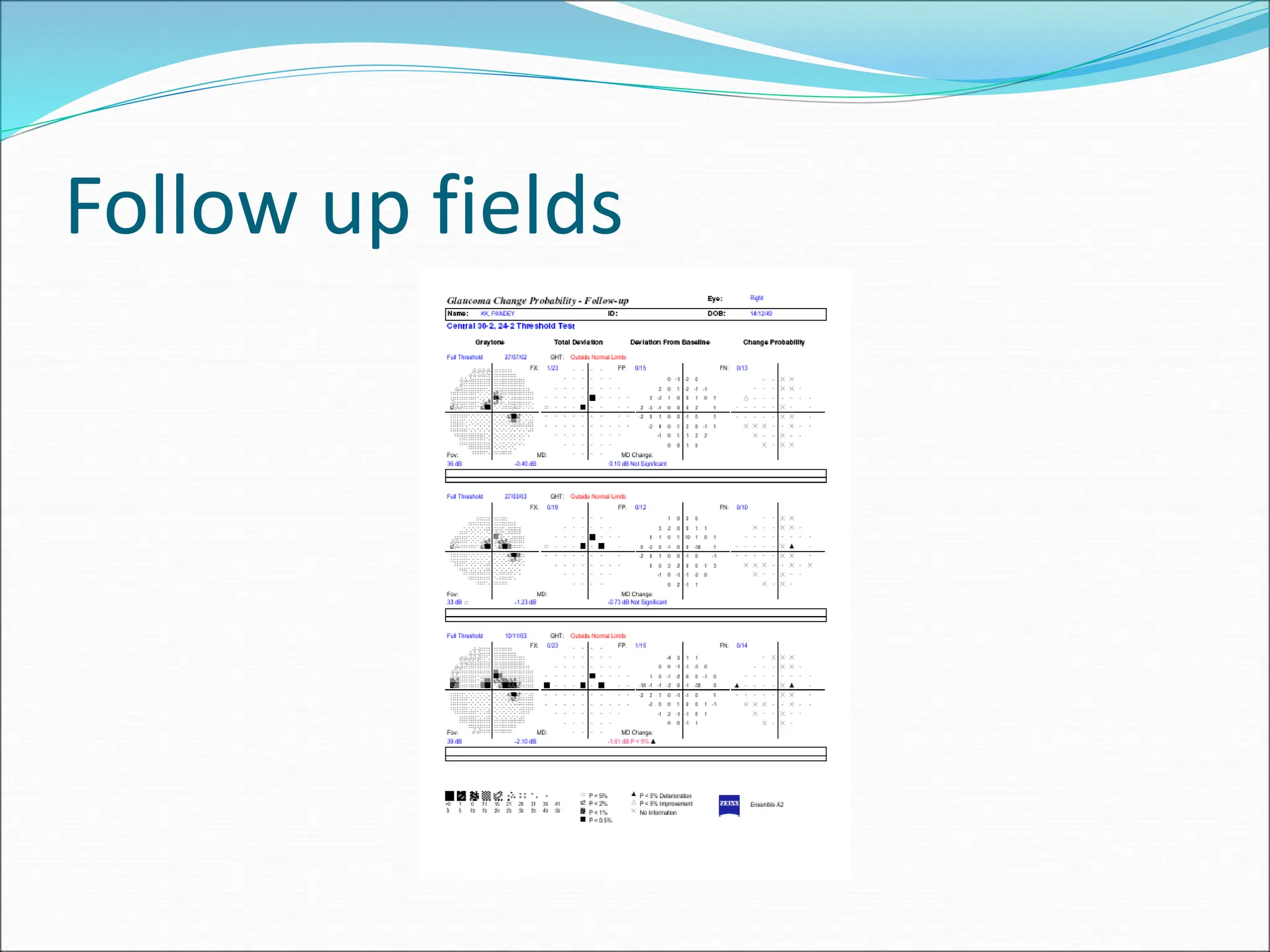
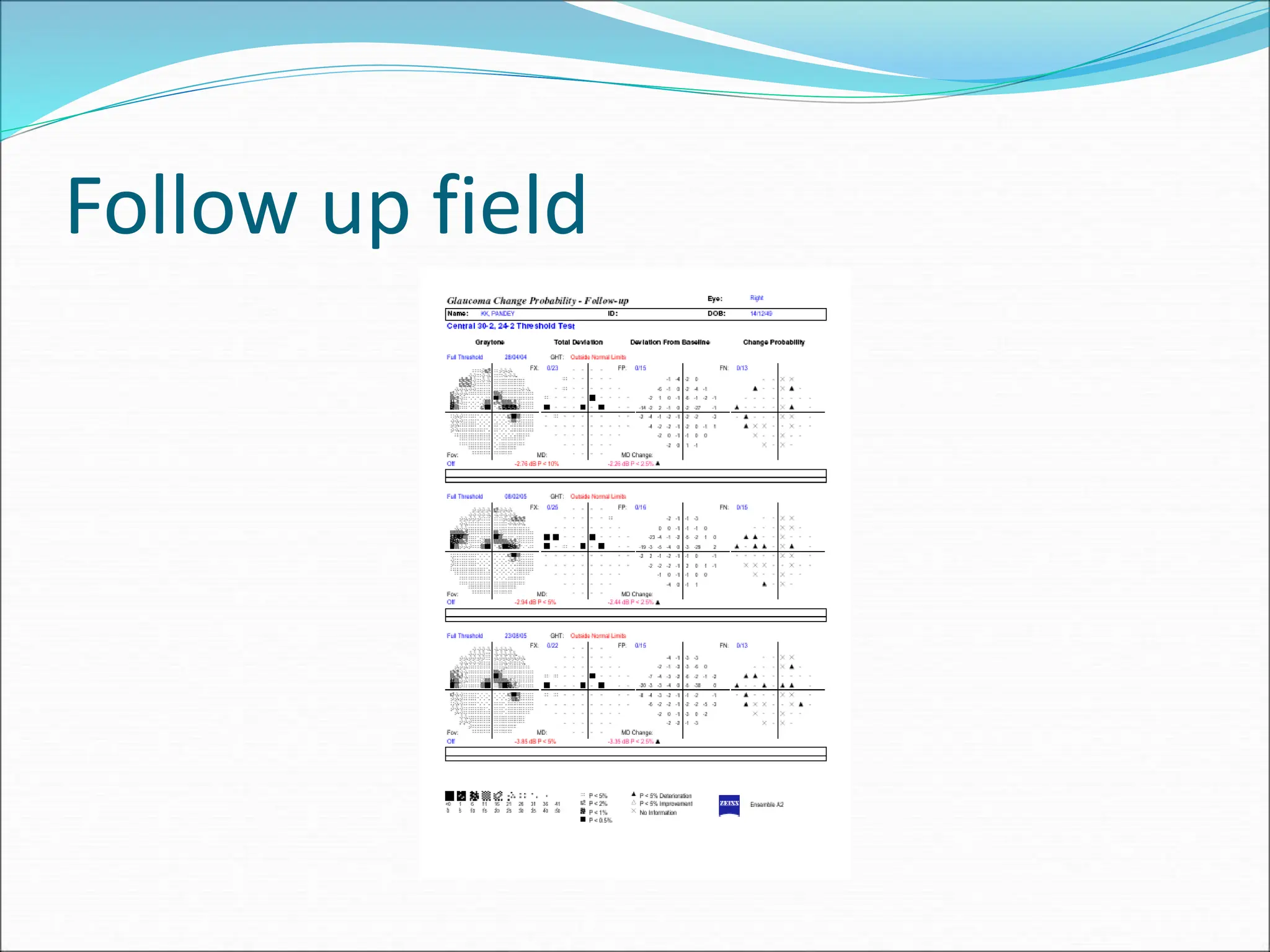
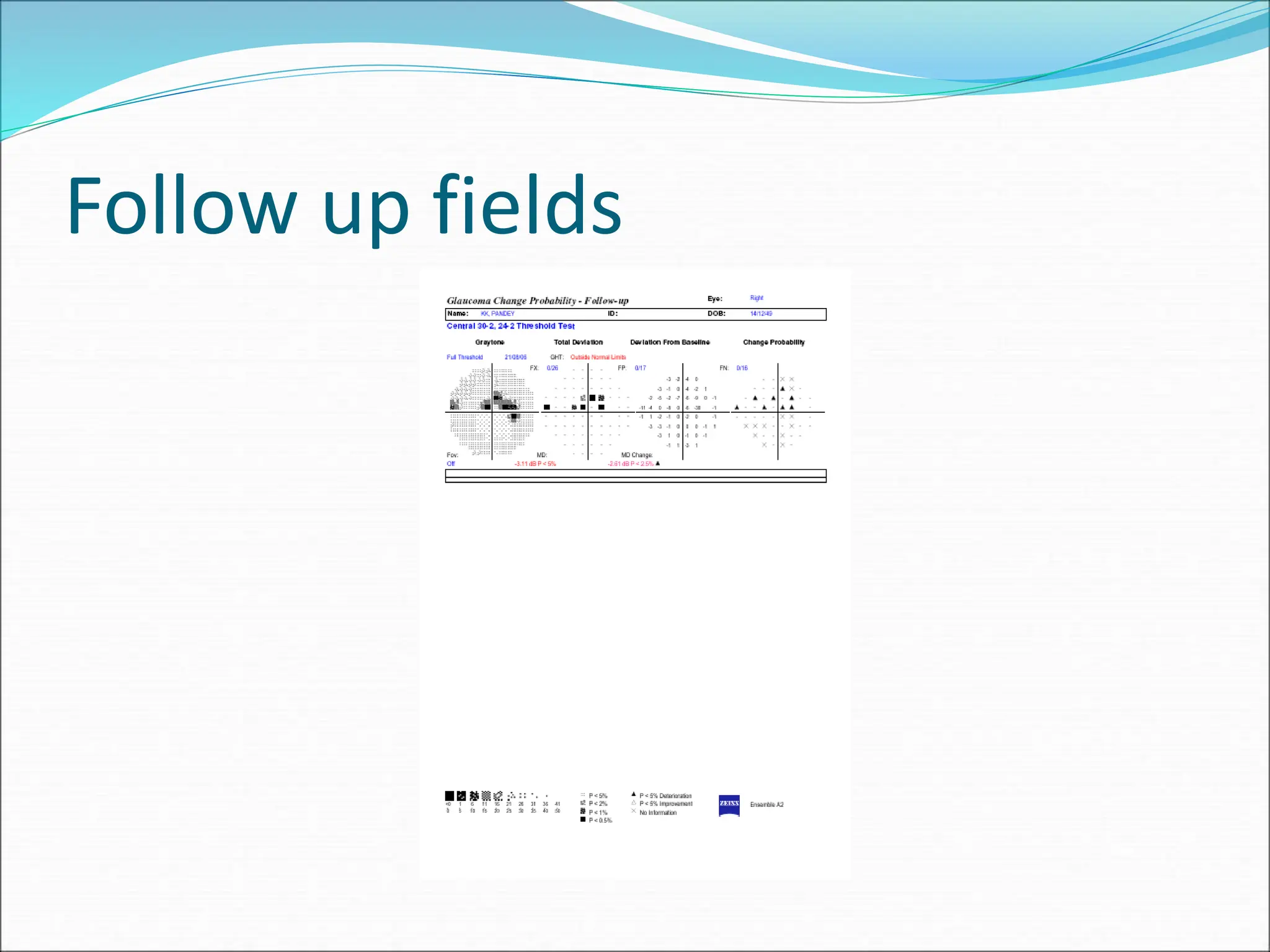
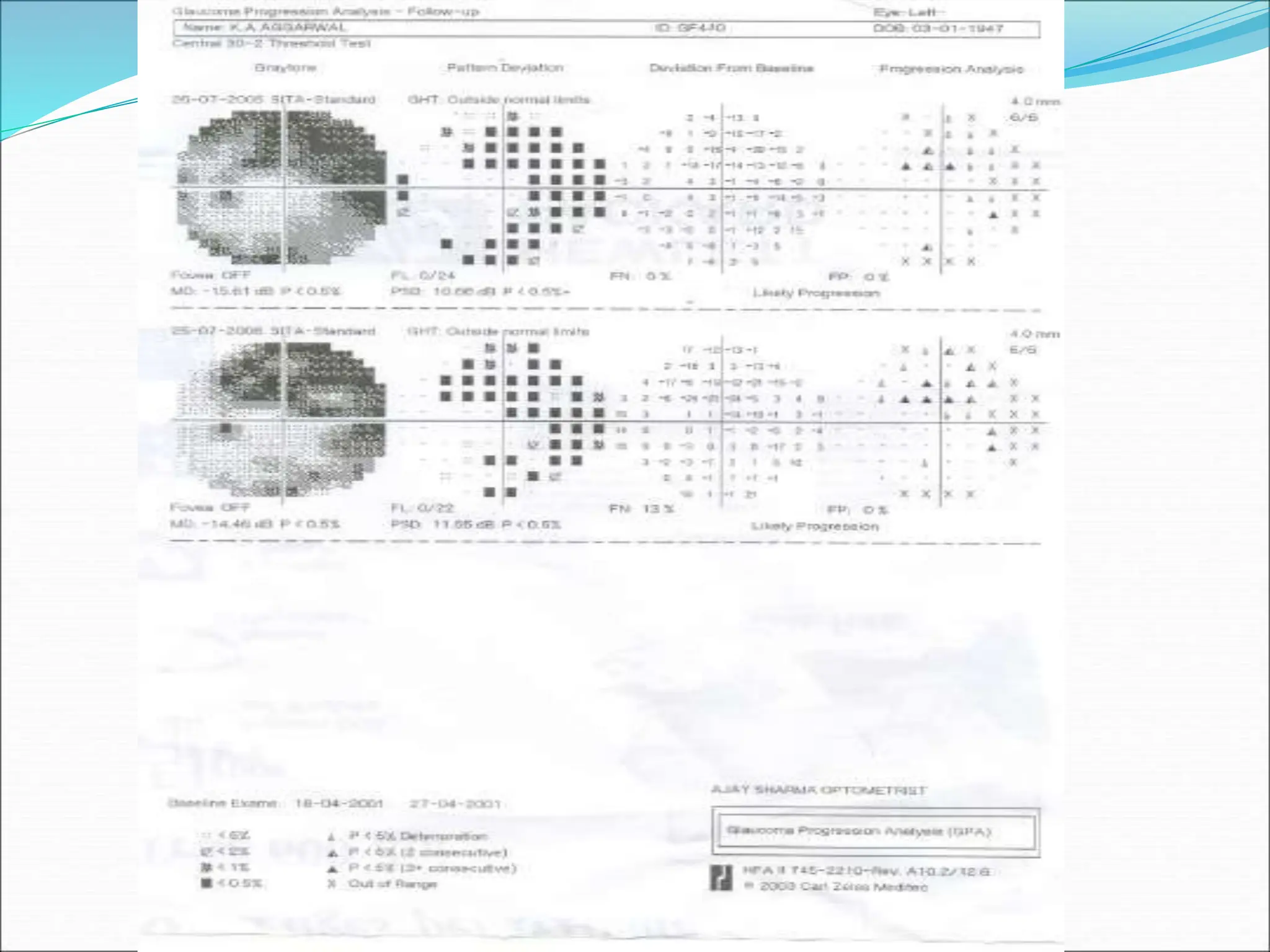
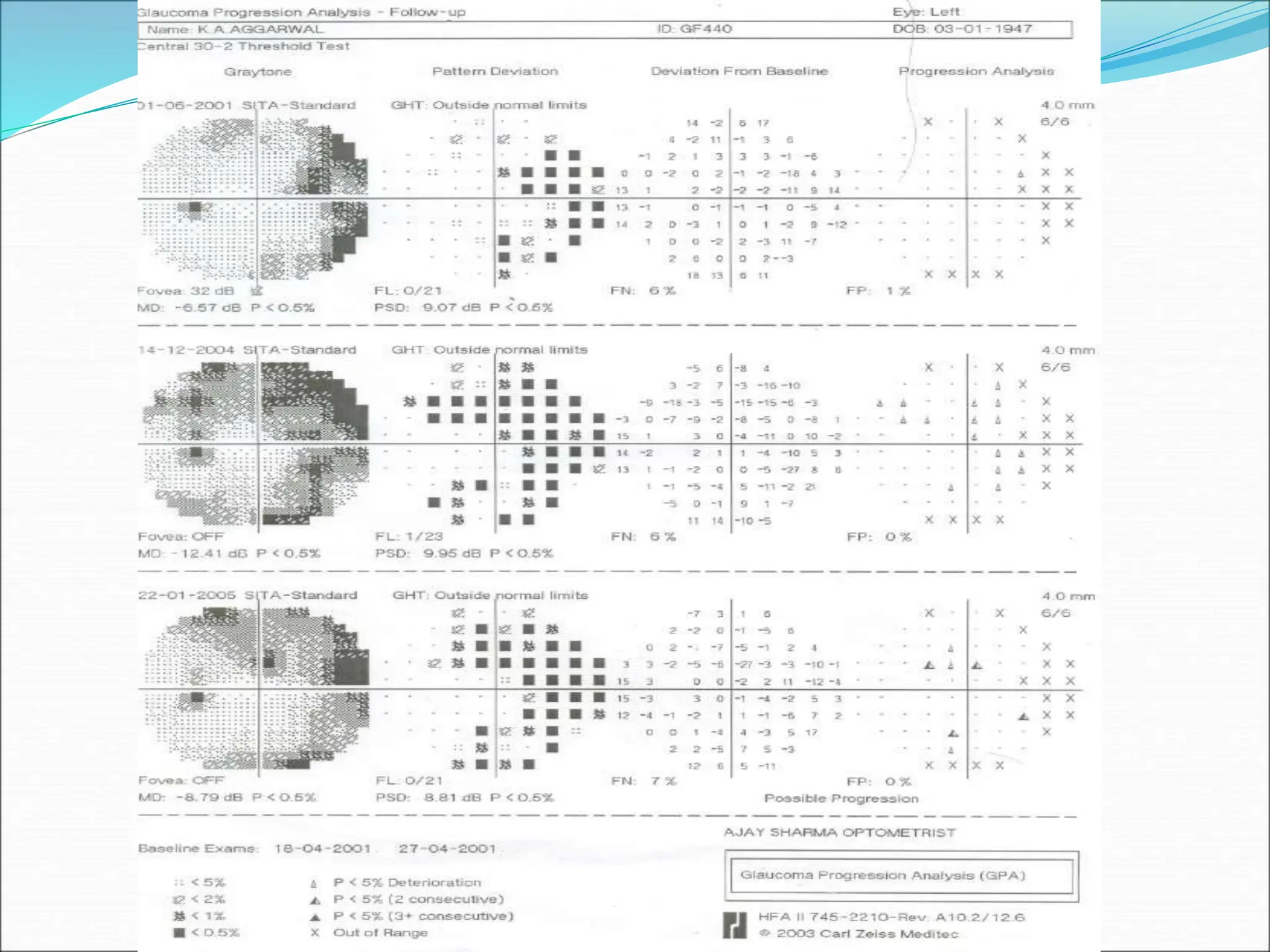
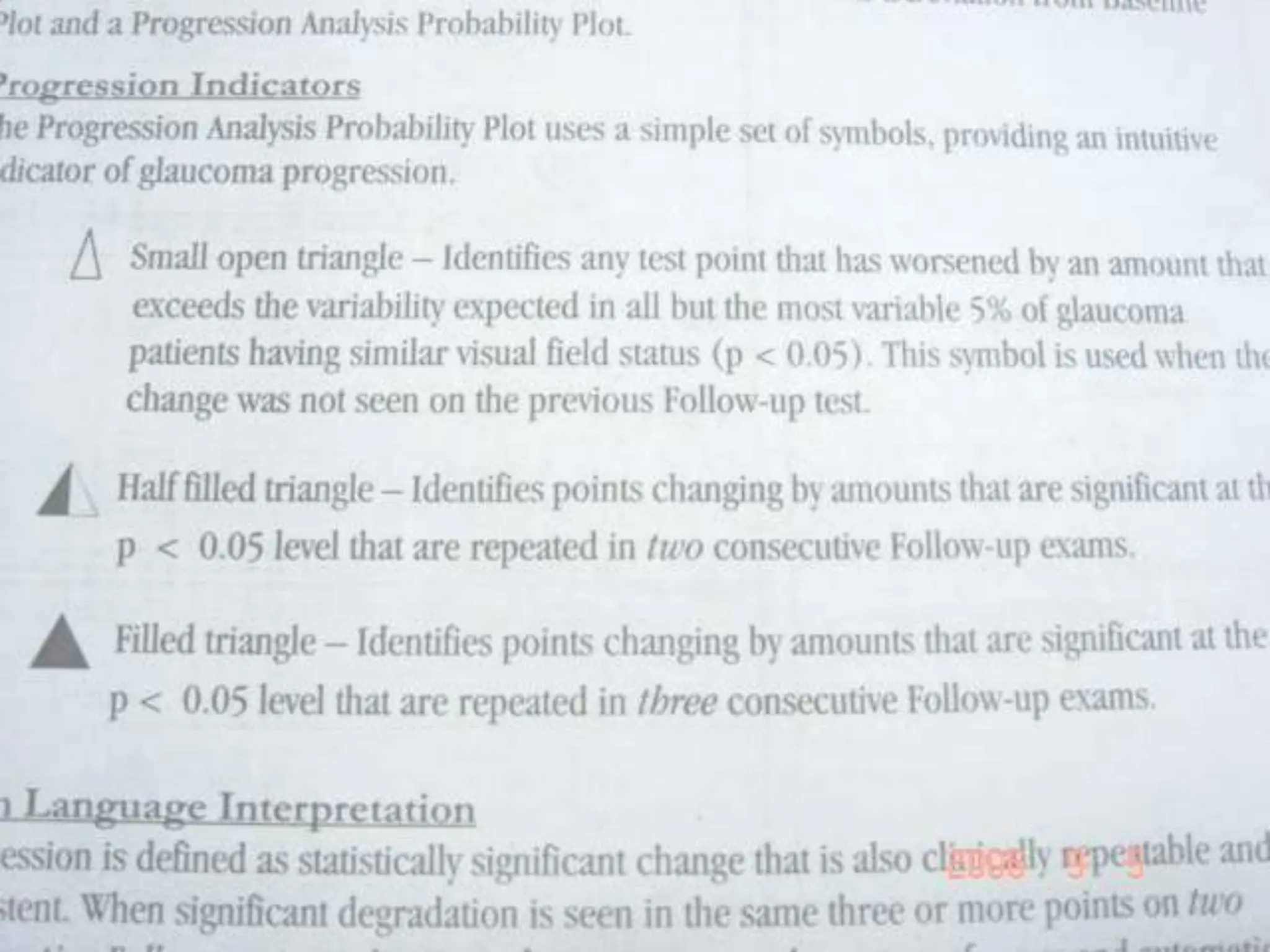
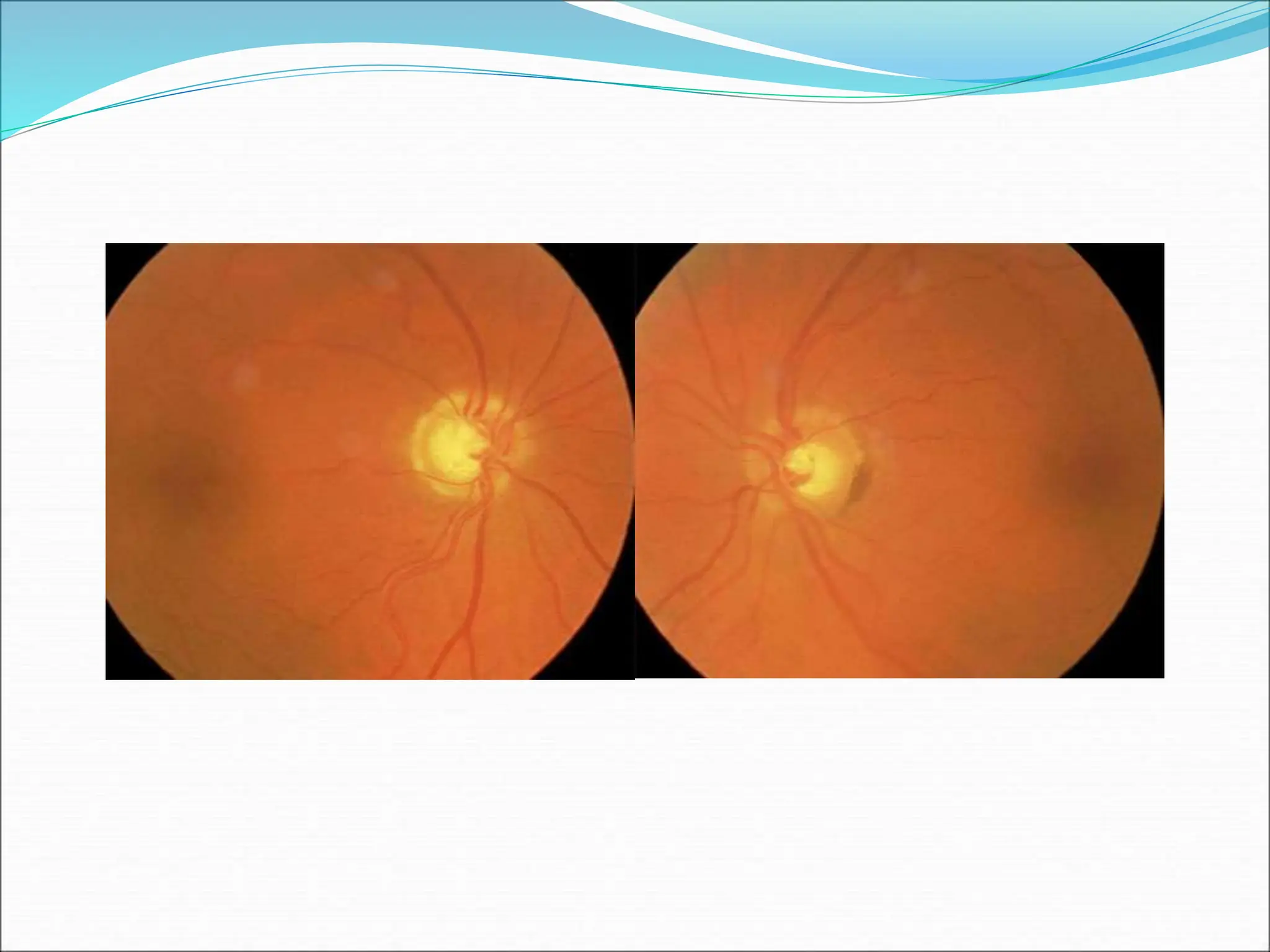
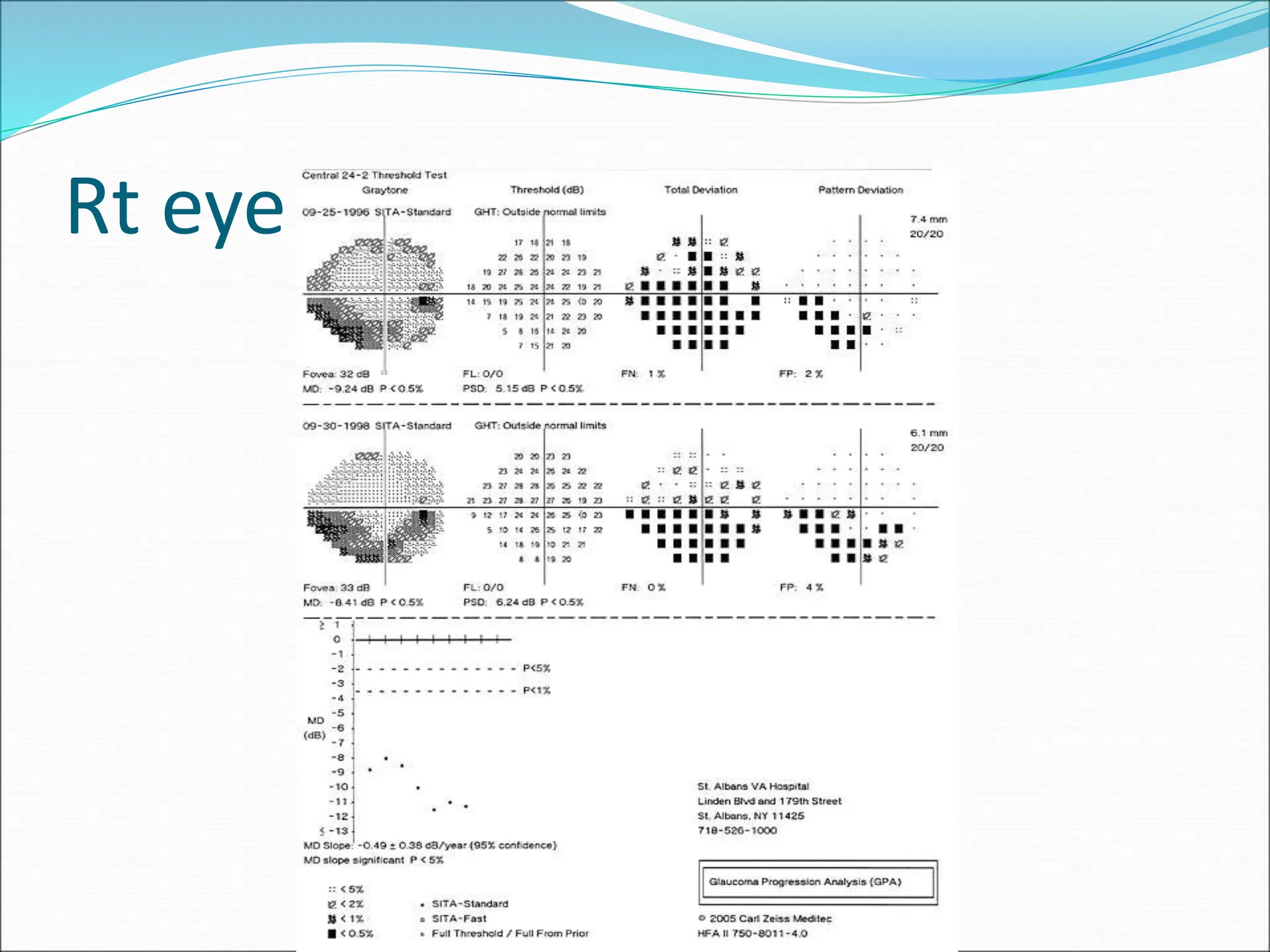
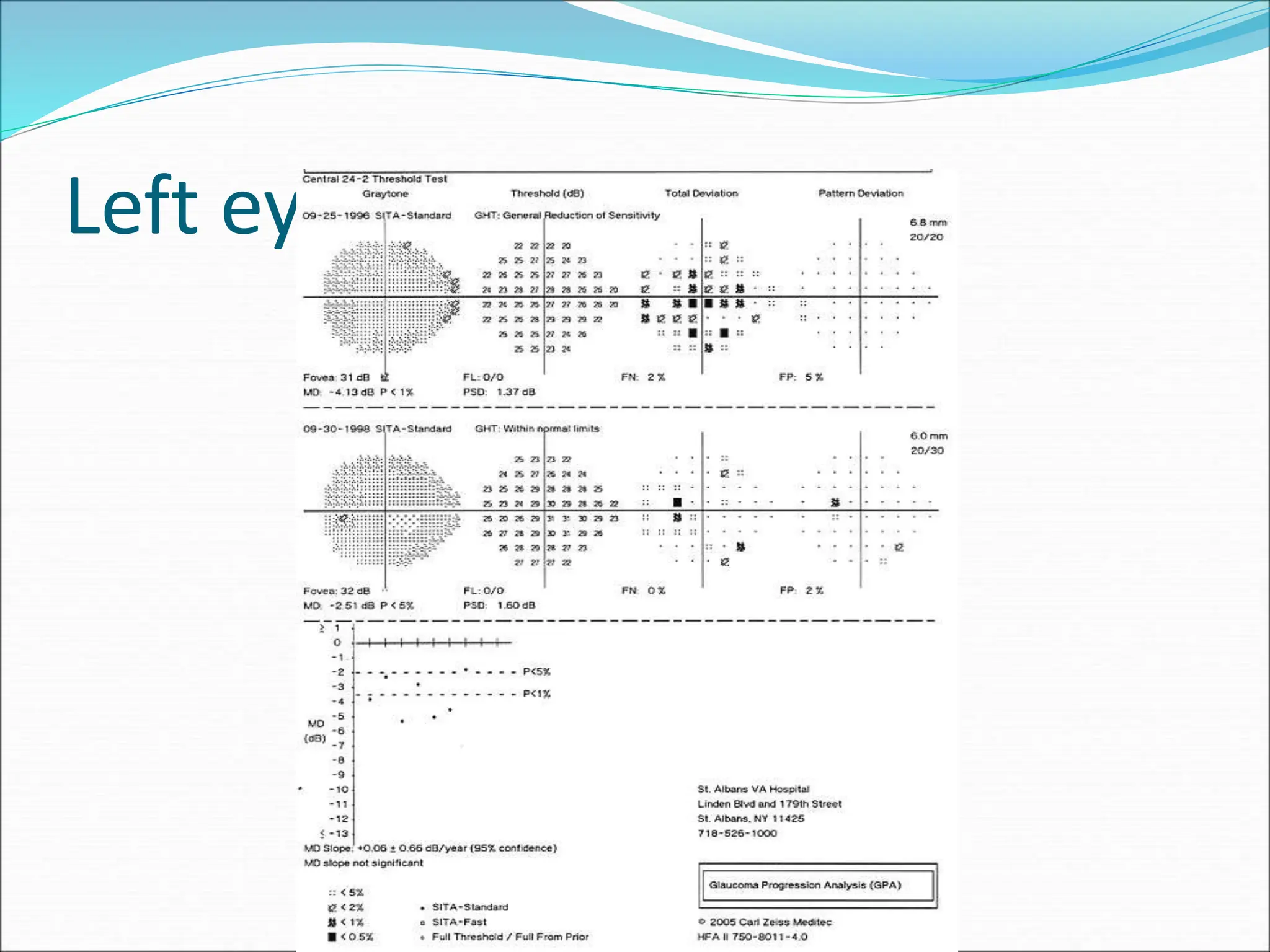
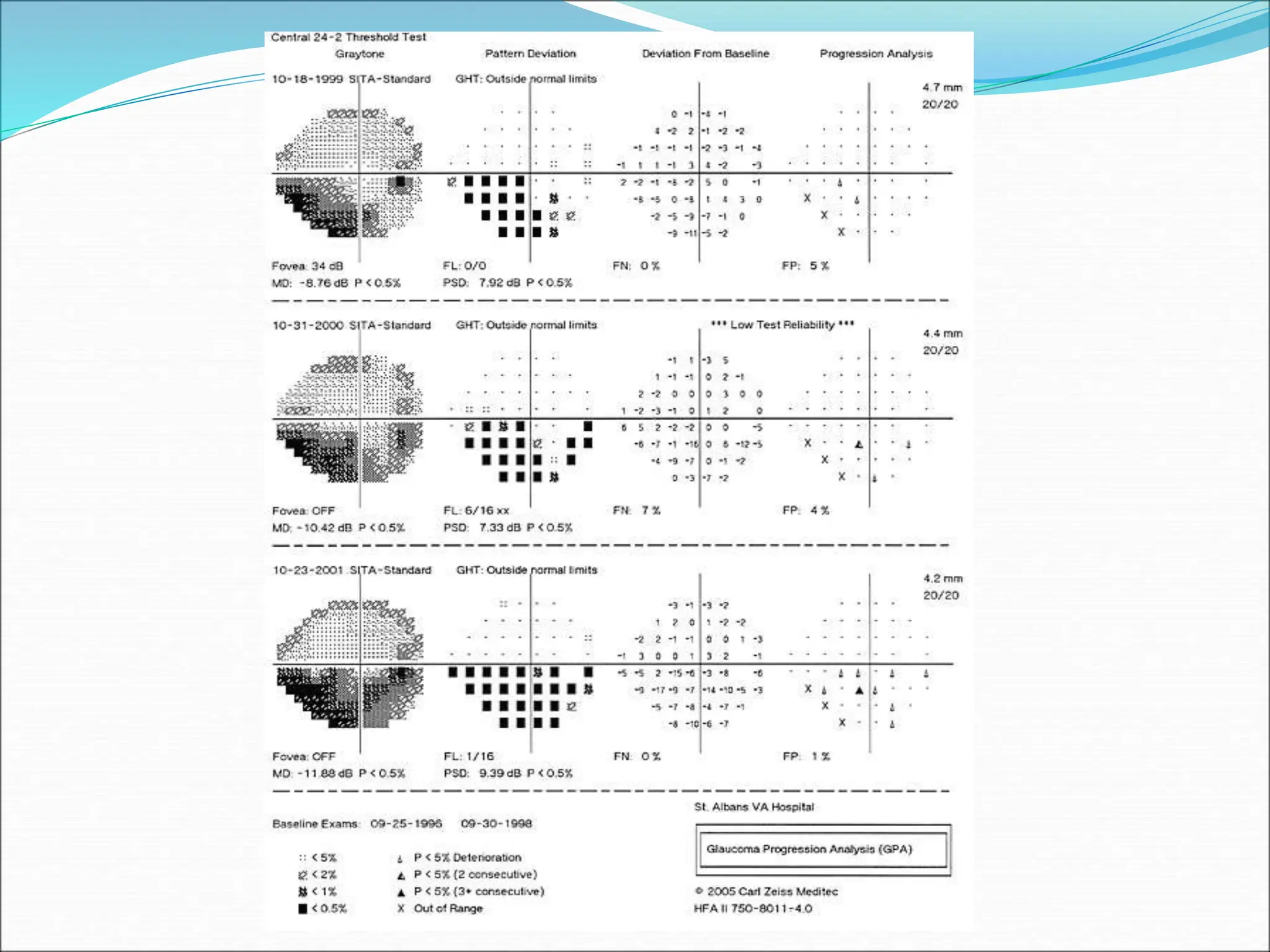
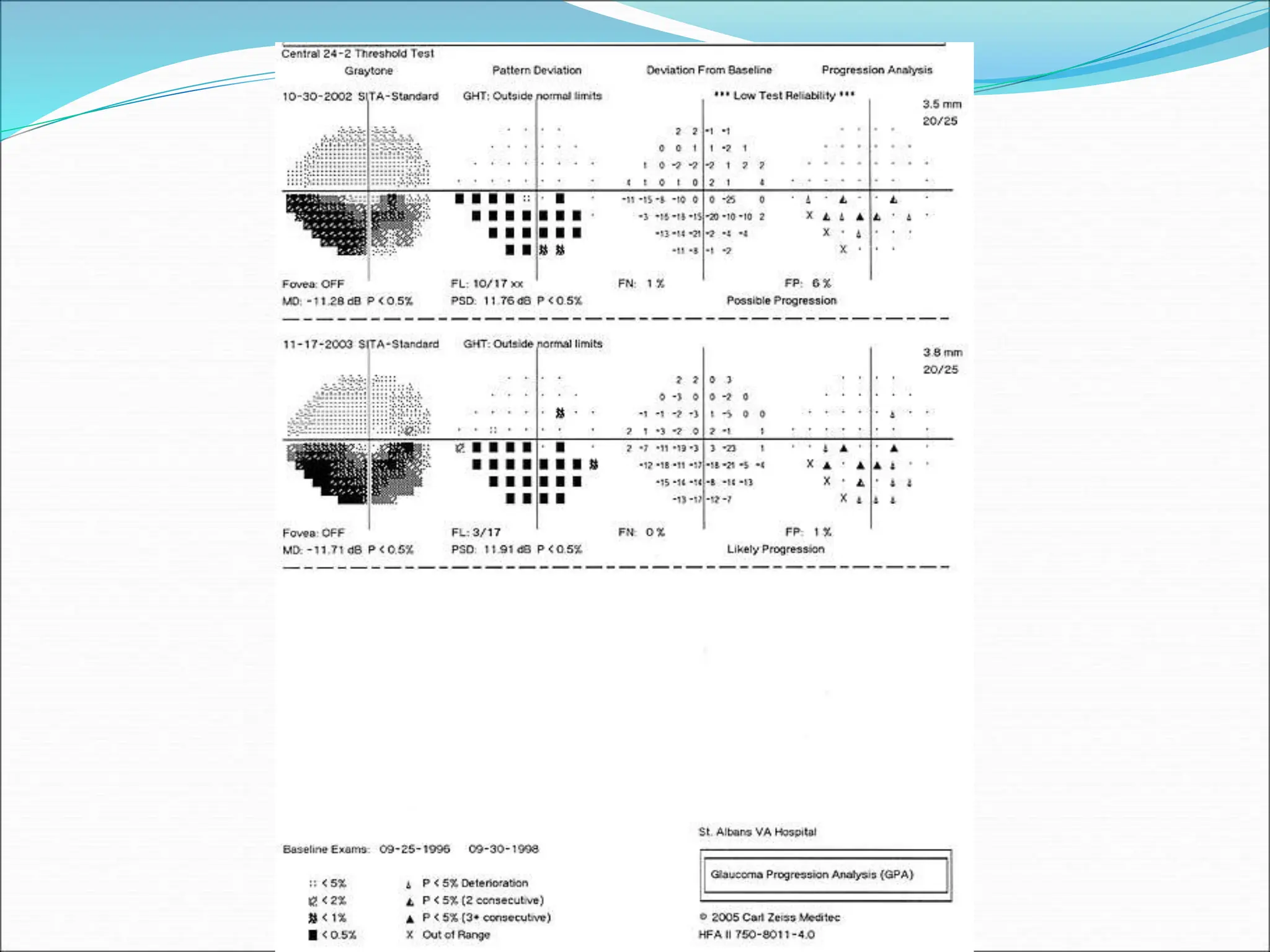
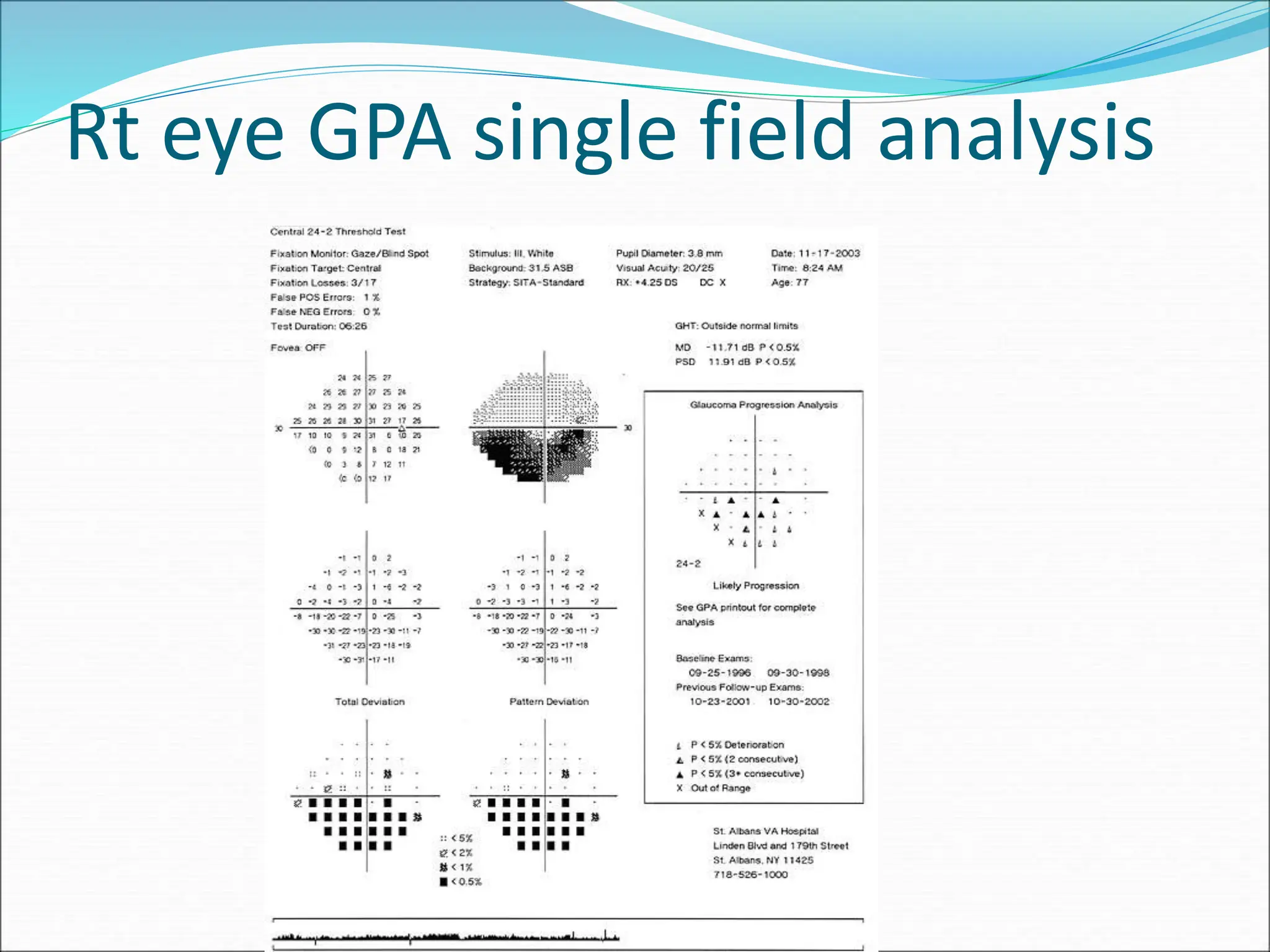
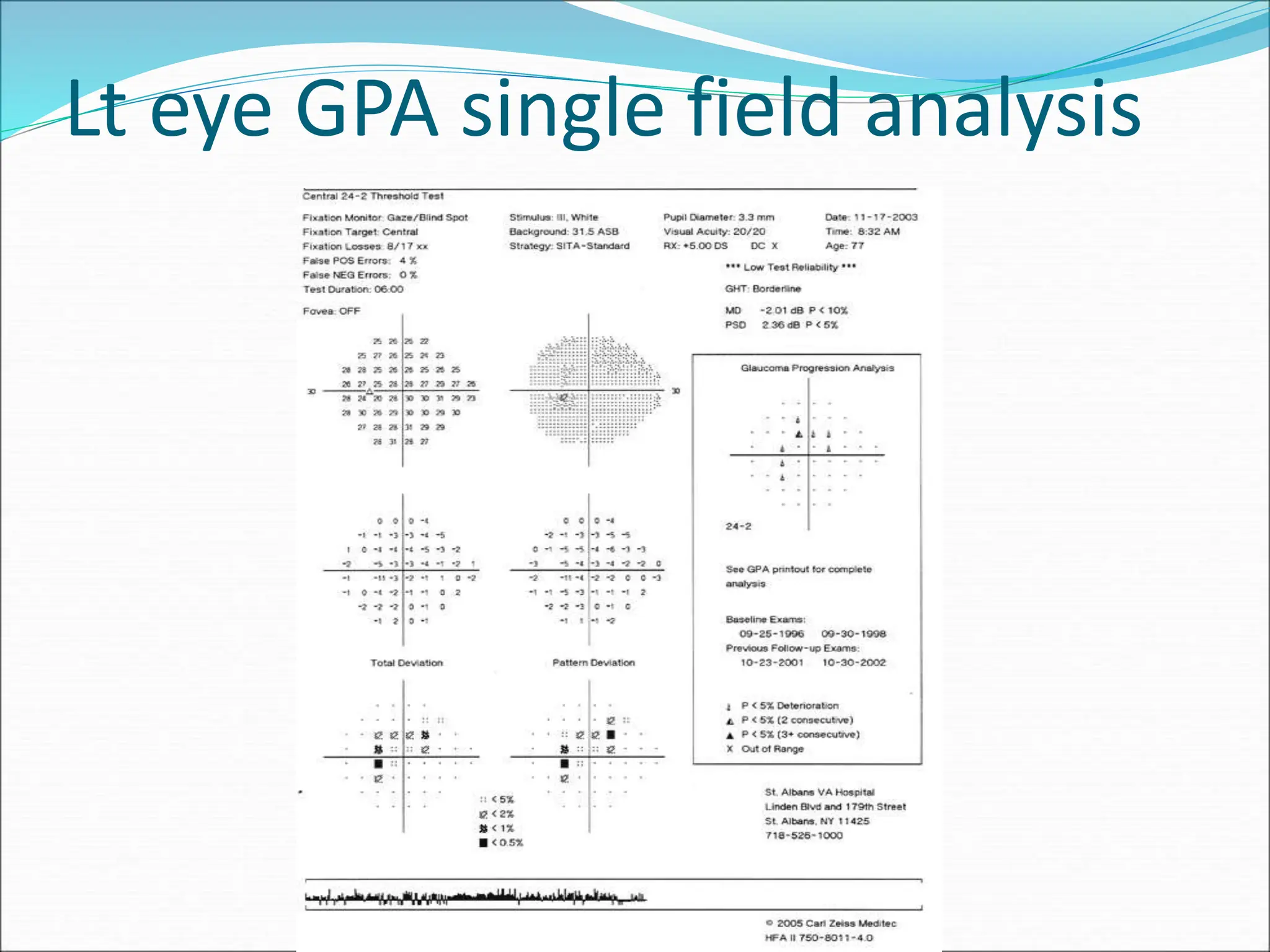
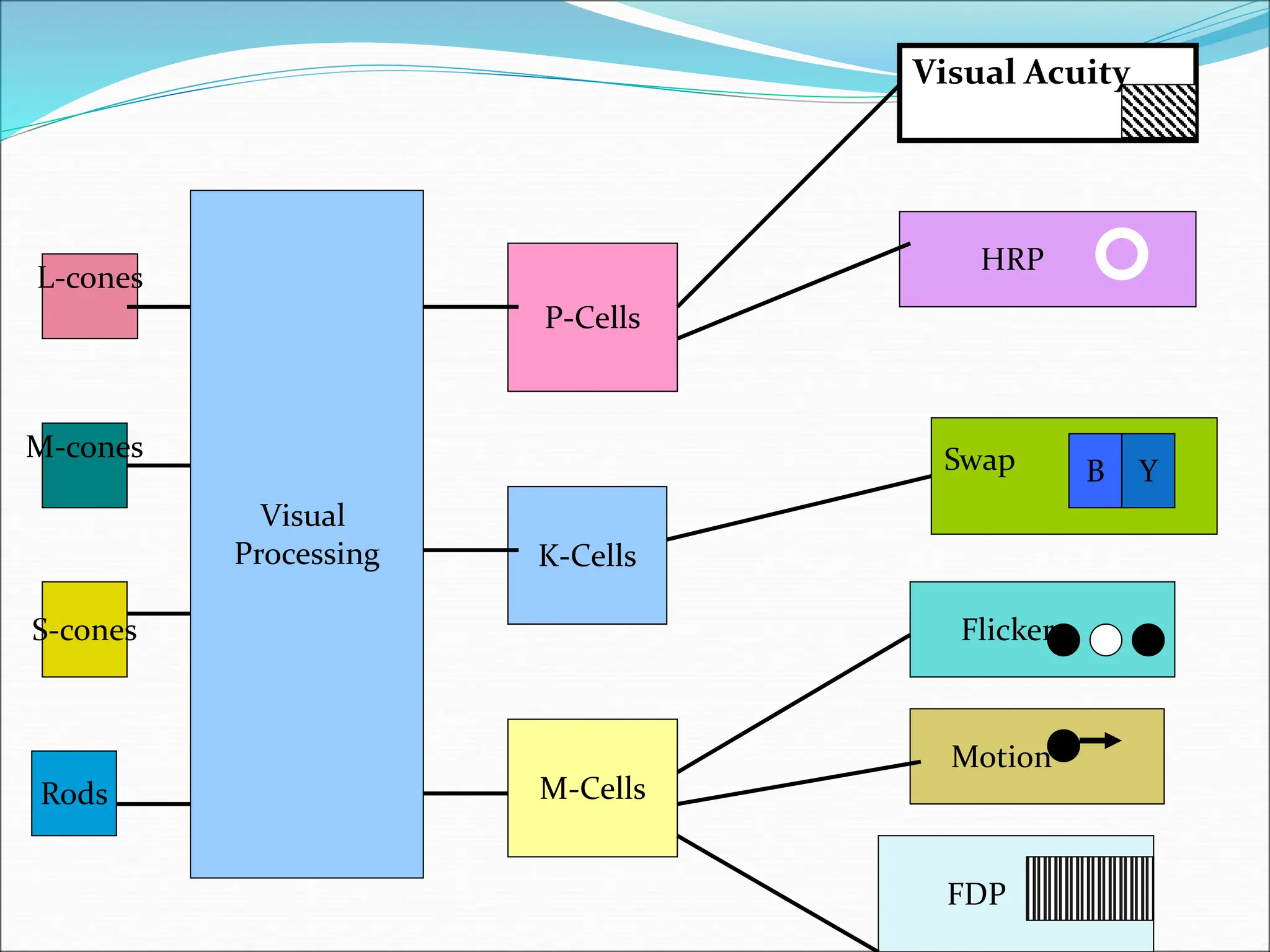
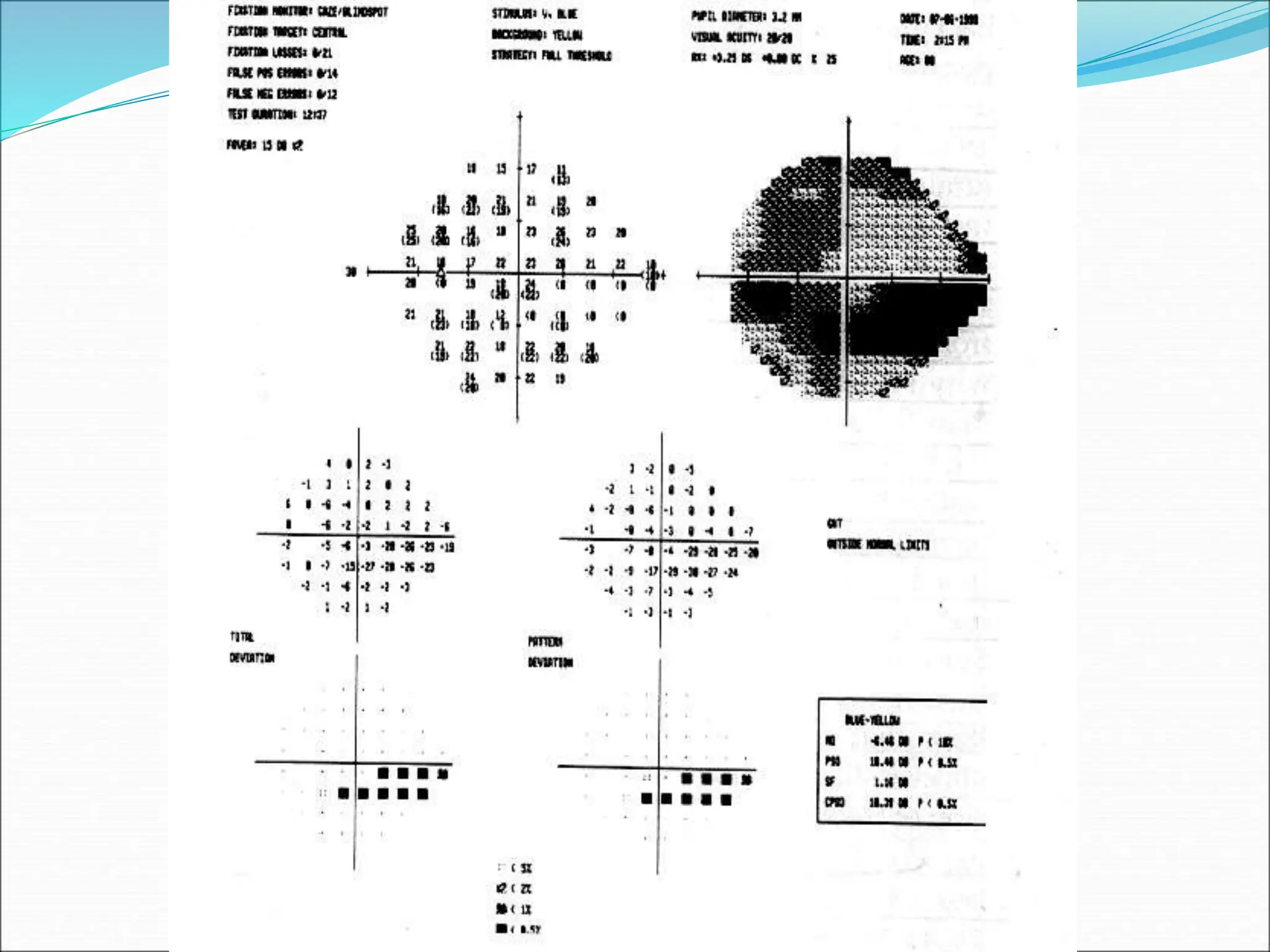
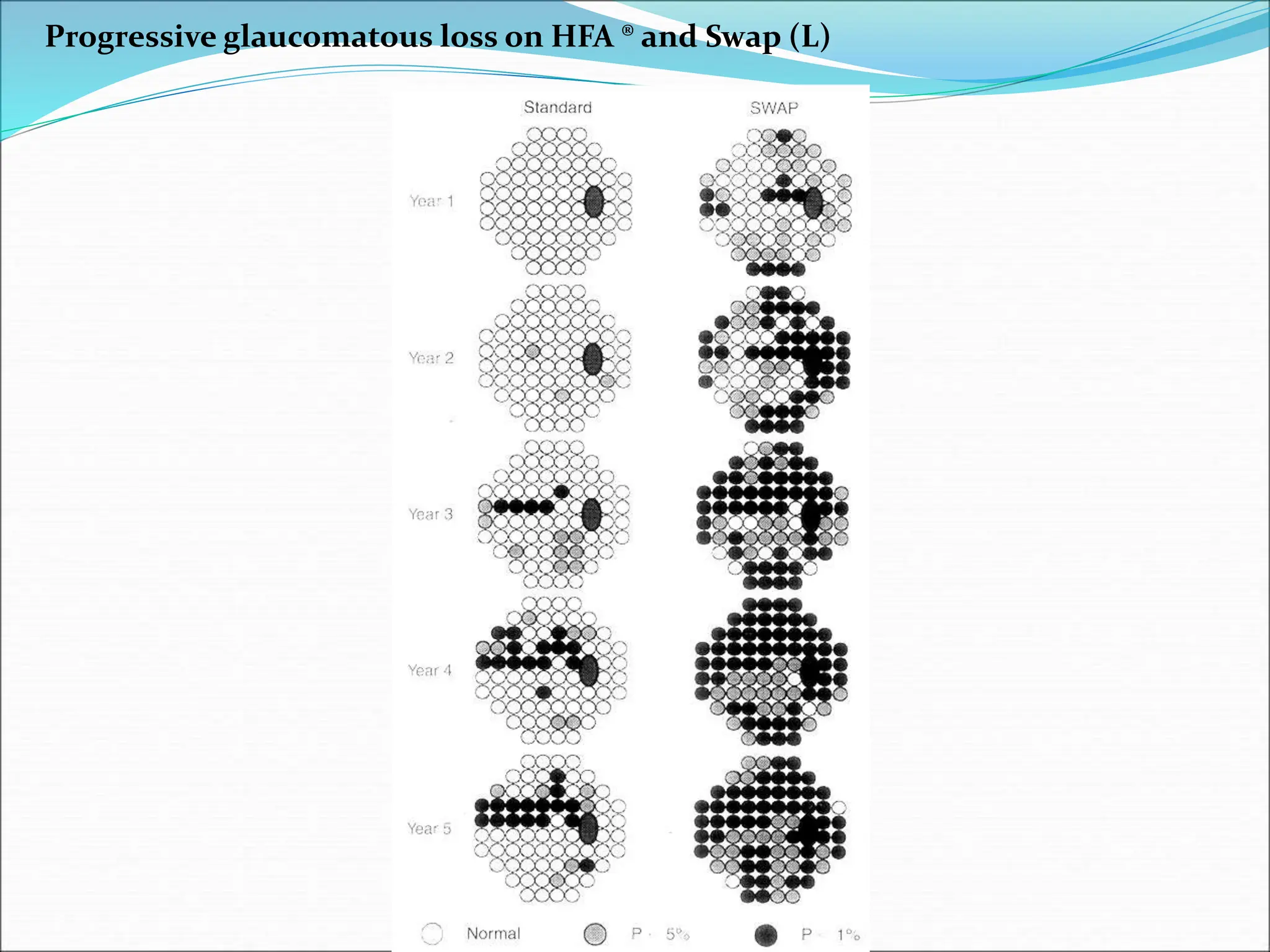
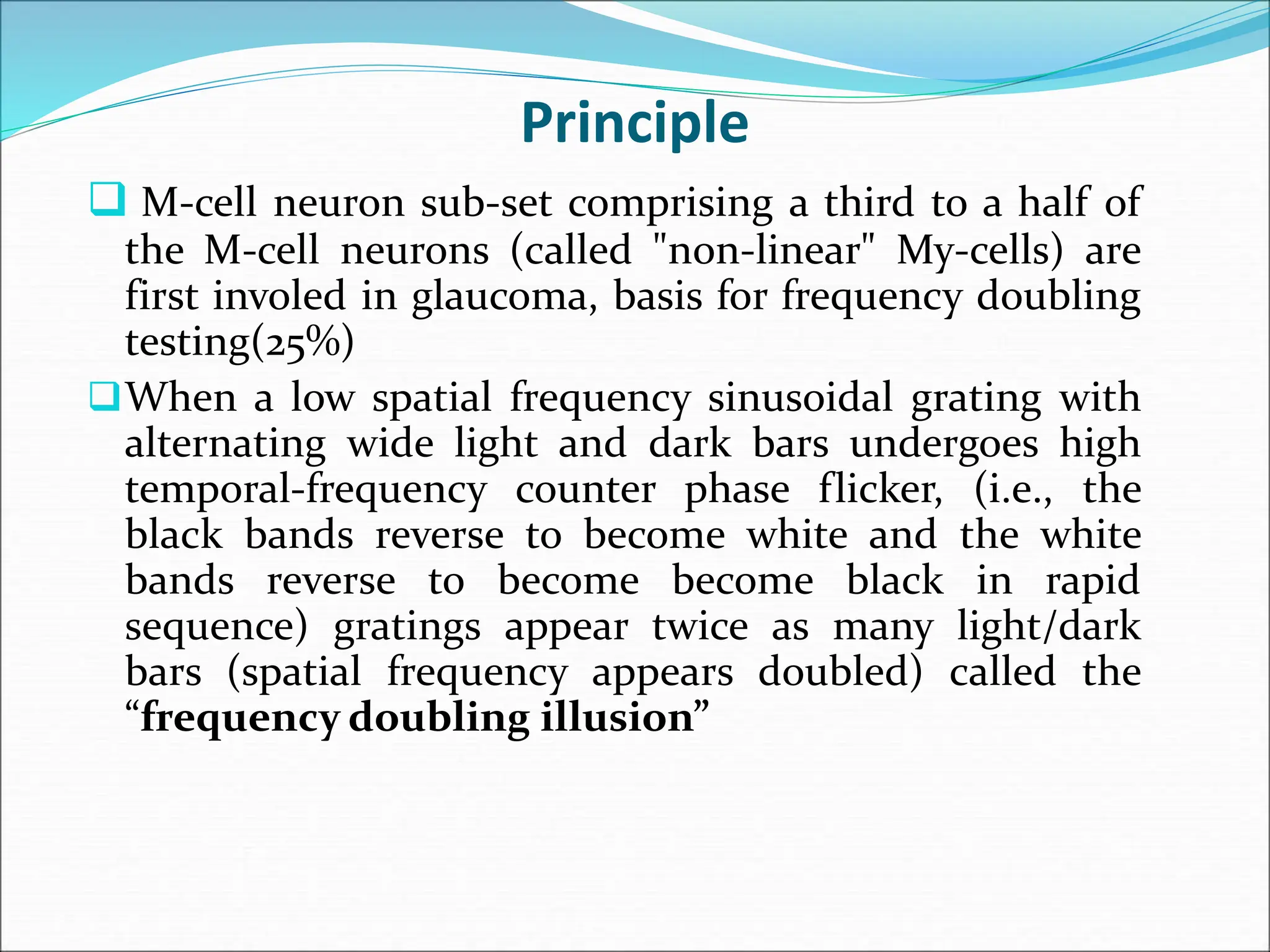
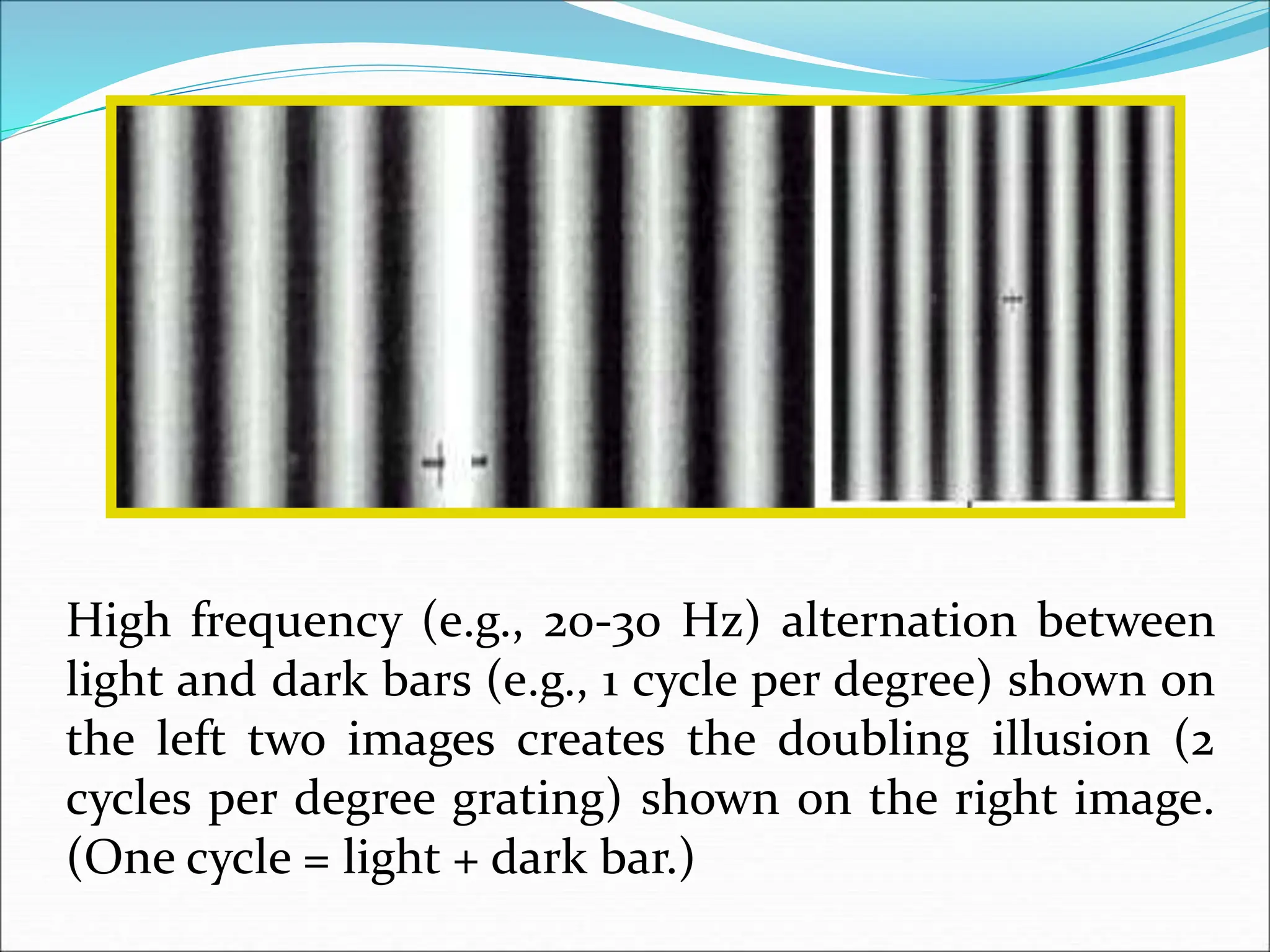
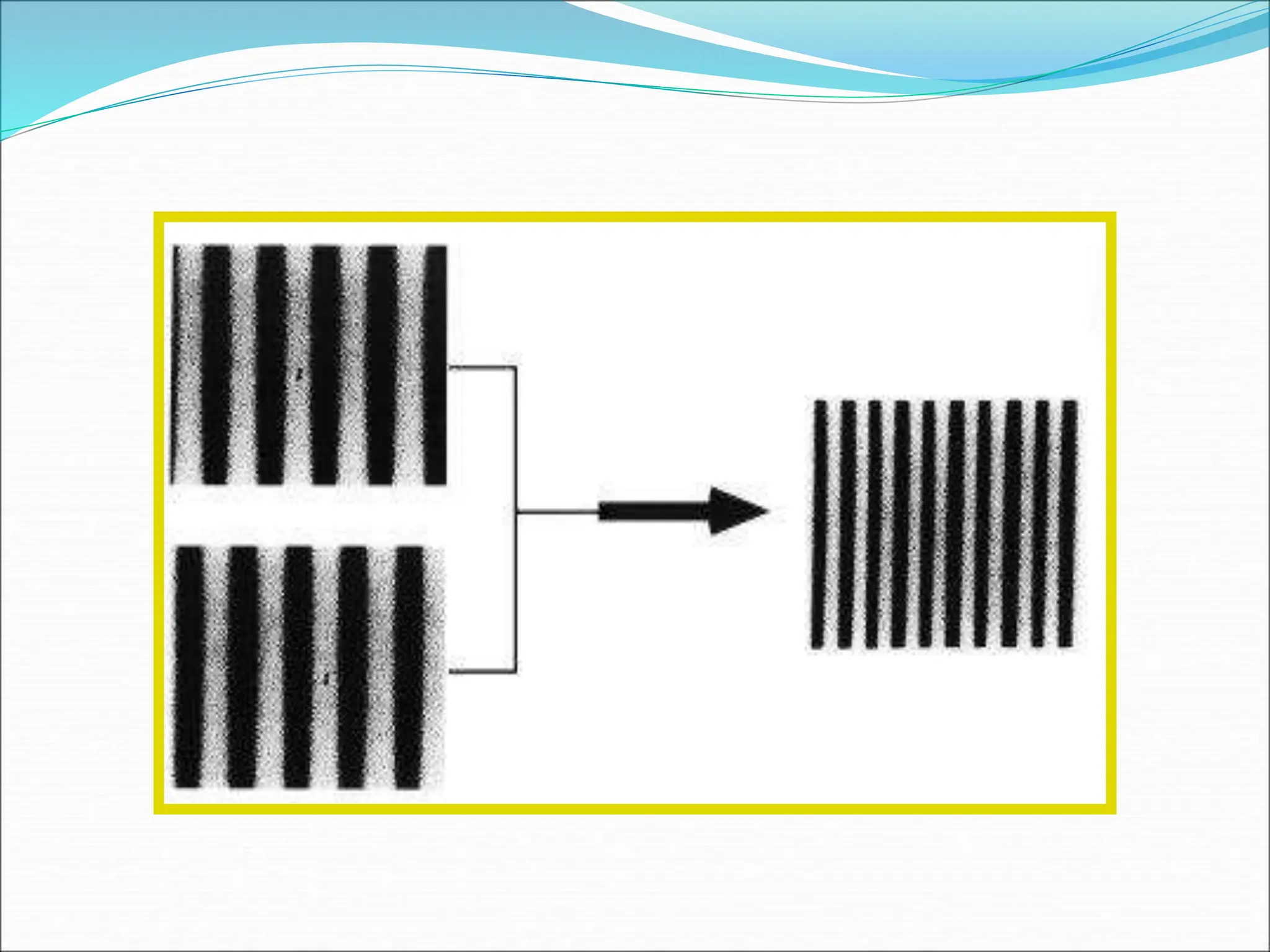
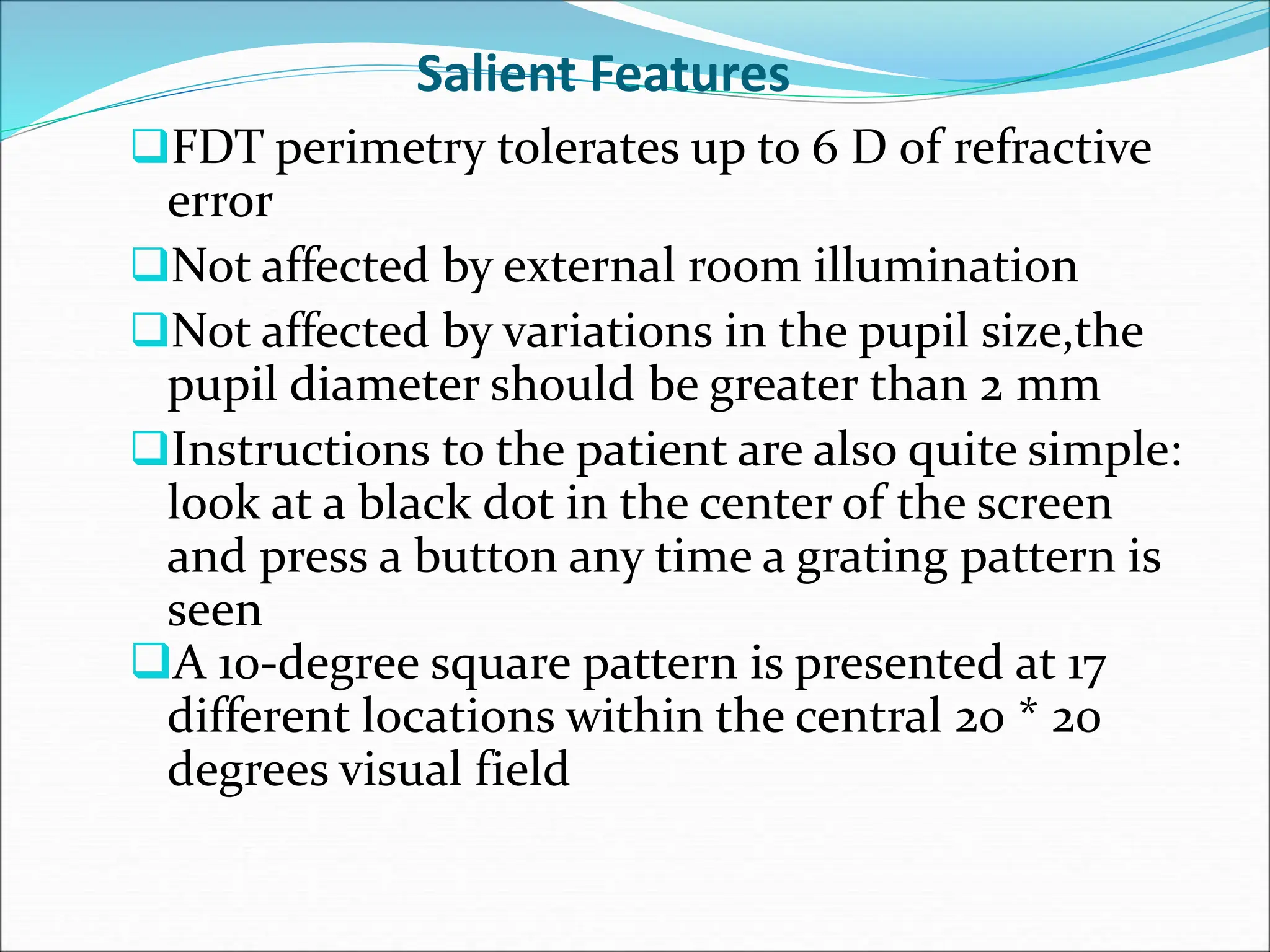
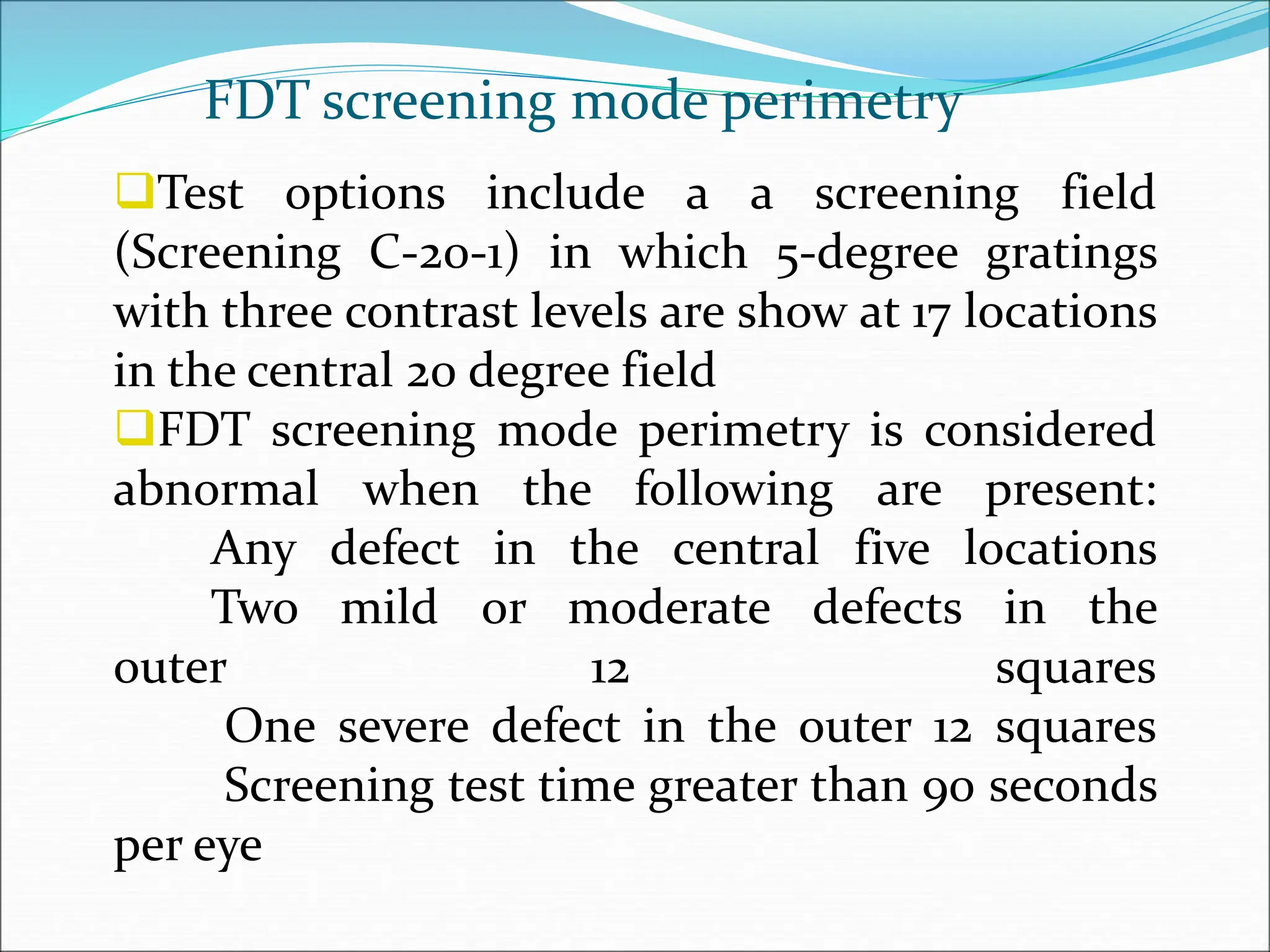
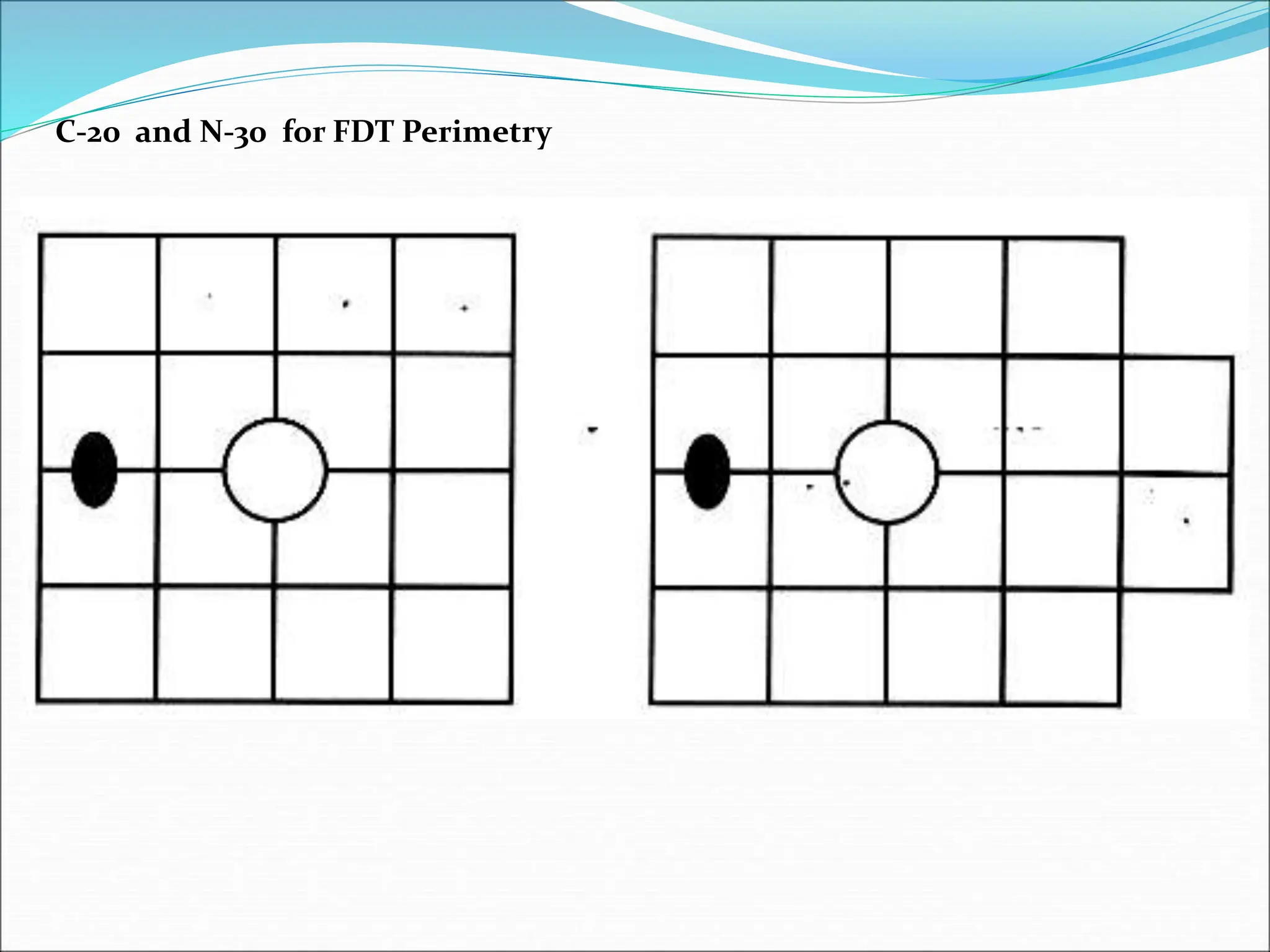
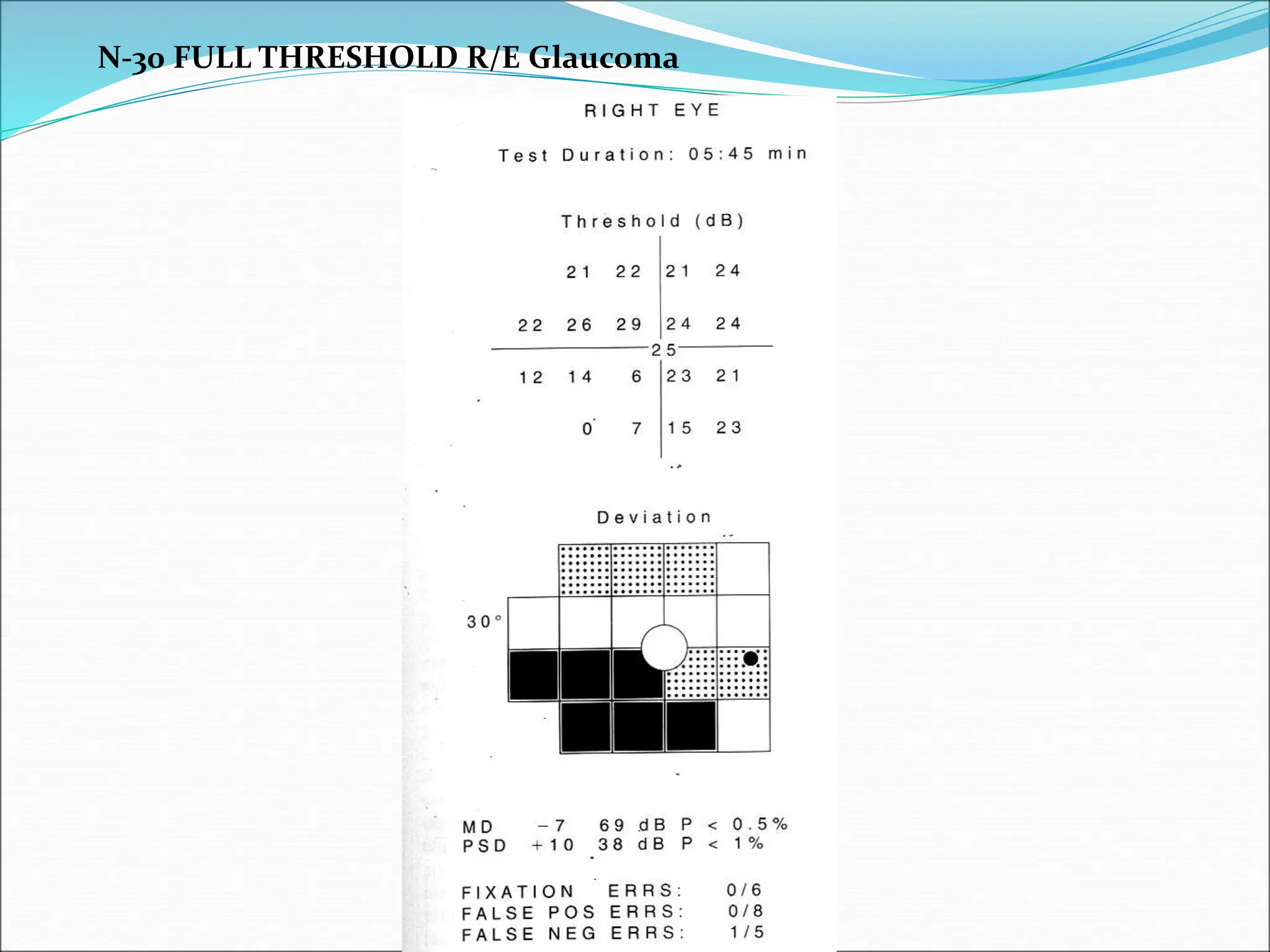
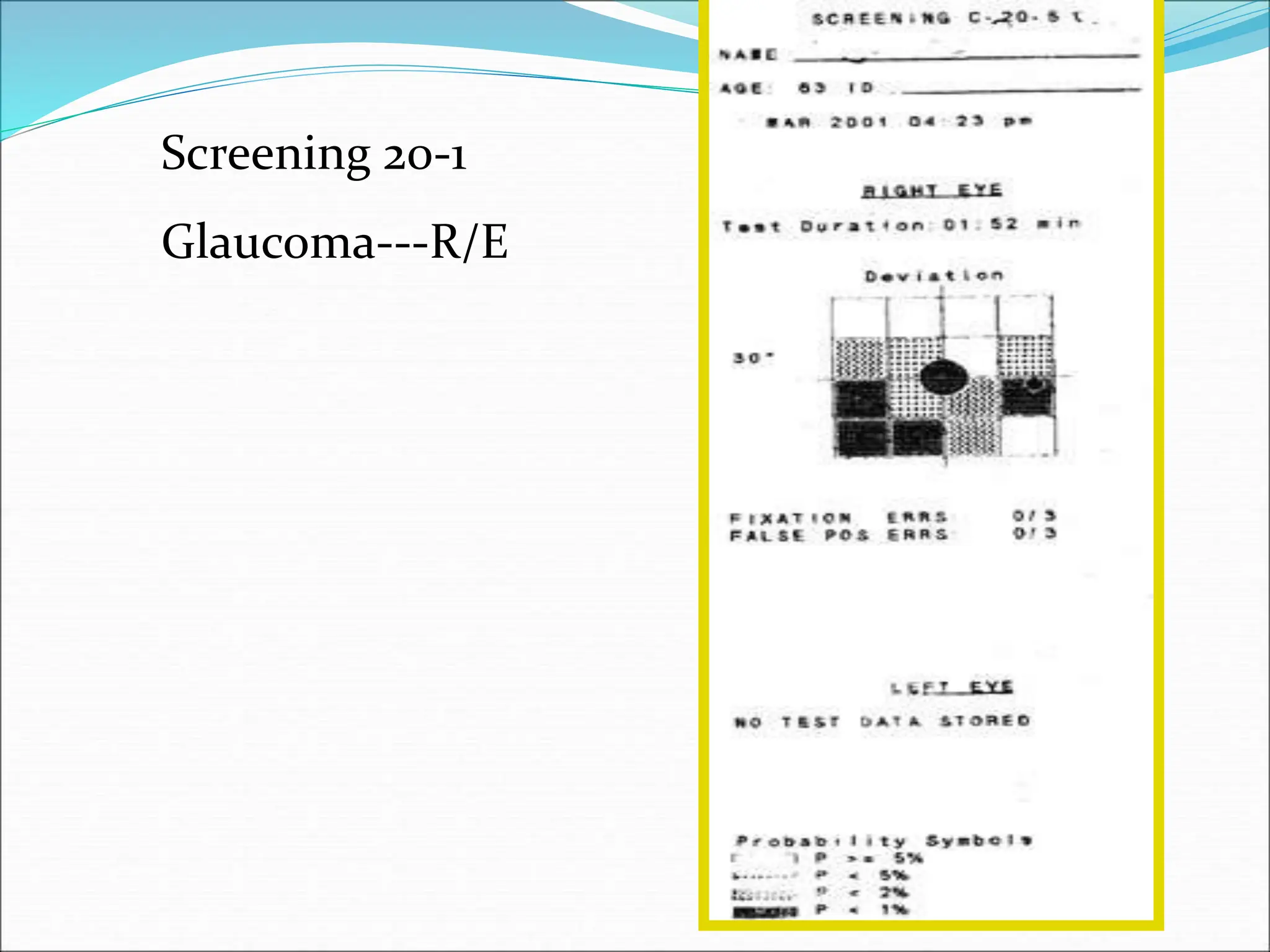
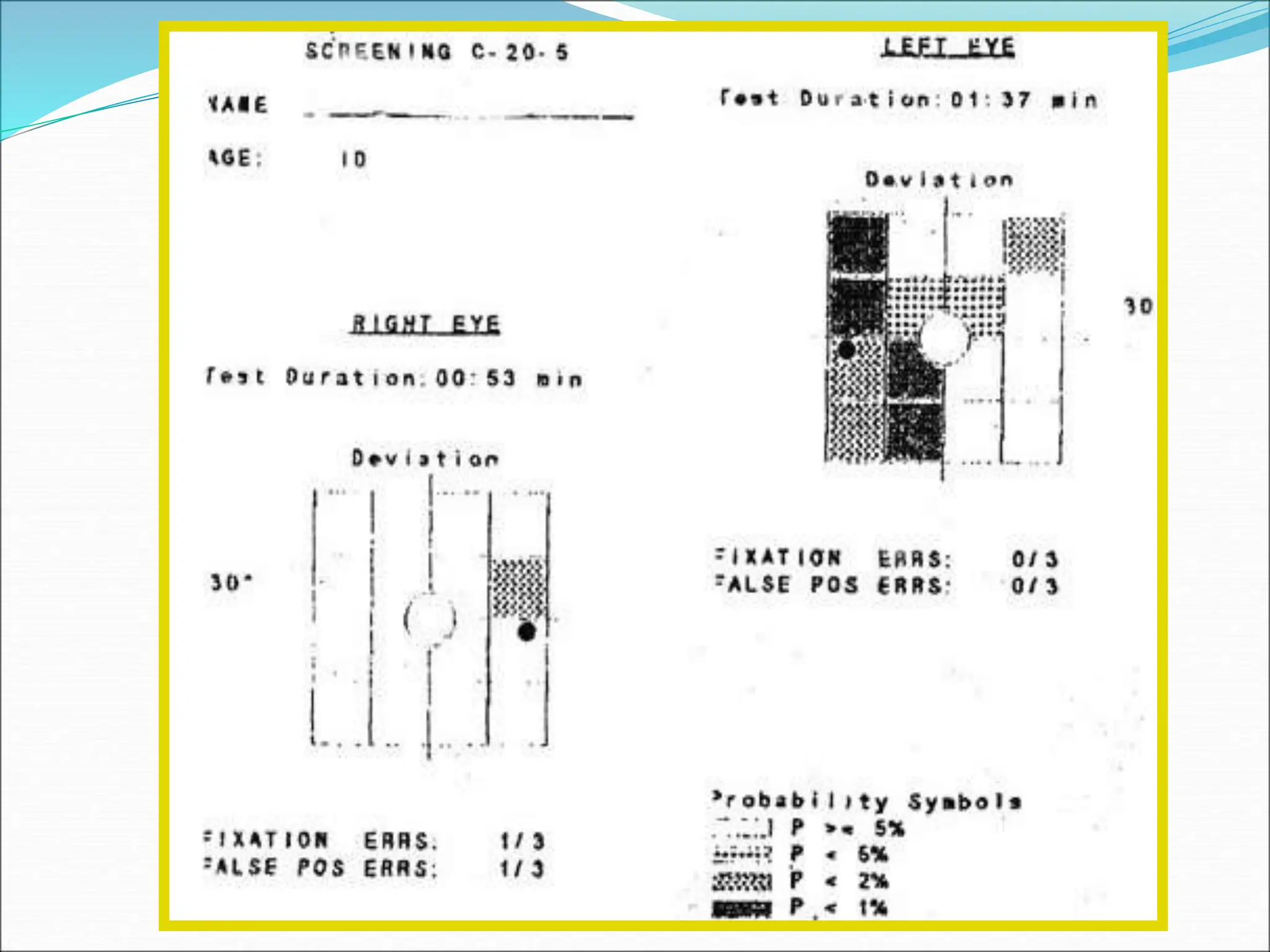
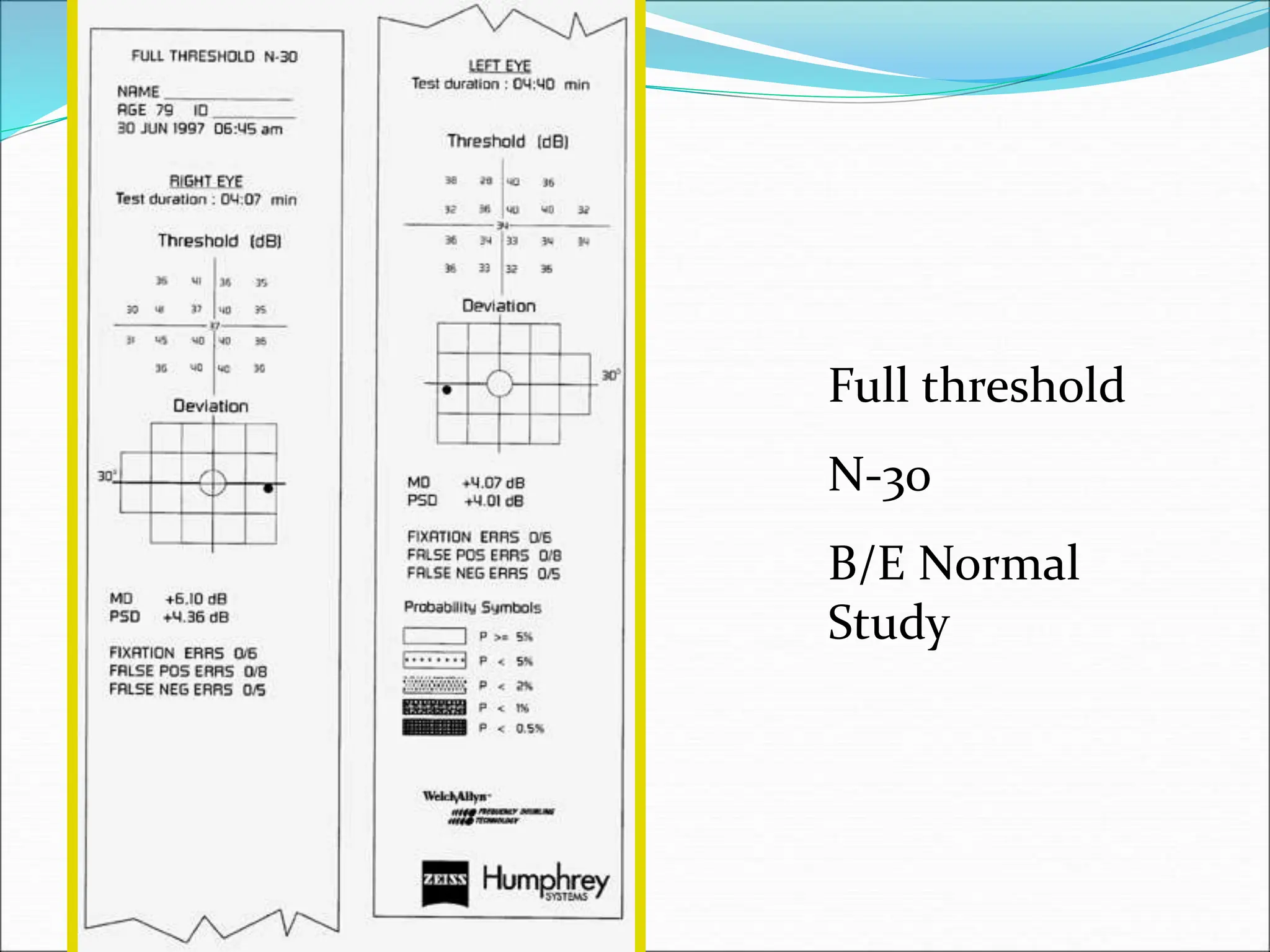
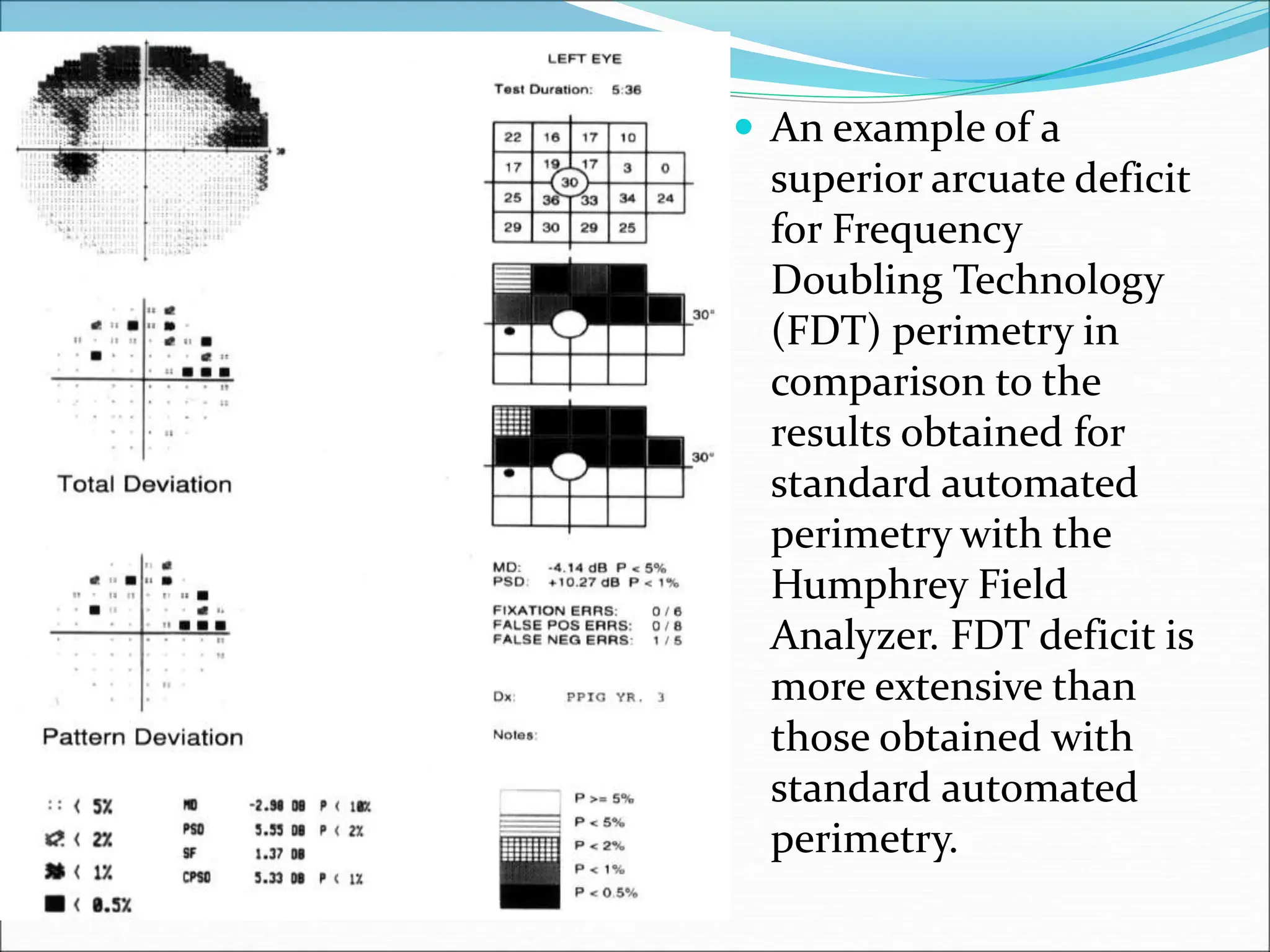
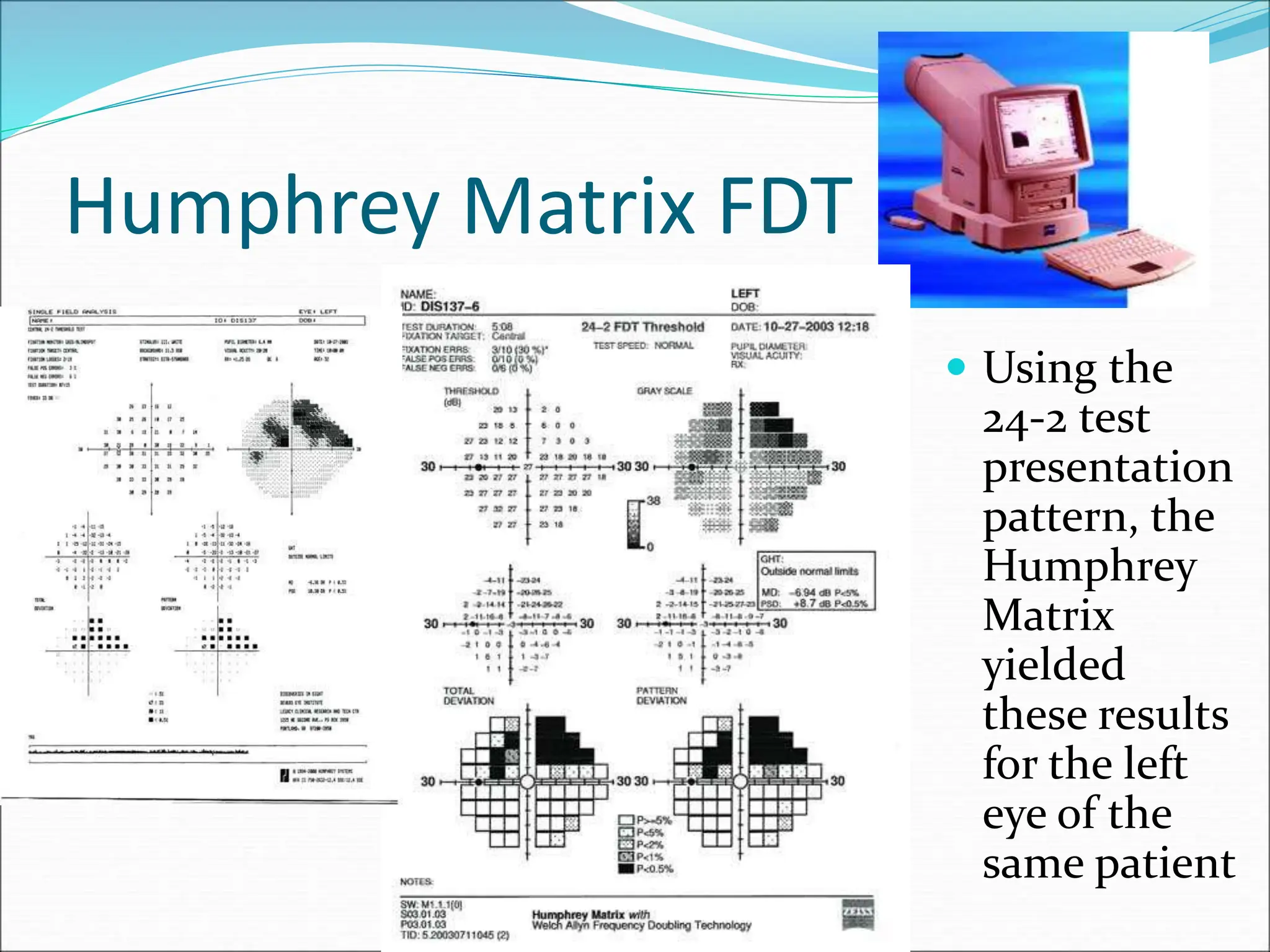
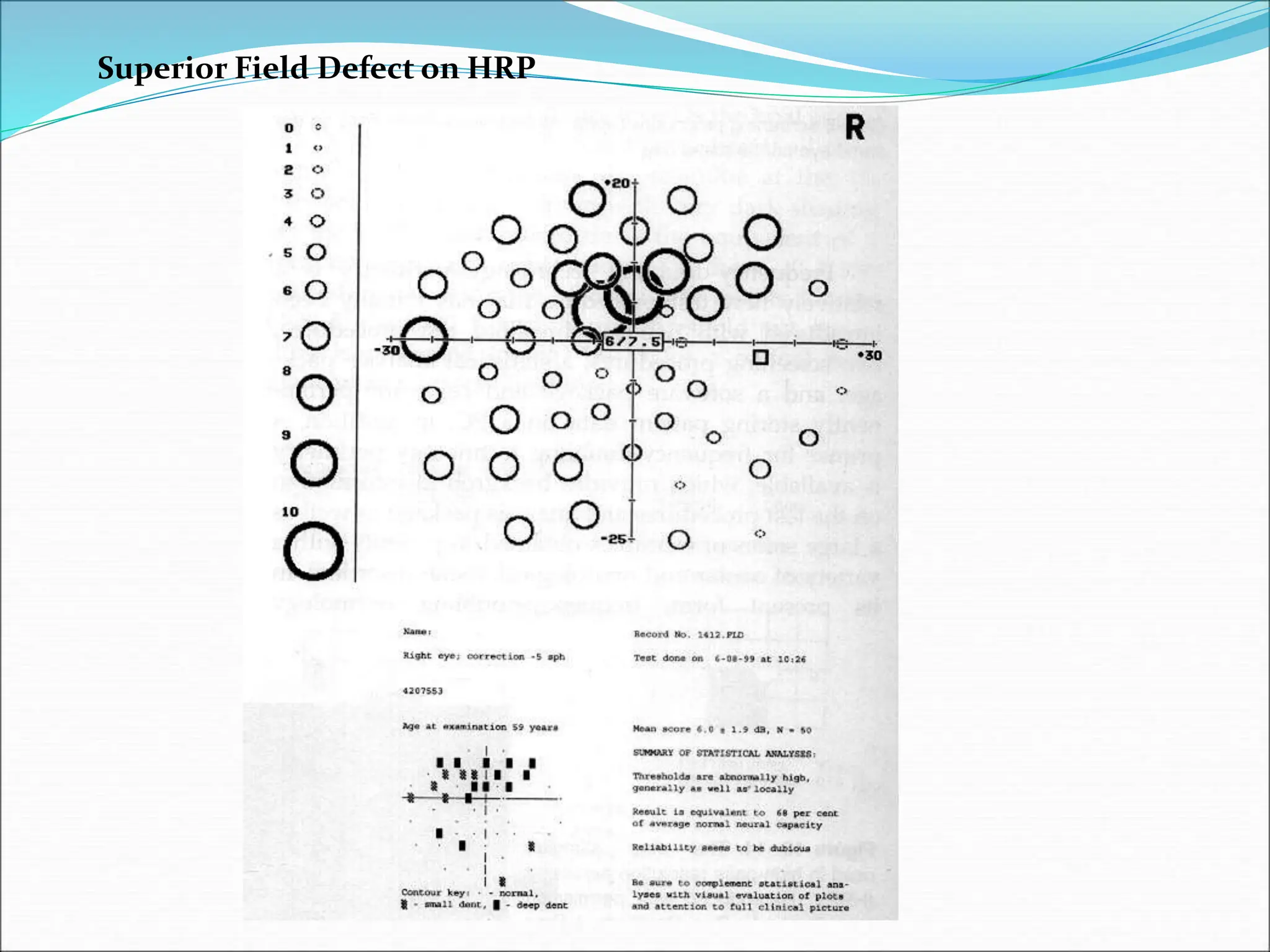
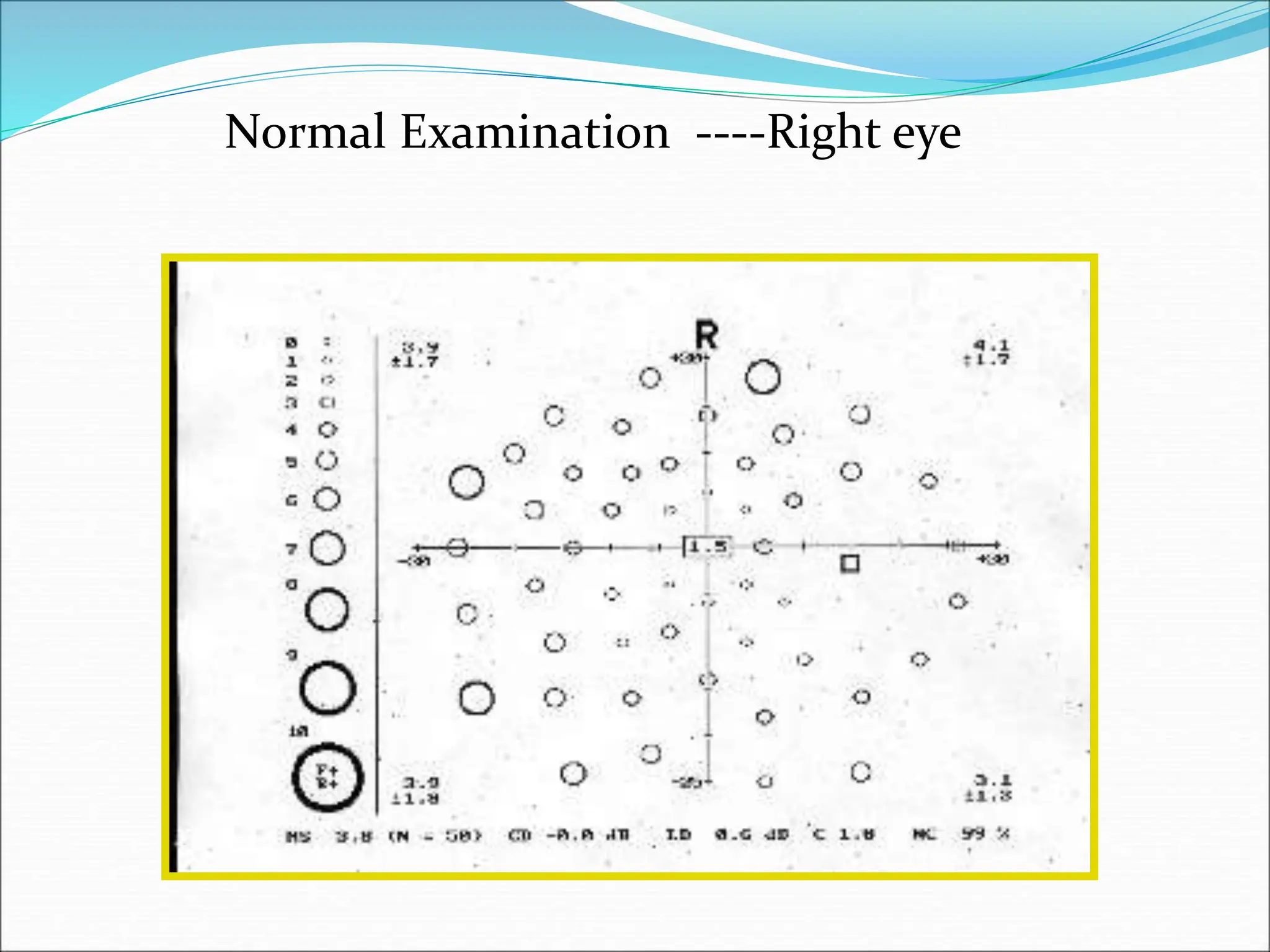
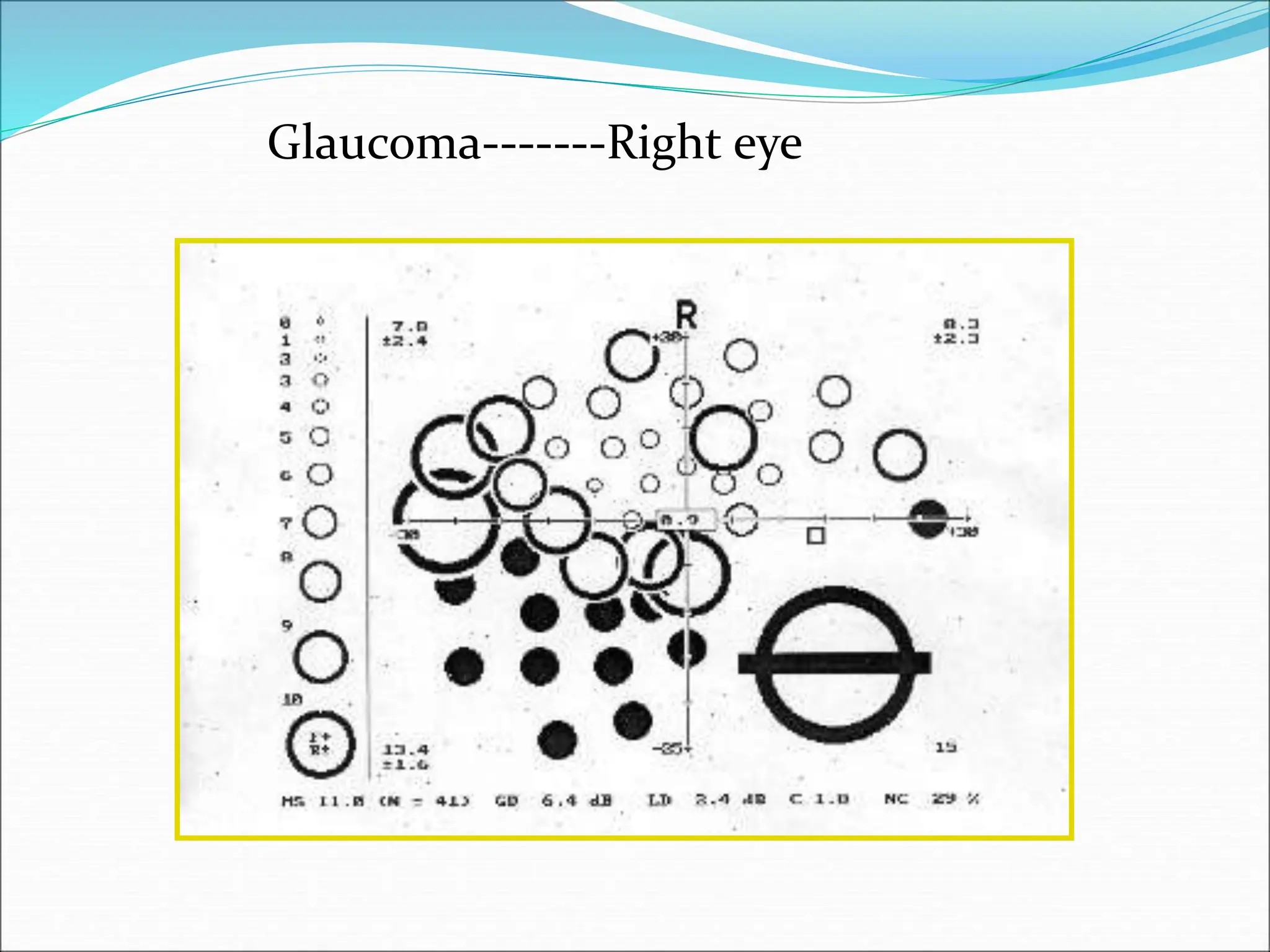
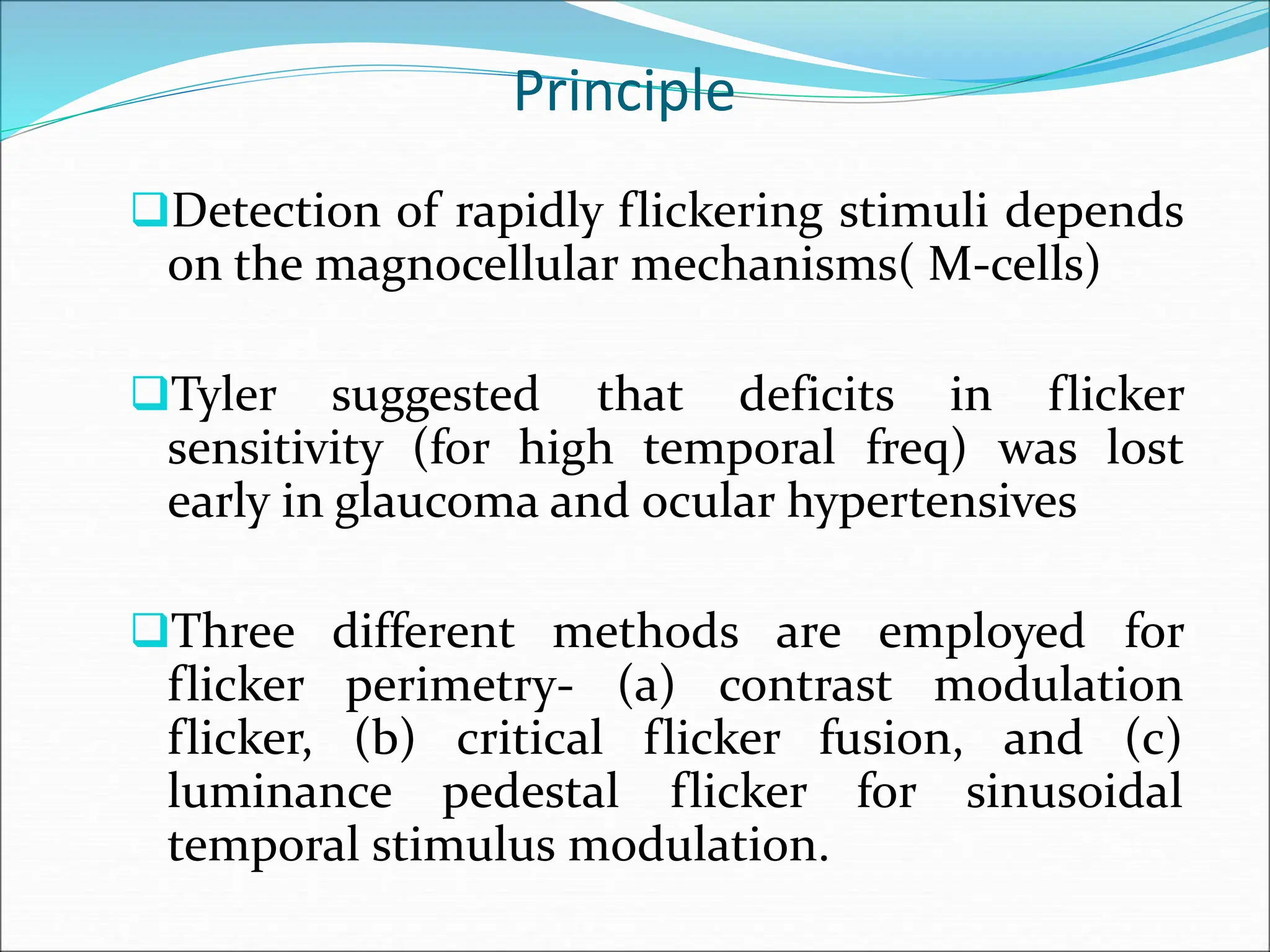
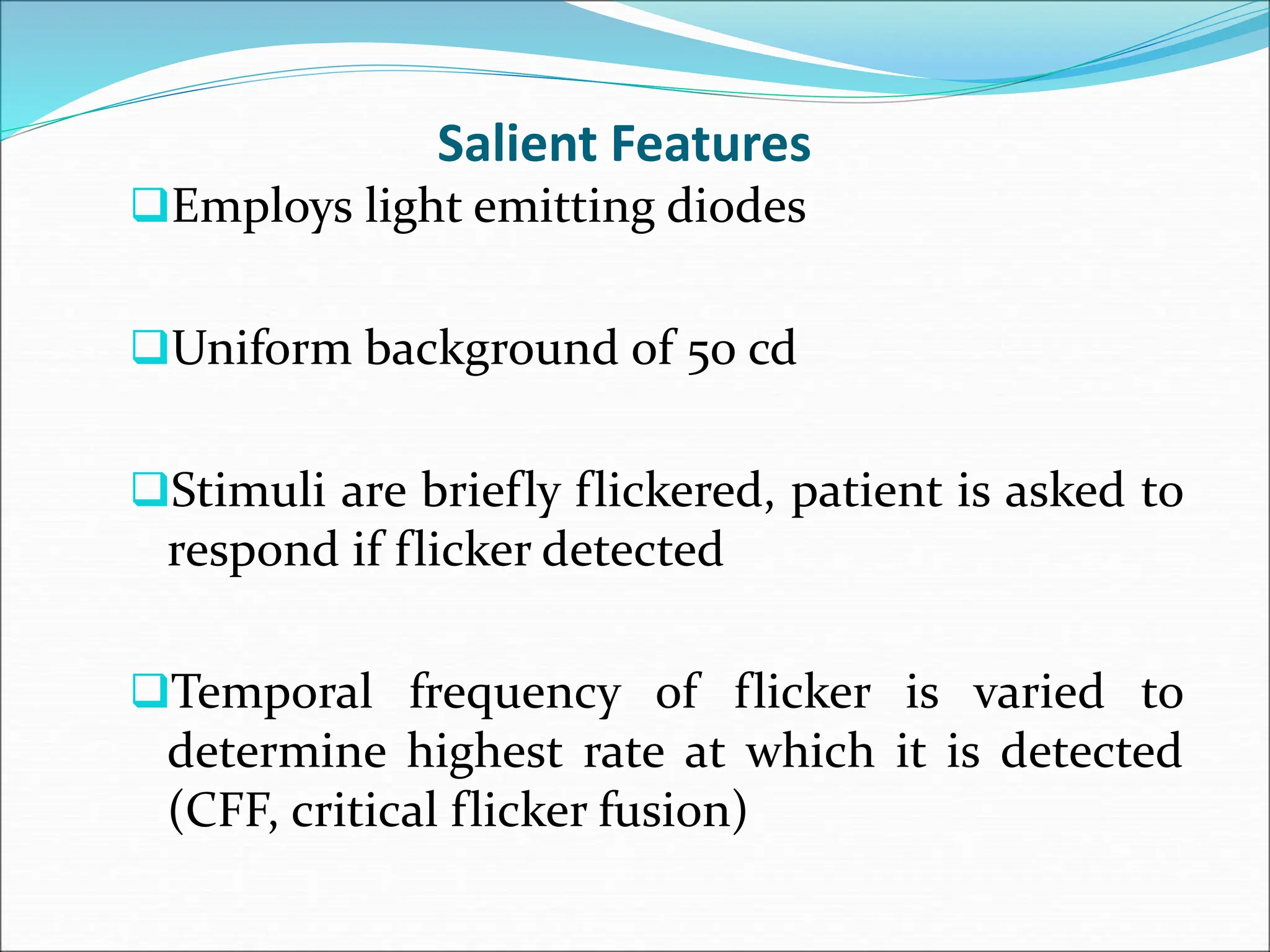
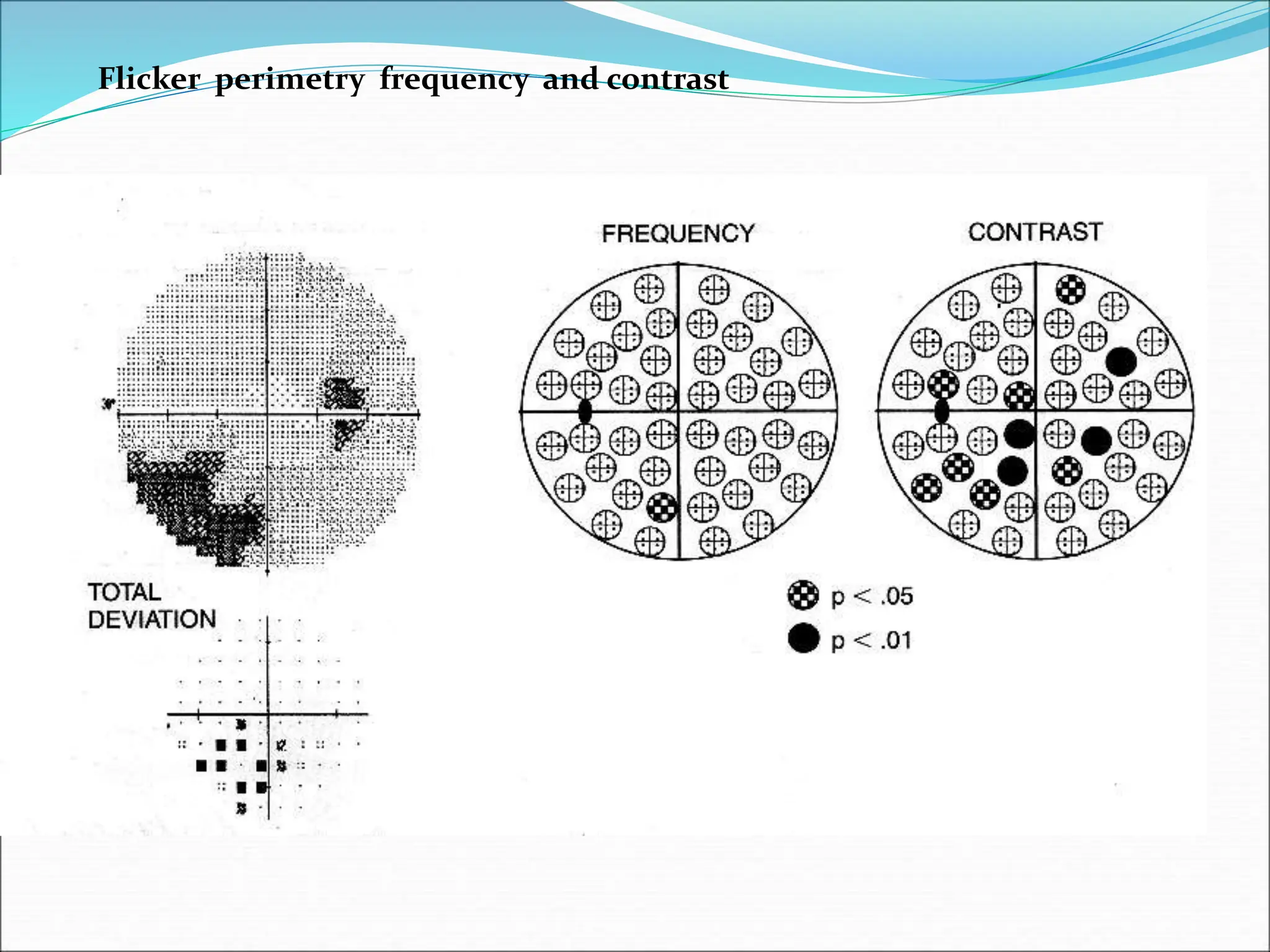
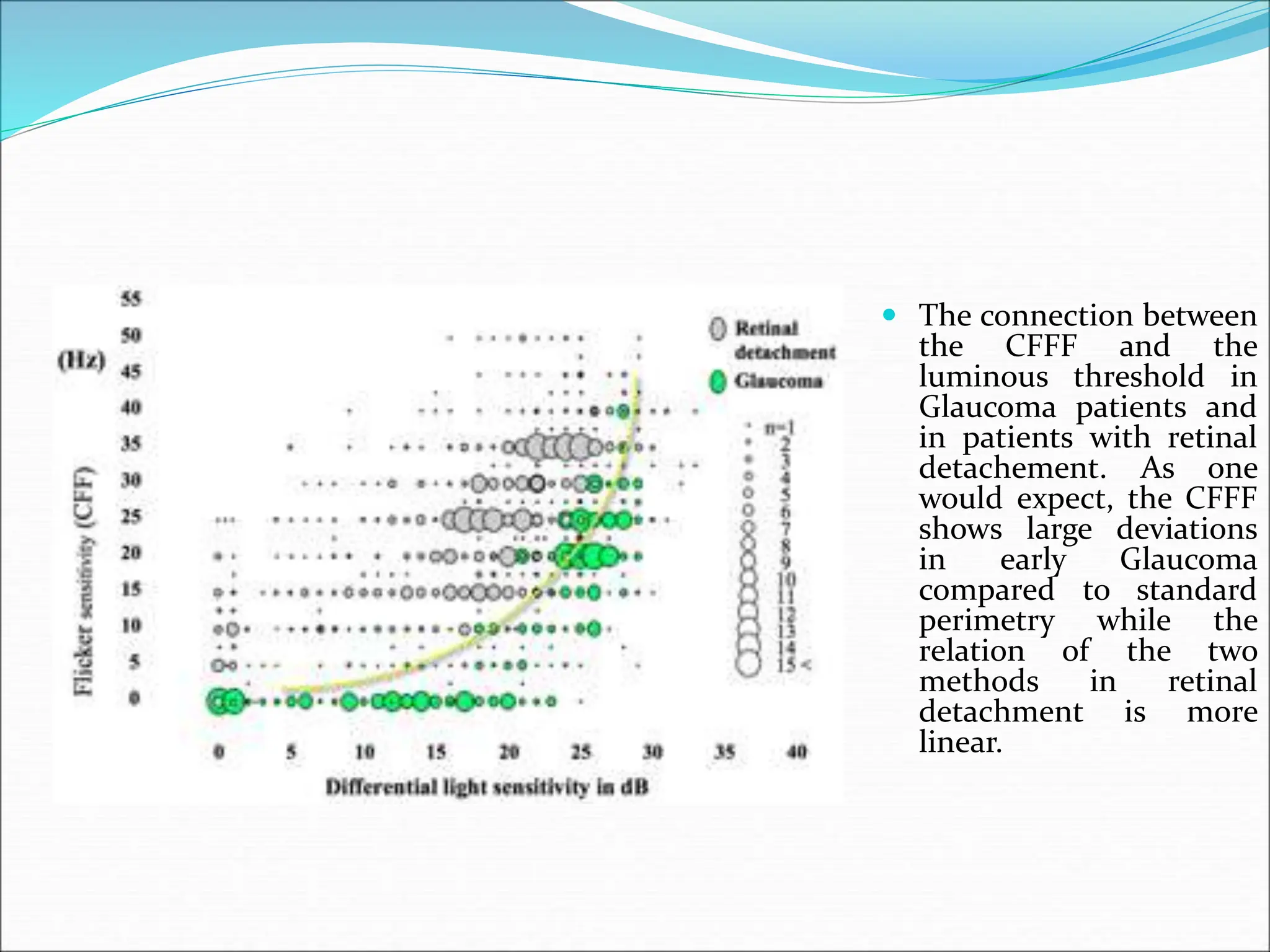
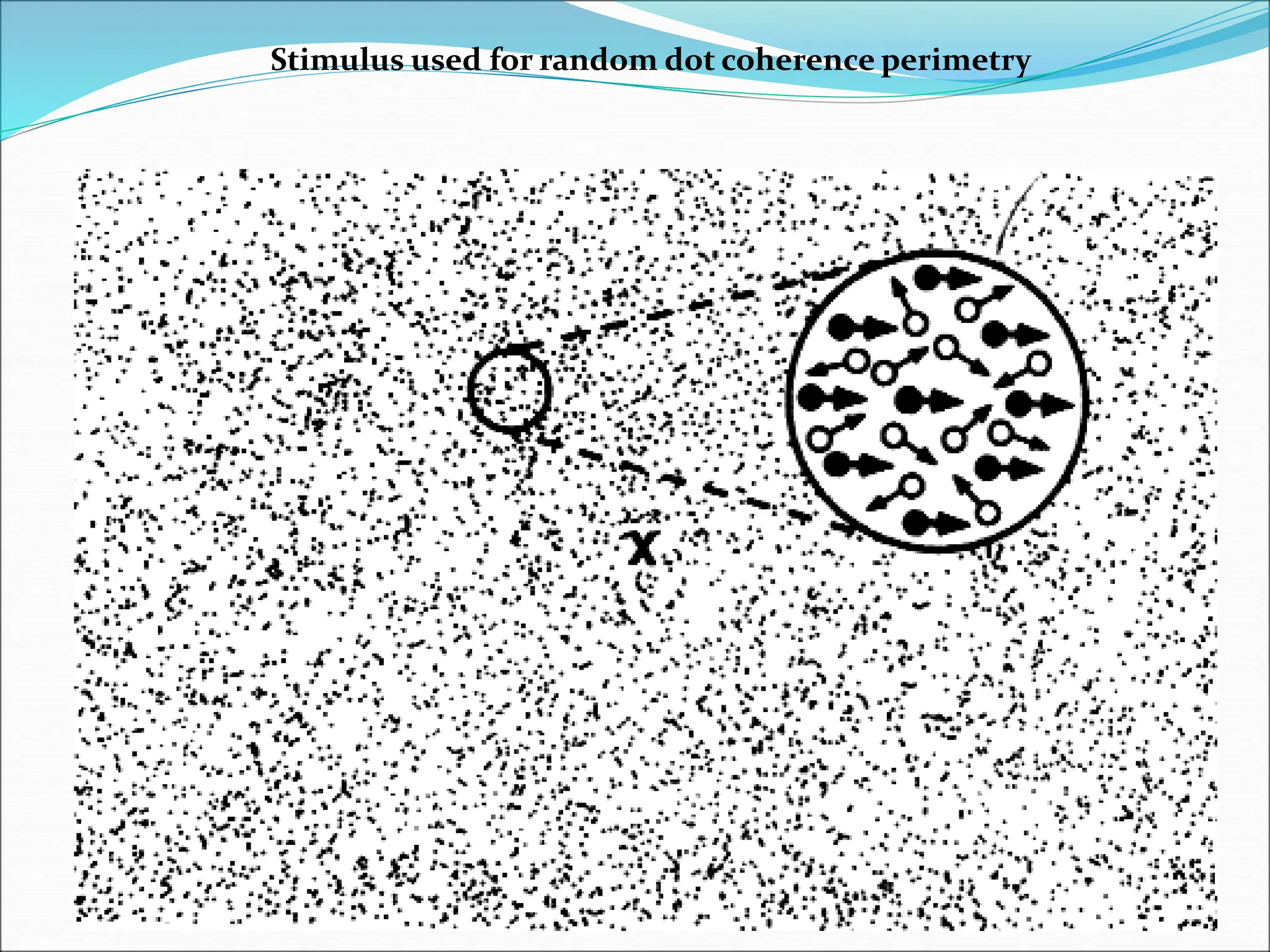
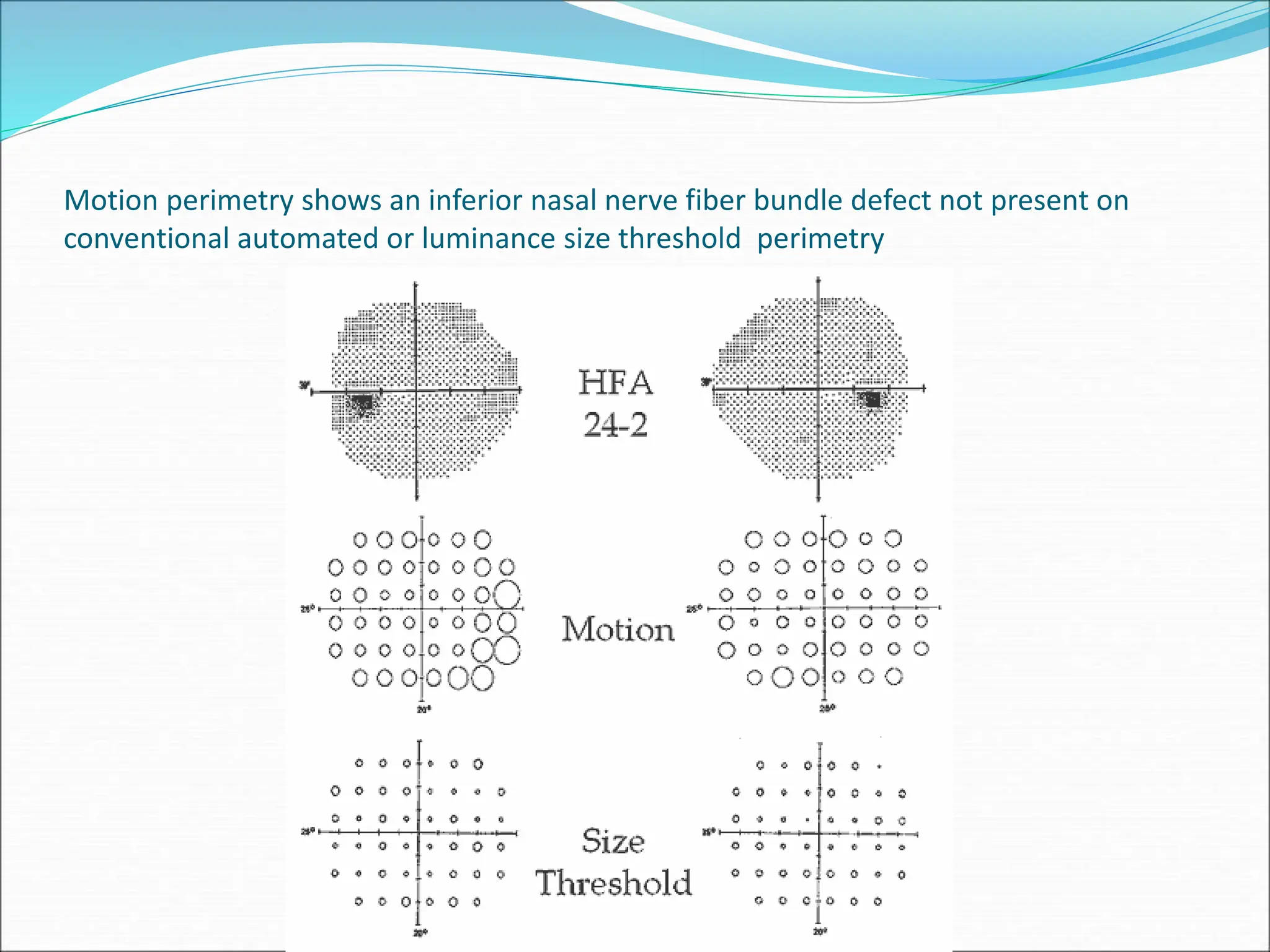
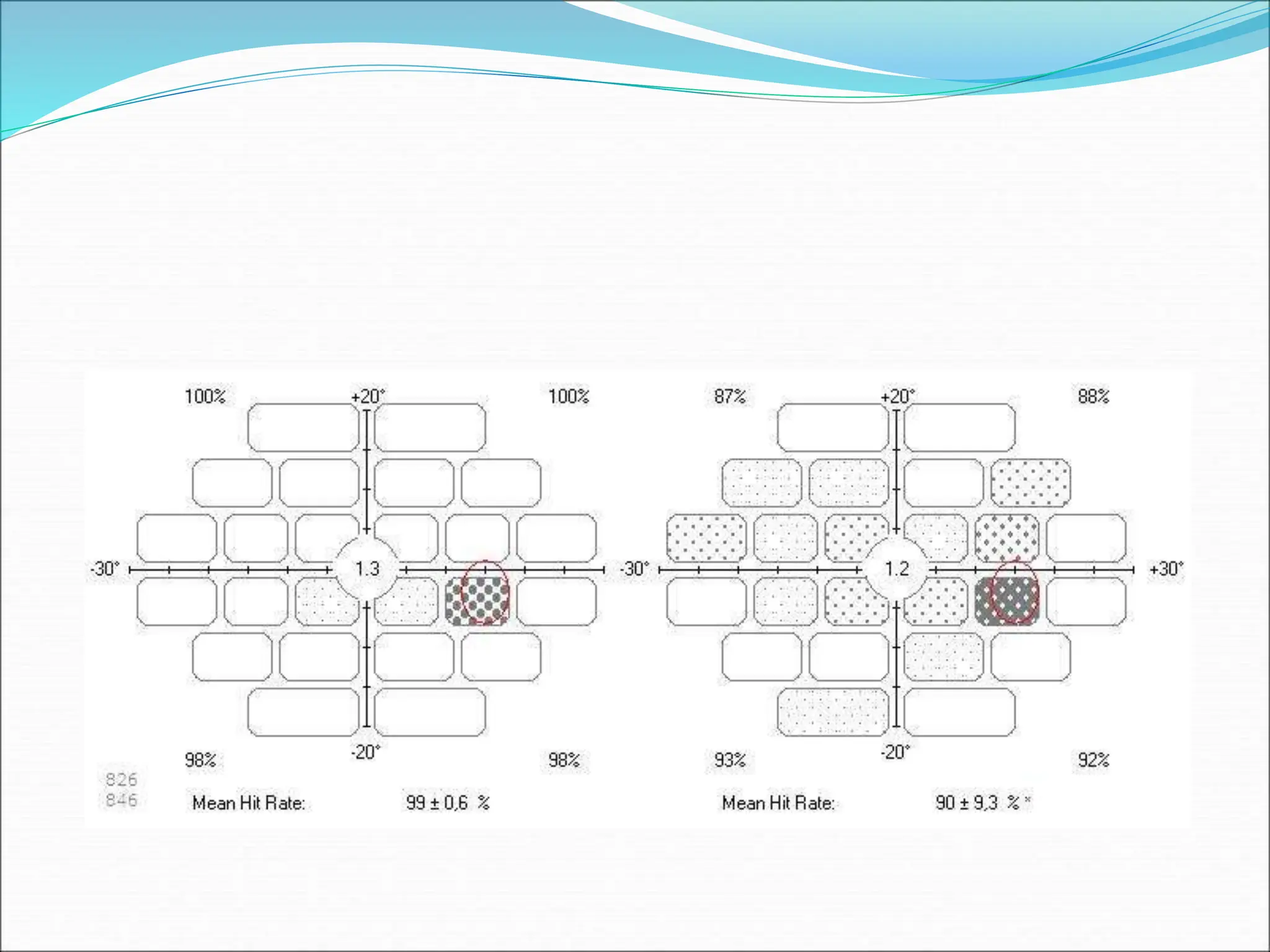
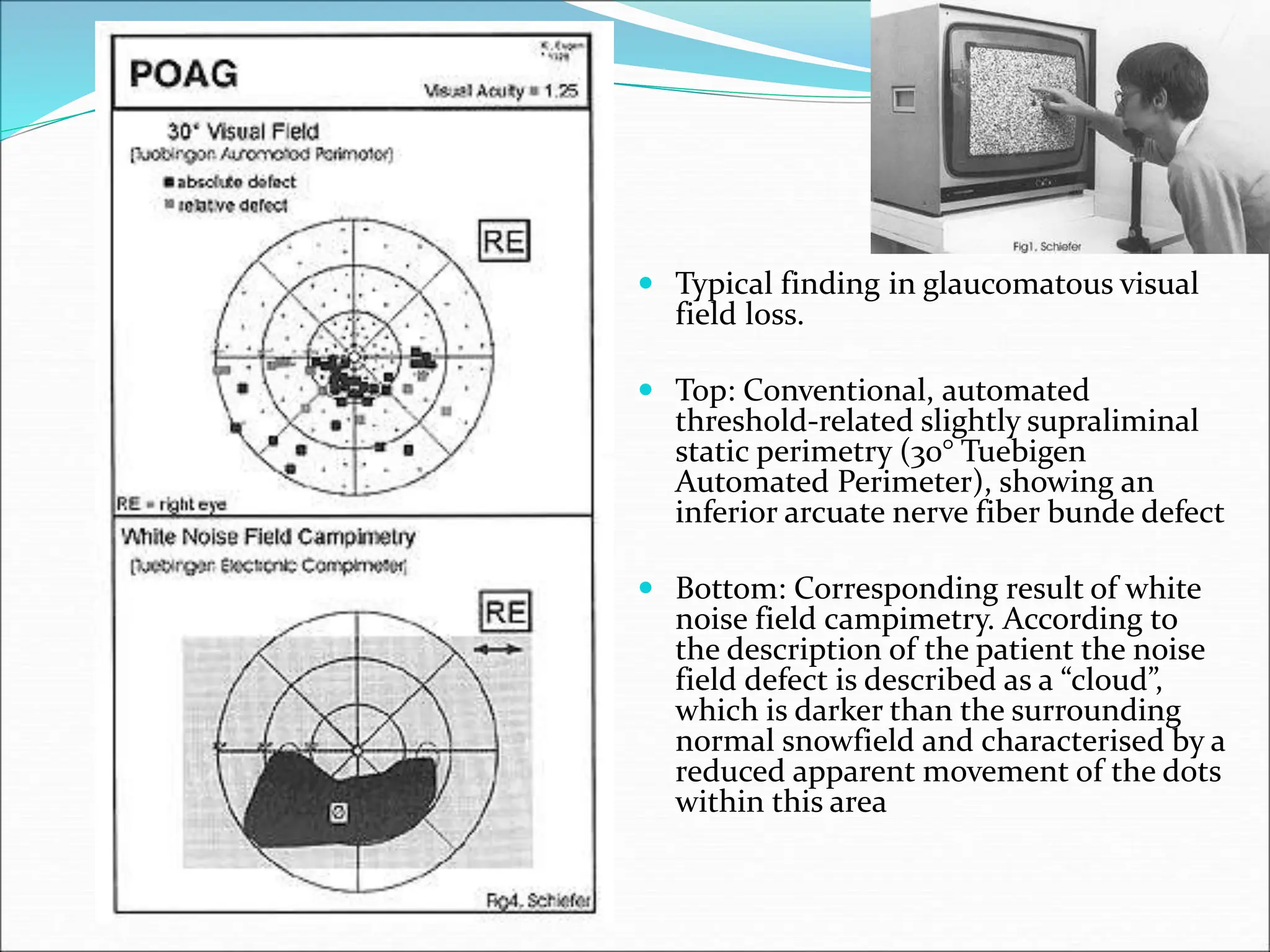
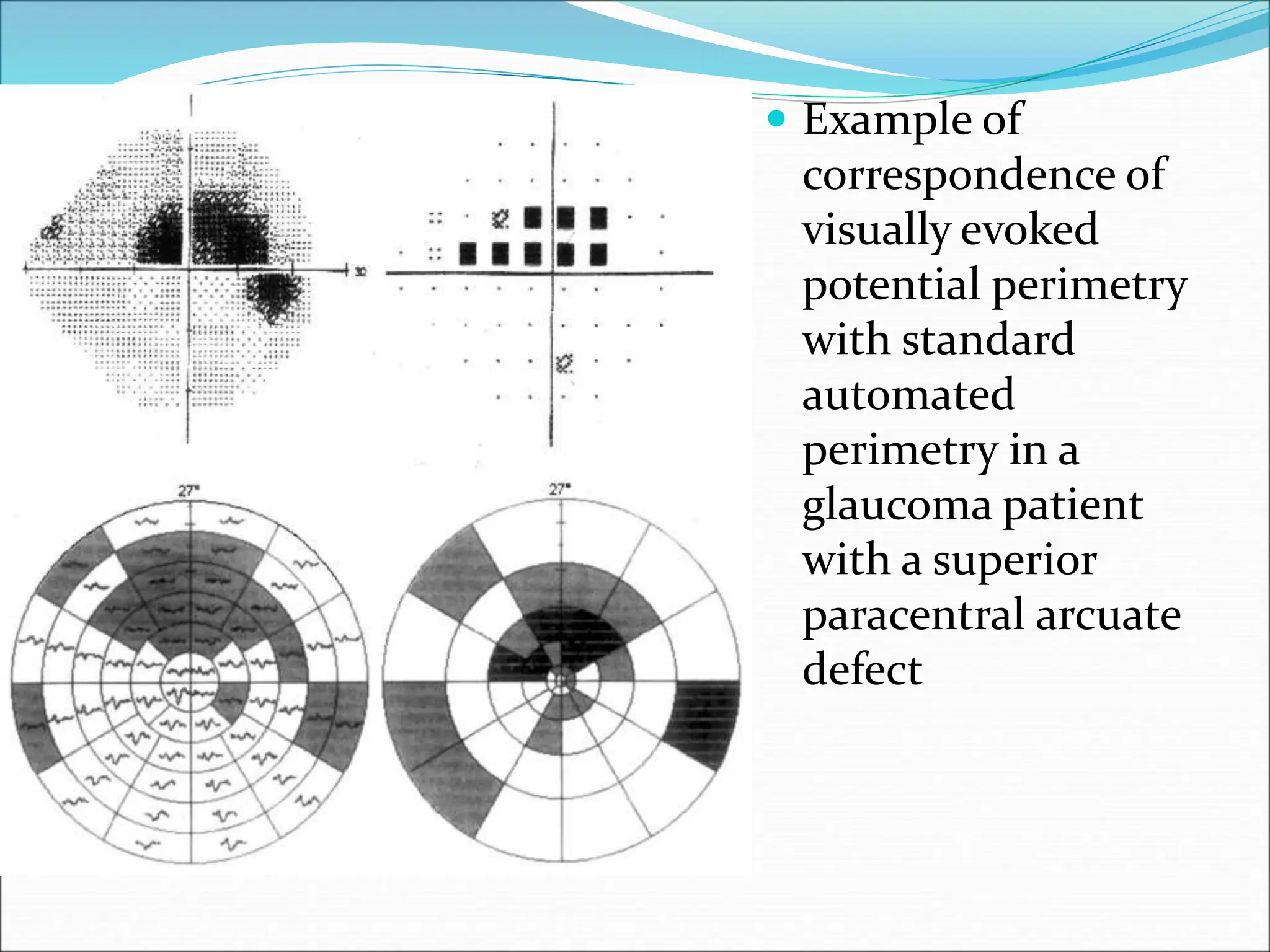
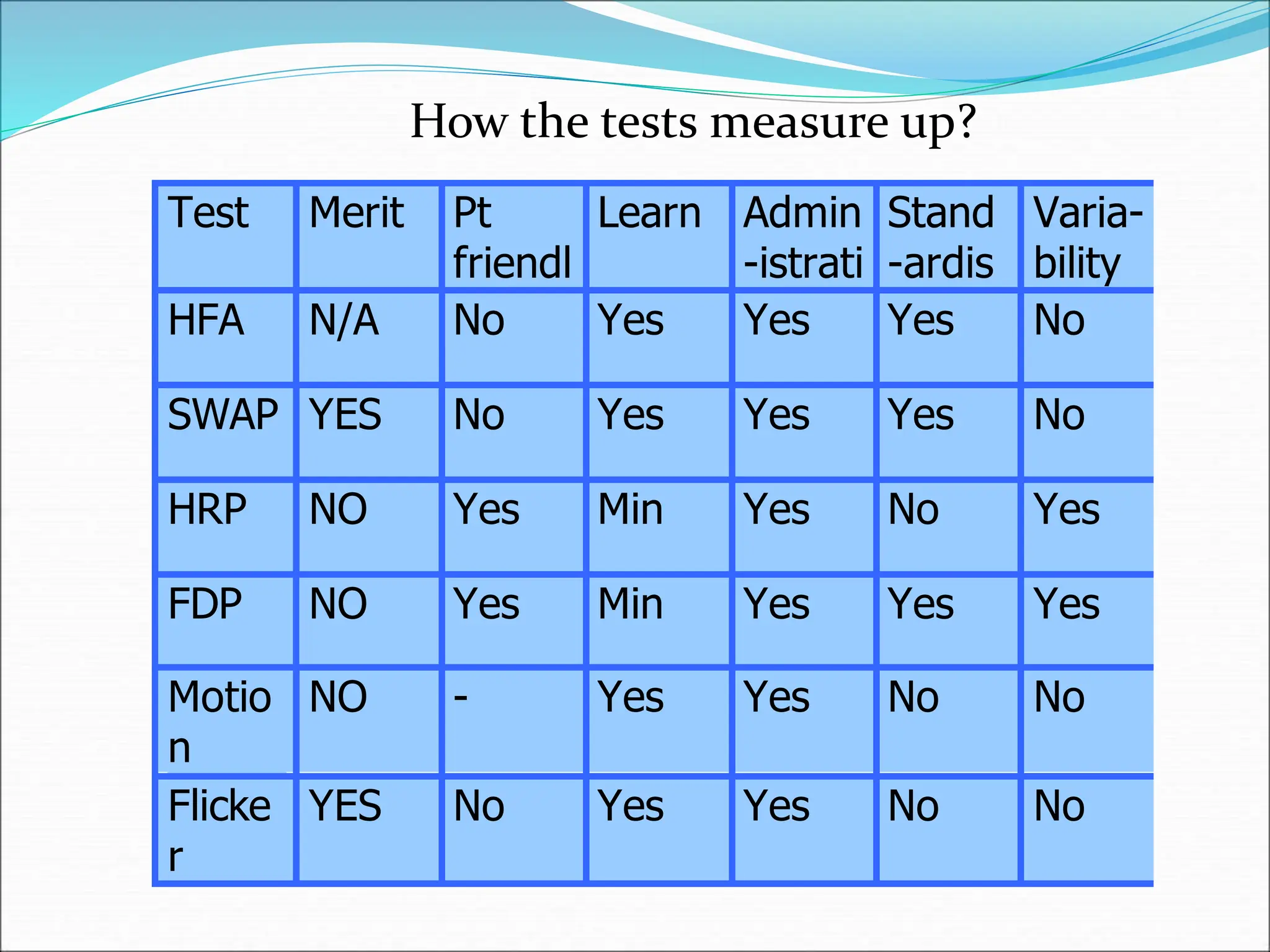
The document discusses ideal features and methods for glaucoma screening, emphasizing tests like octopus perimetry and newer techniques such as short wave automated perimetry and frequency doubling perimetry. It details procedures for detecting and analyzing progression in visual field defects with statistical evaluations and clinical examples for effective monitoring. The importance of establishing baselines and employing advanced software for detecting changes is highlighted to improve patient management and outcomes.