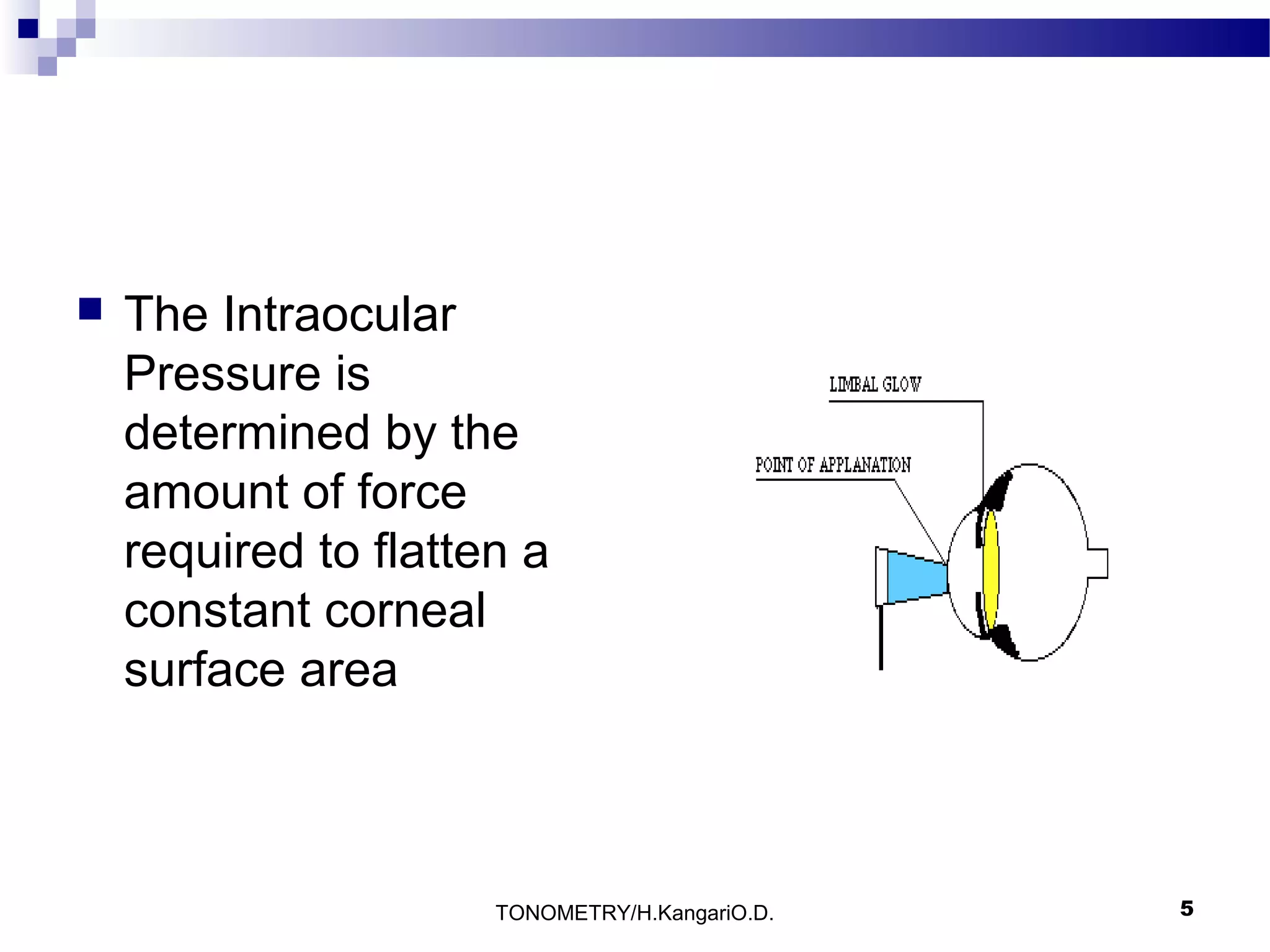
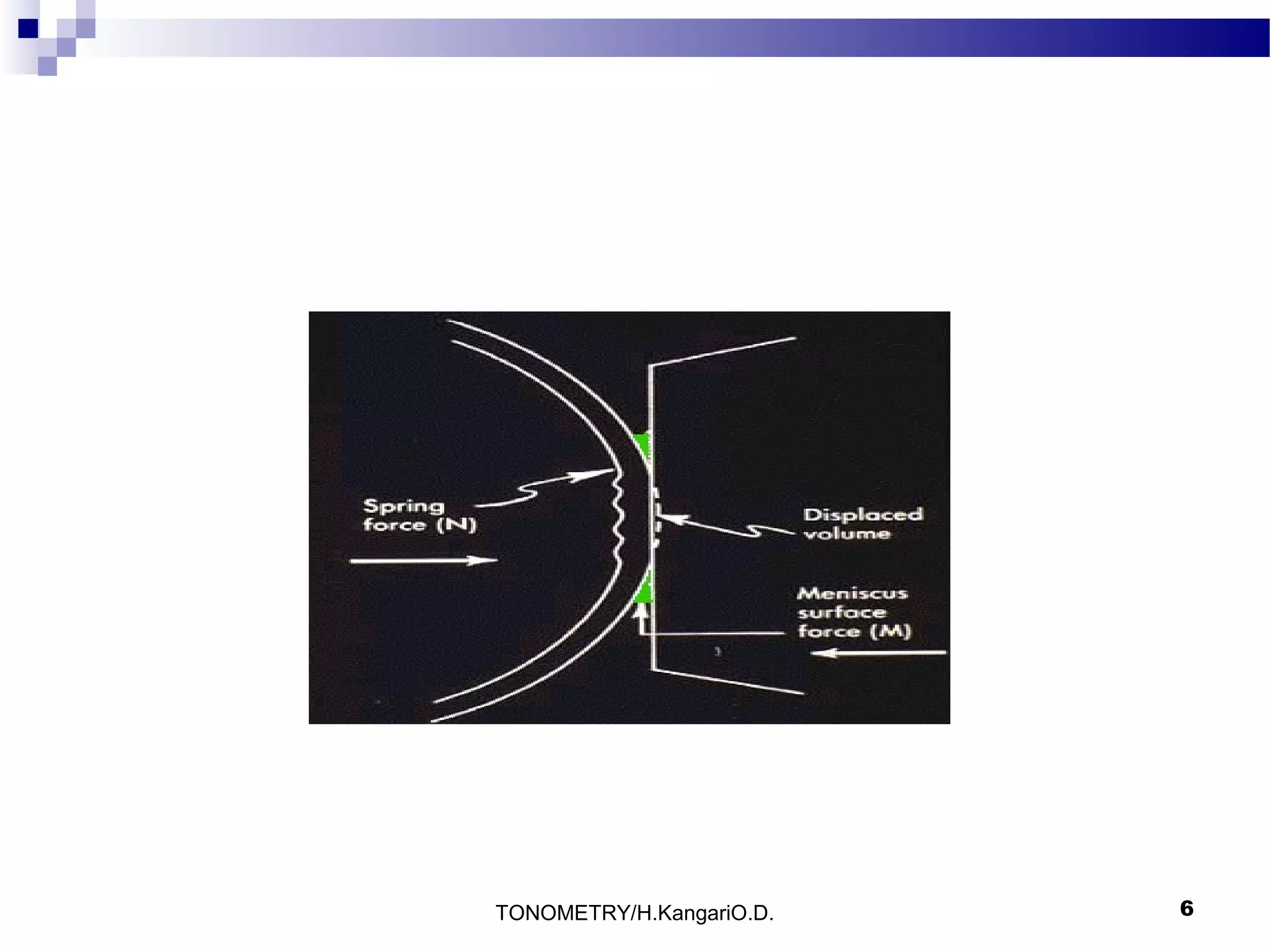
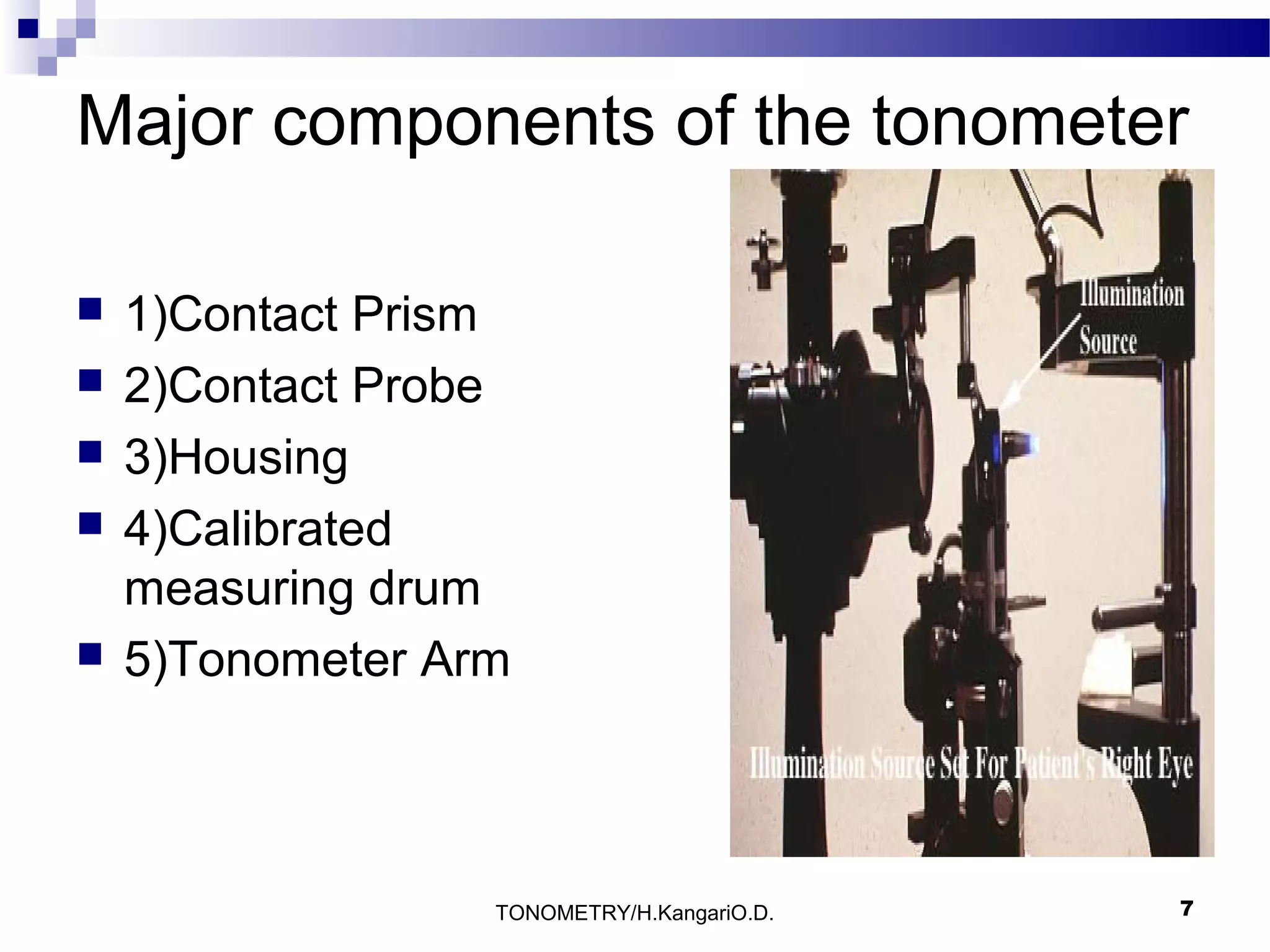
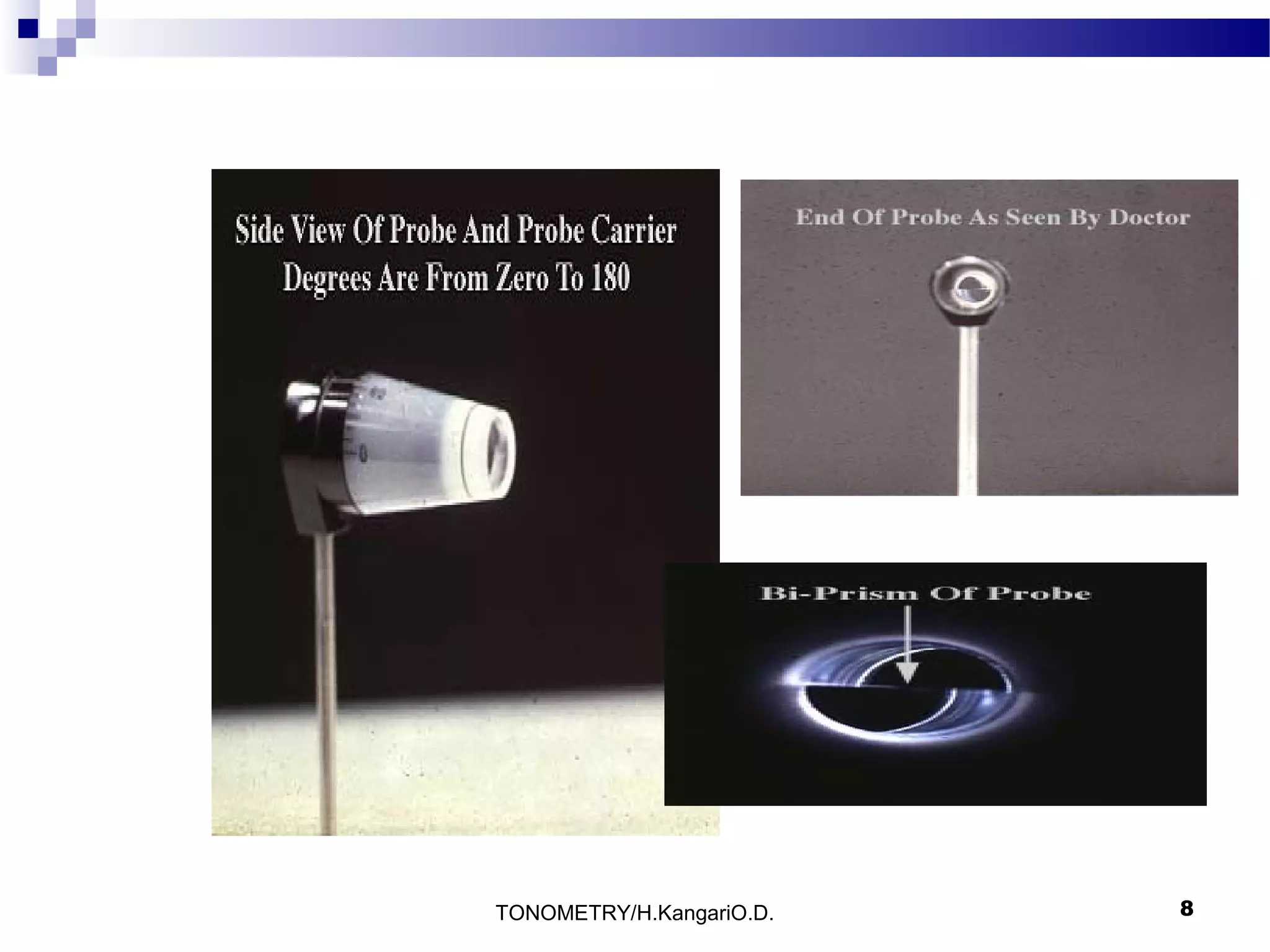
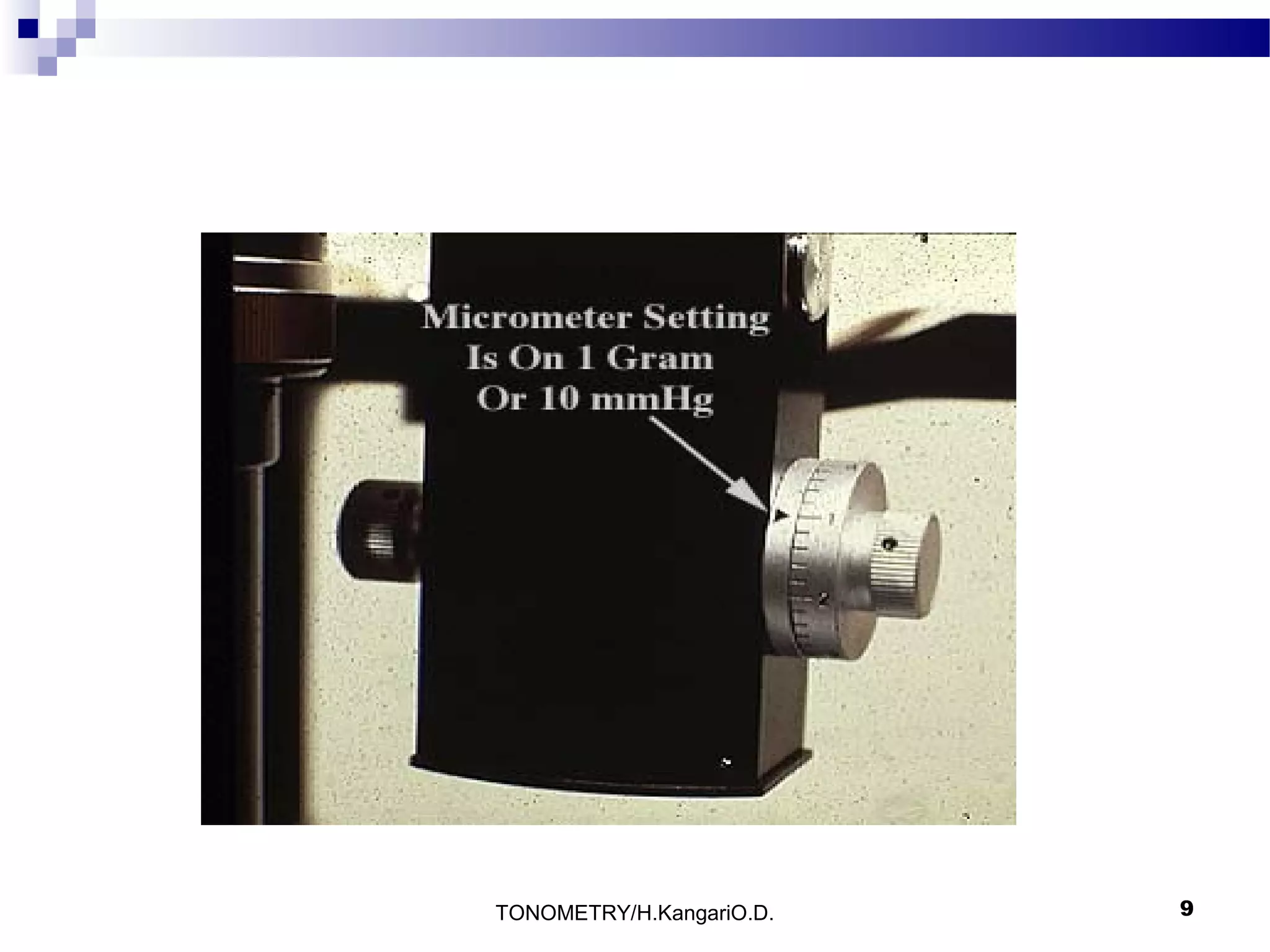
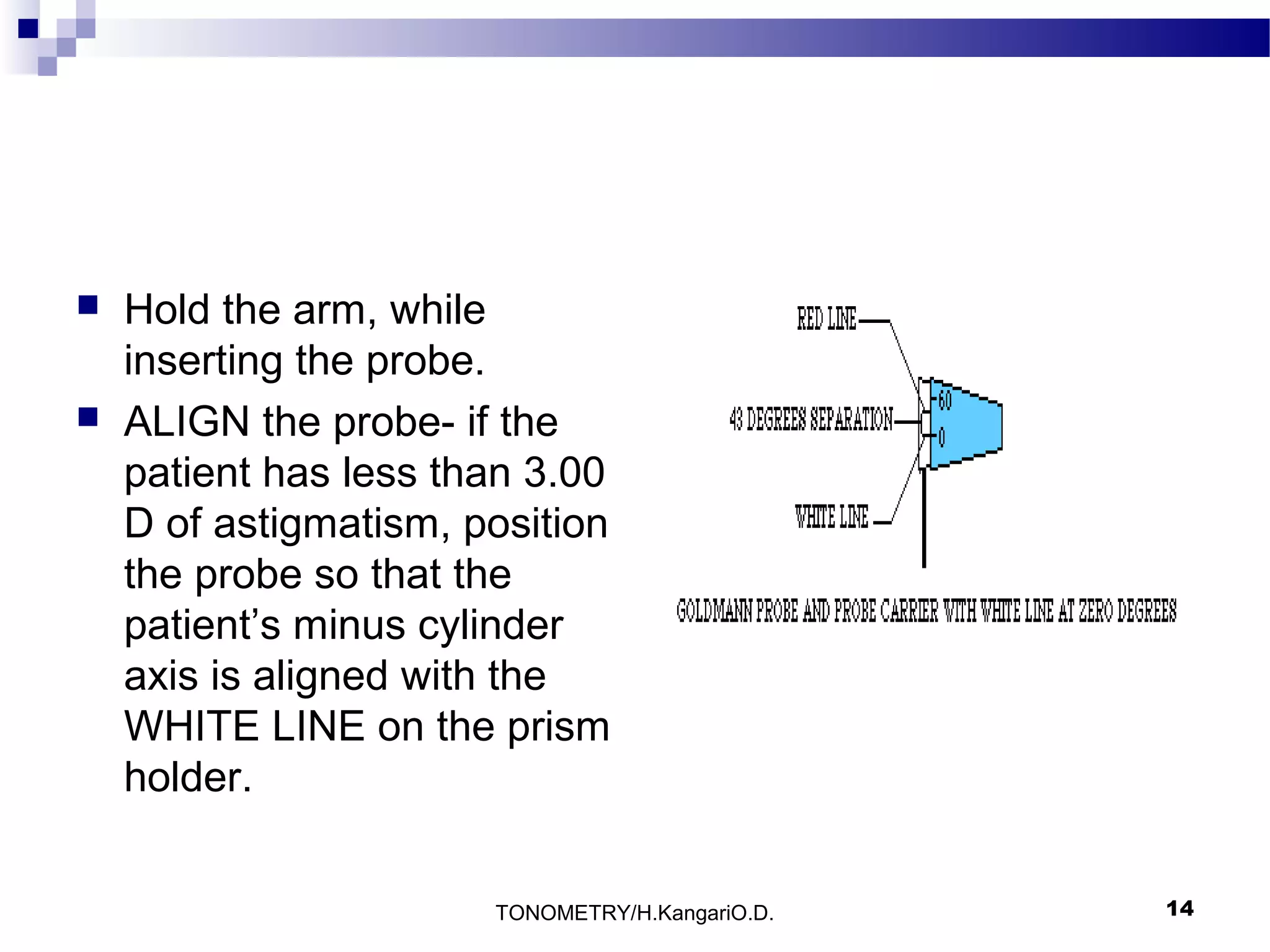
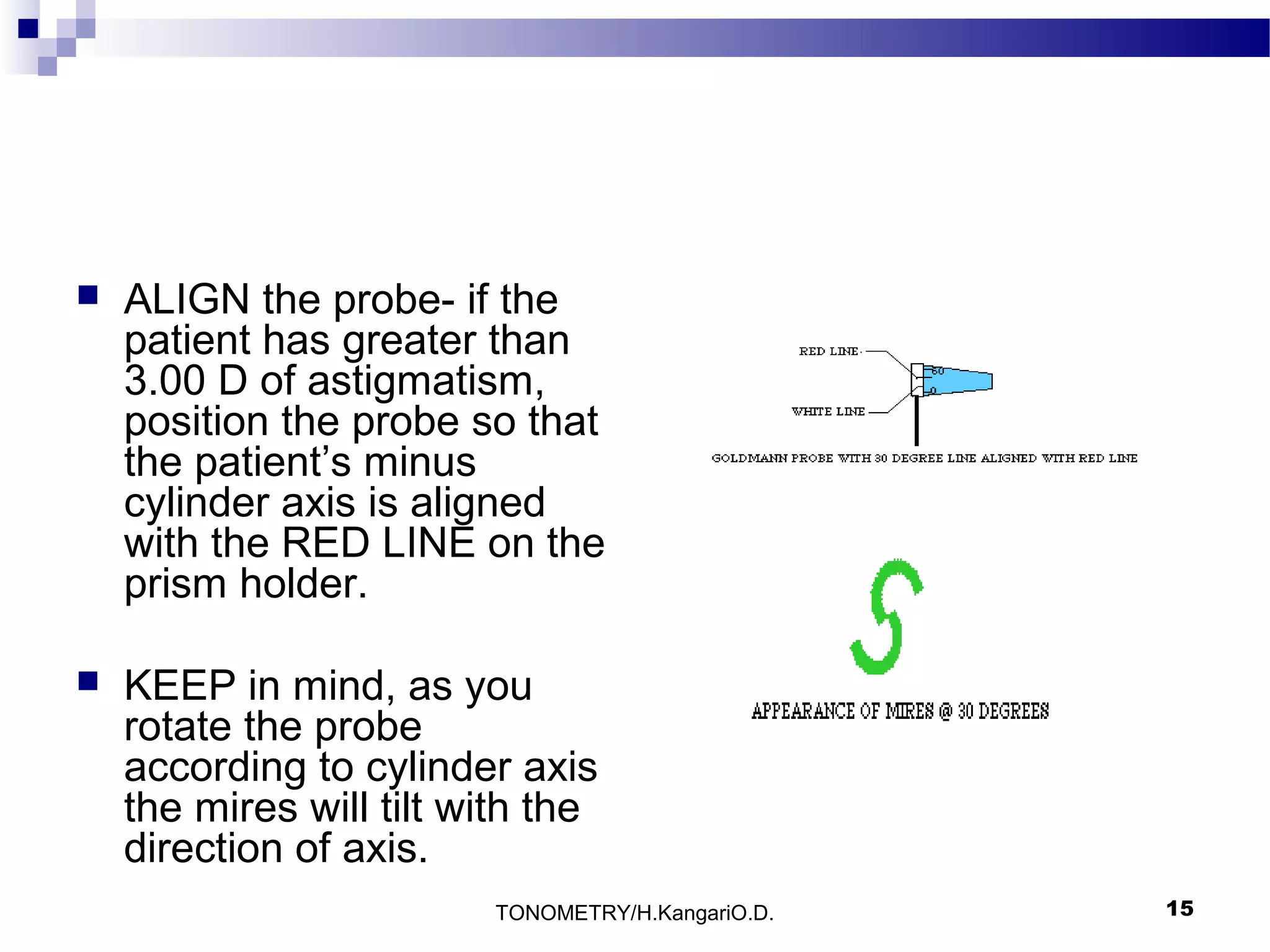
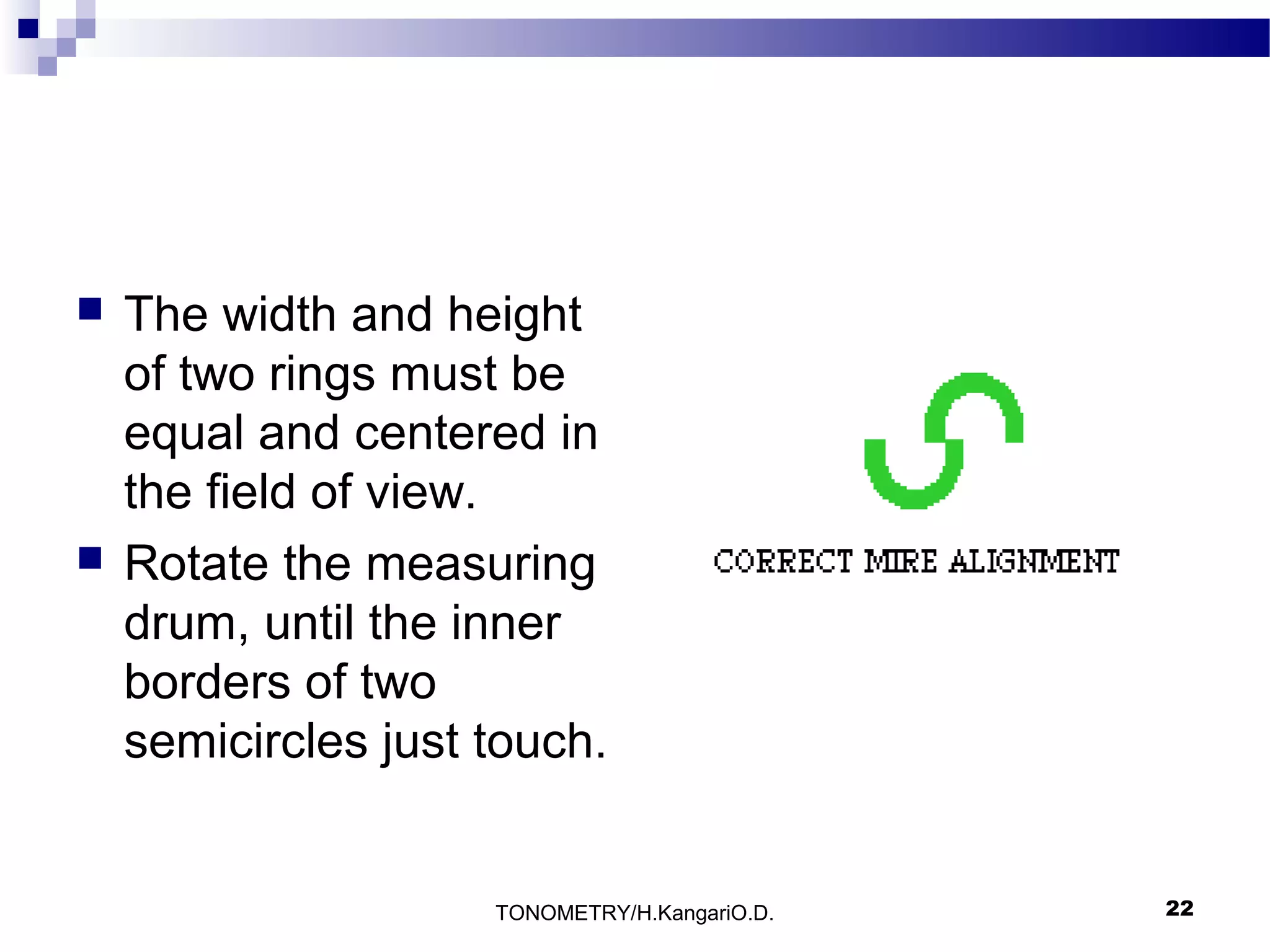
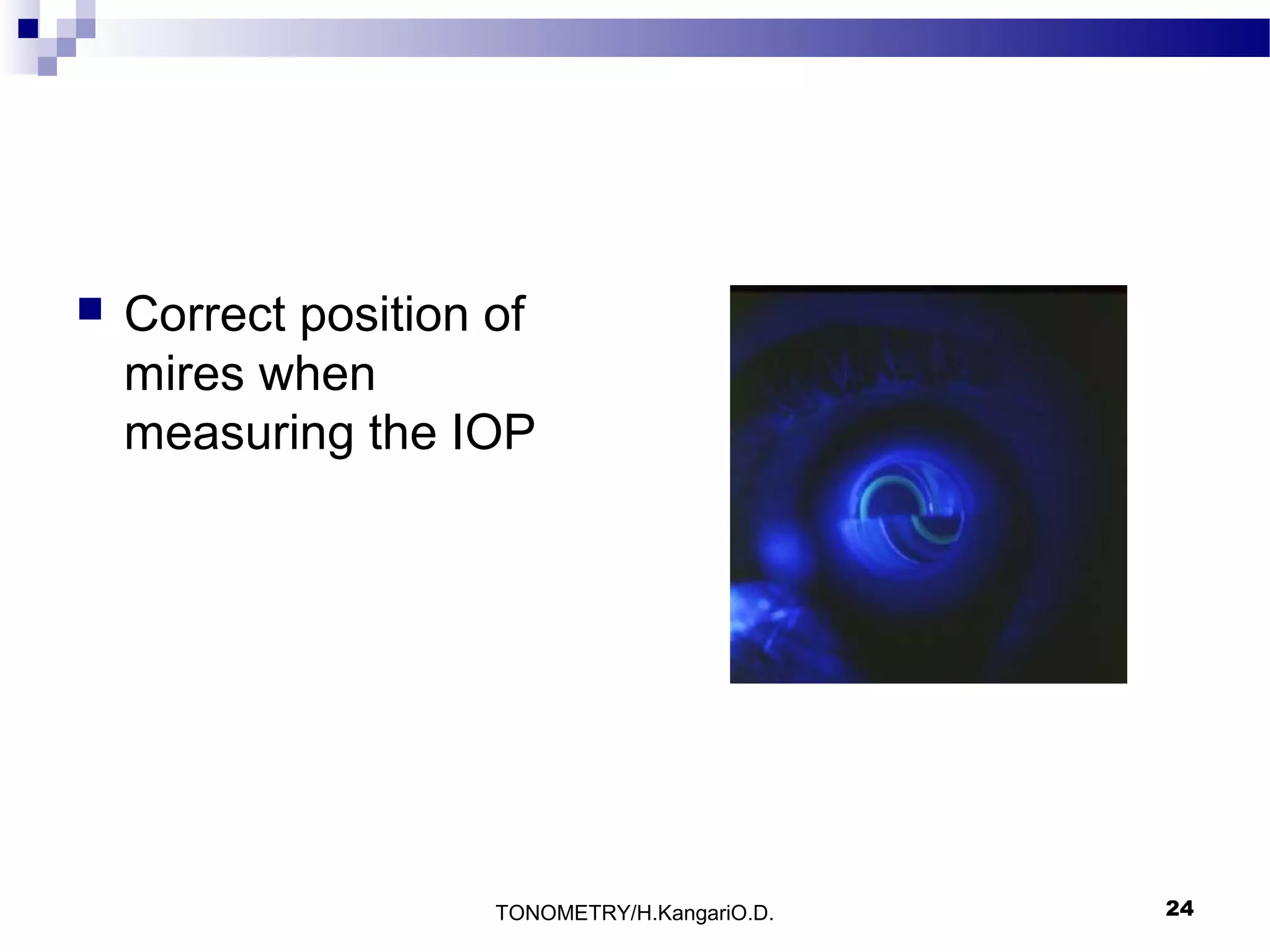
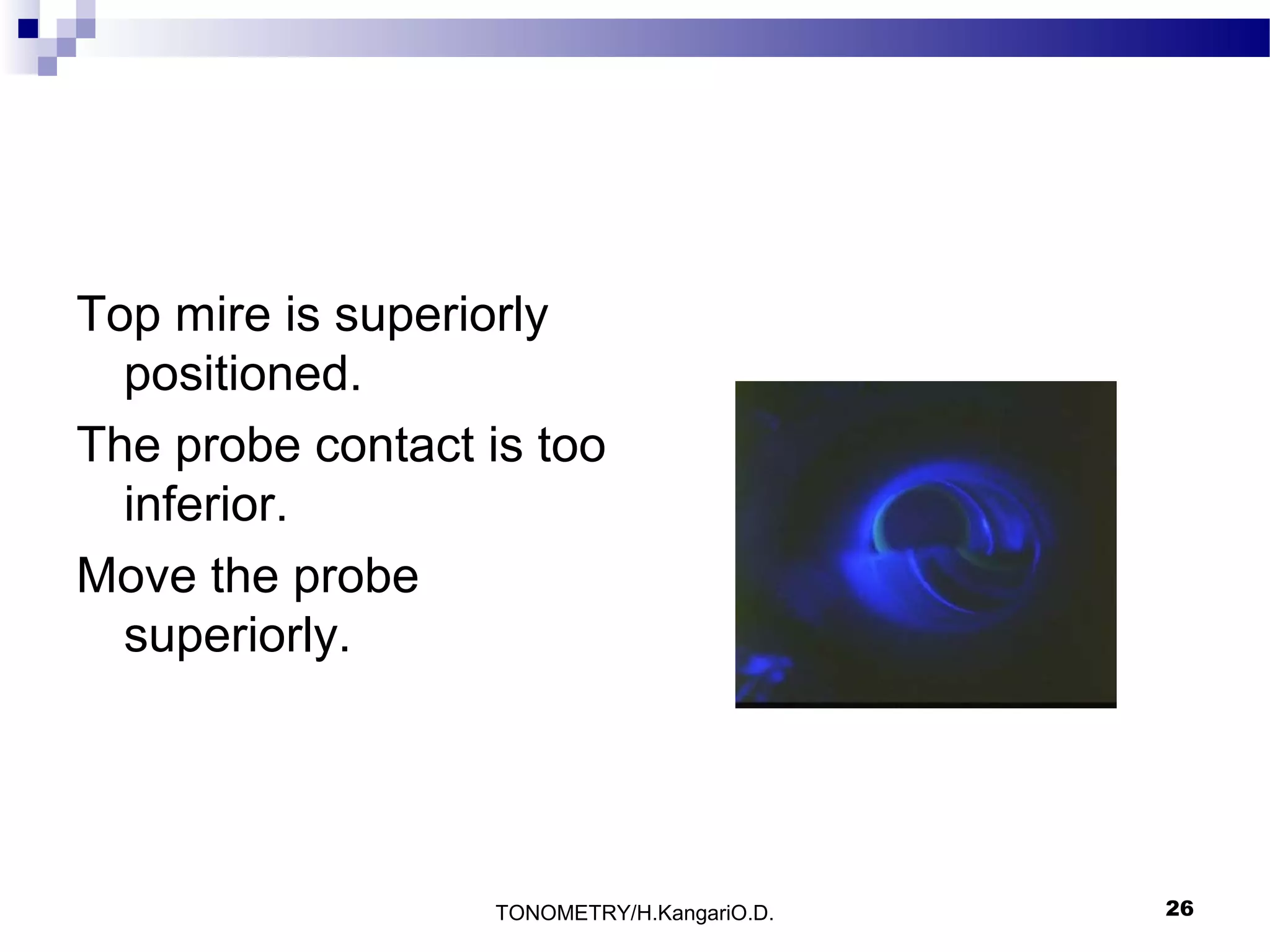
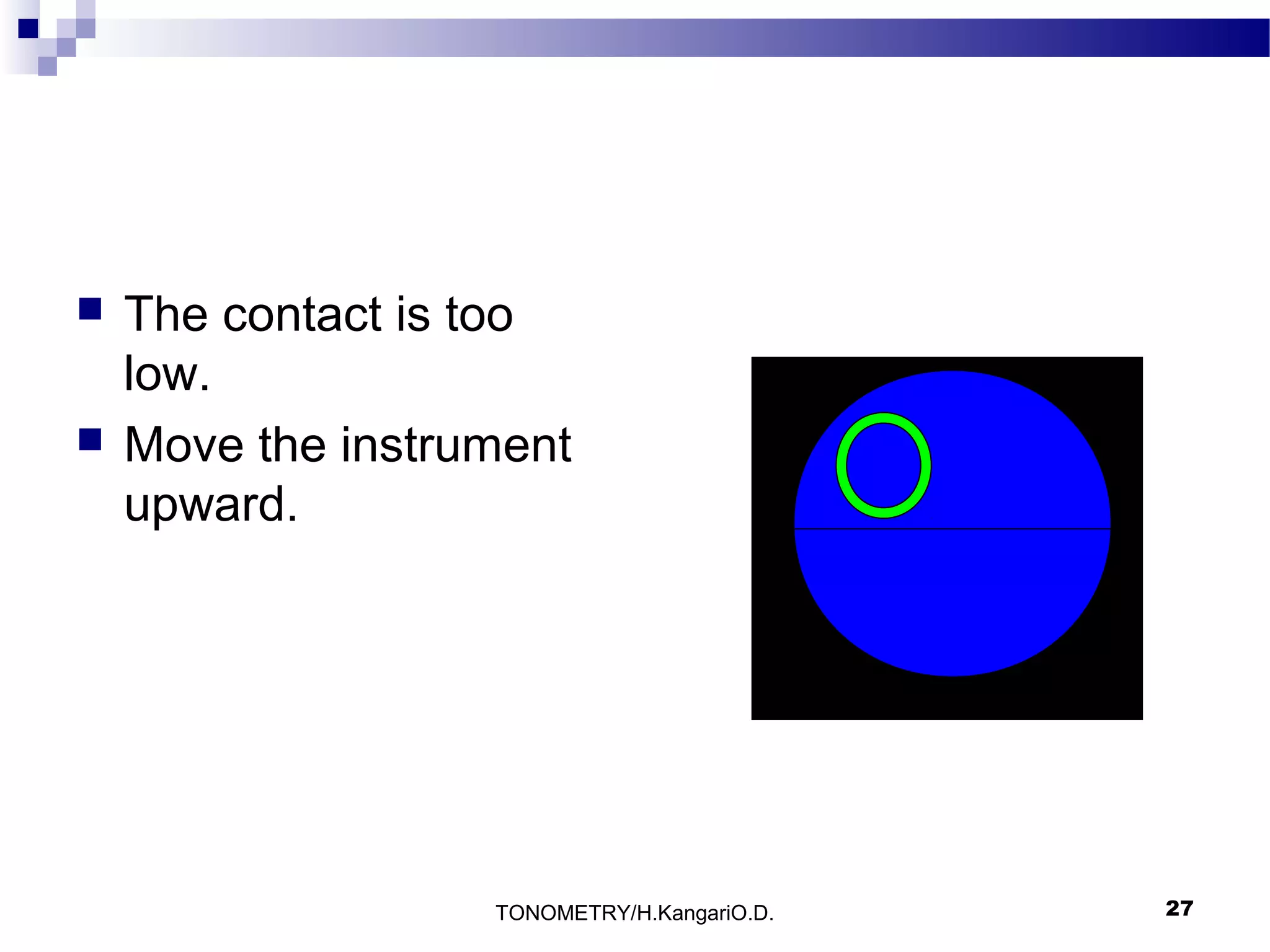
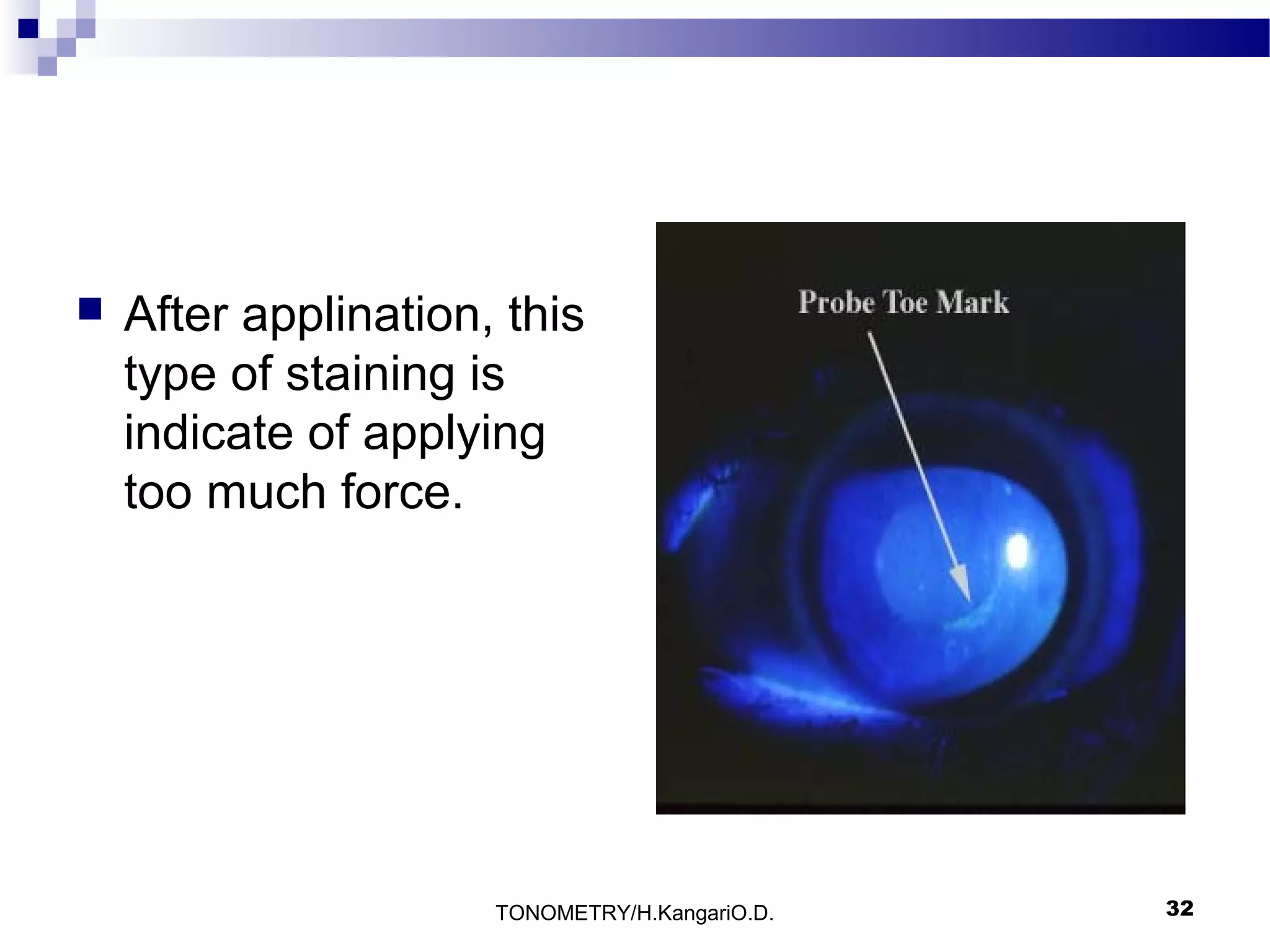
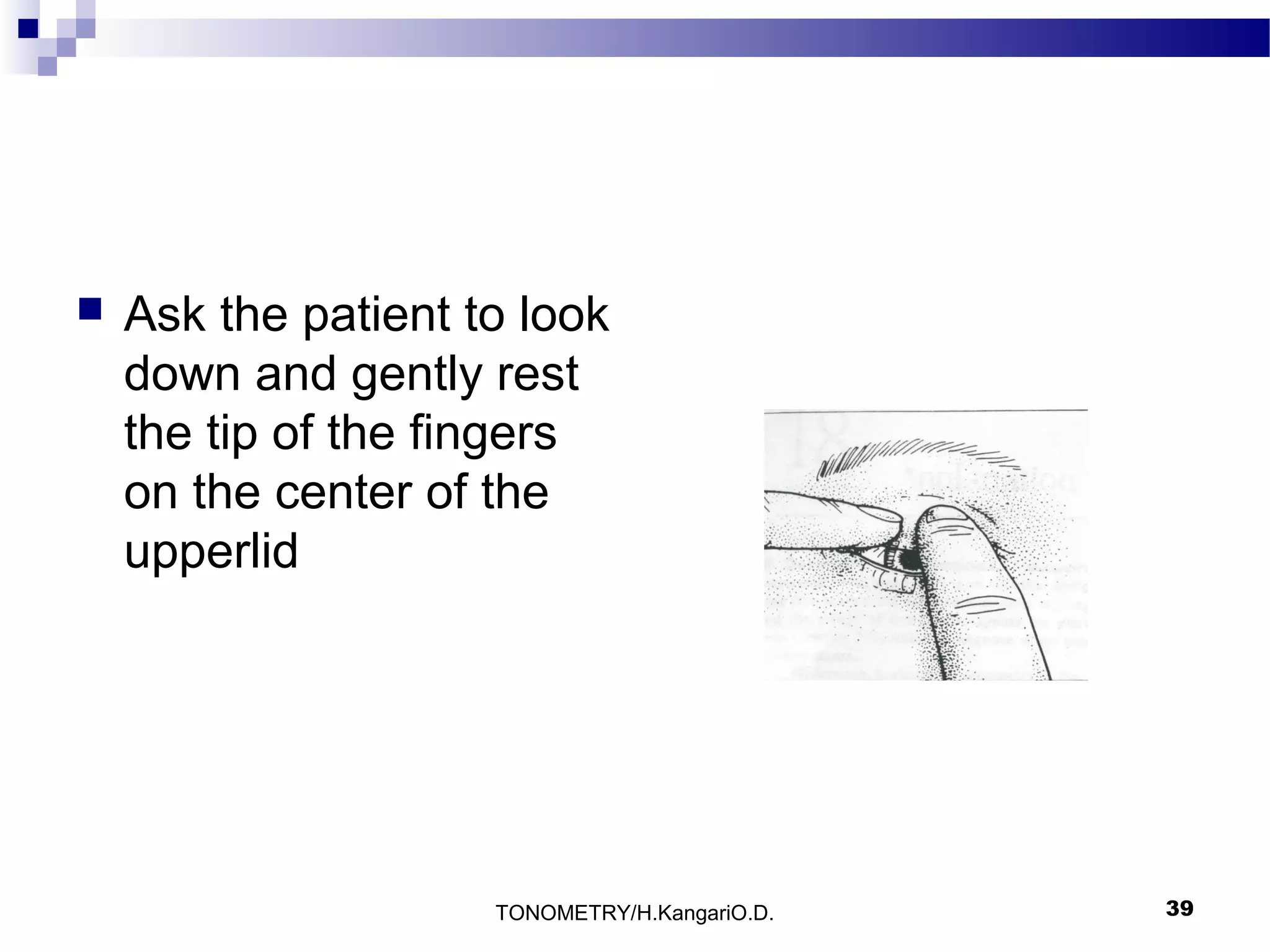
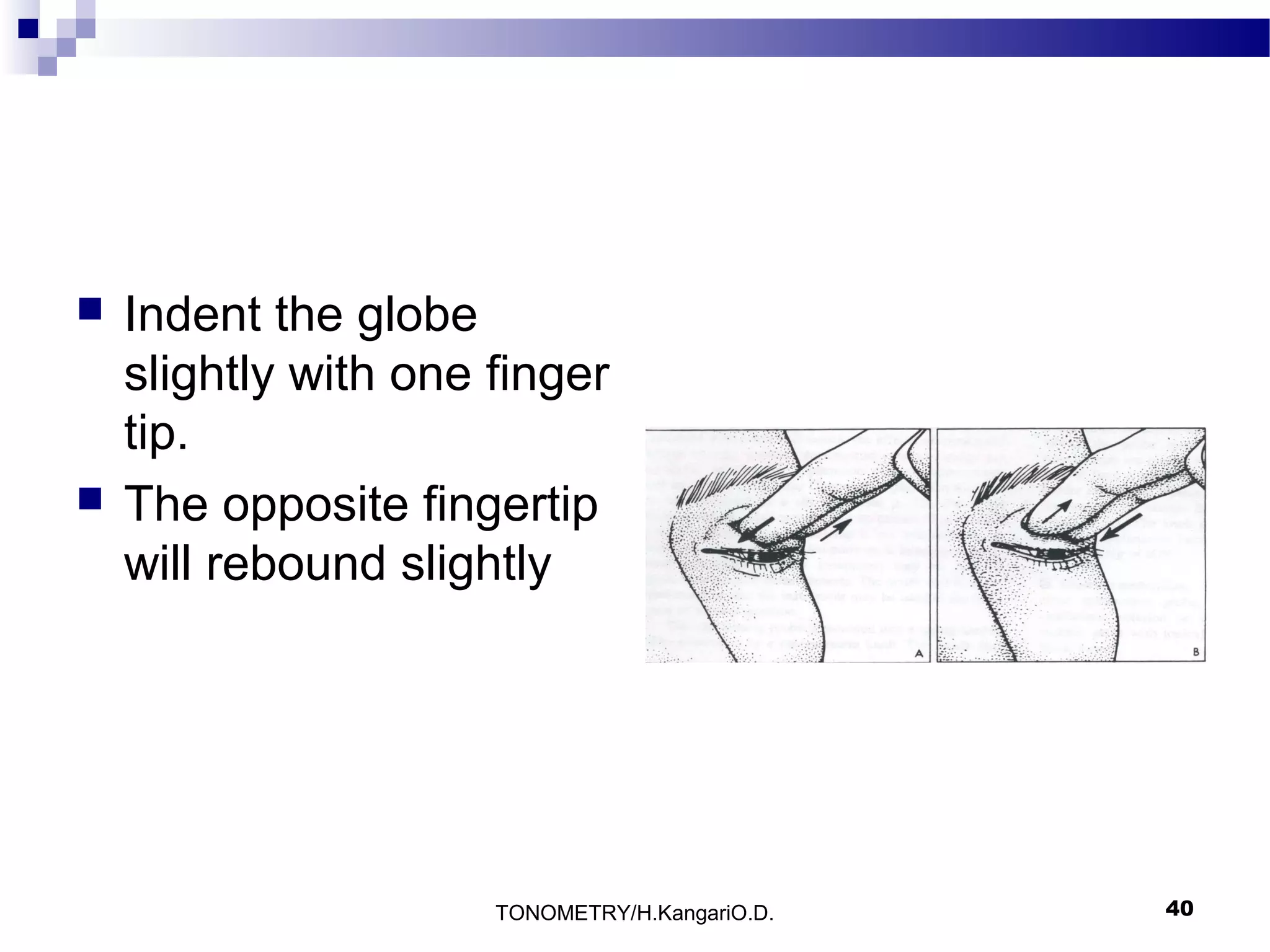
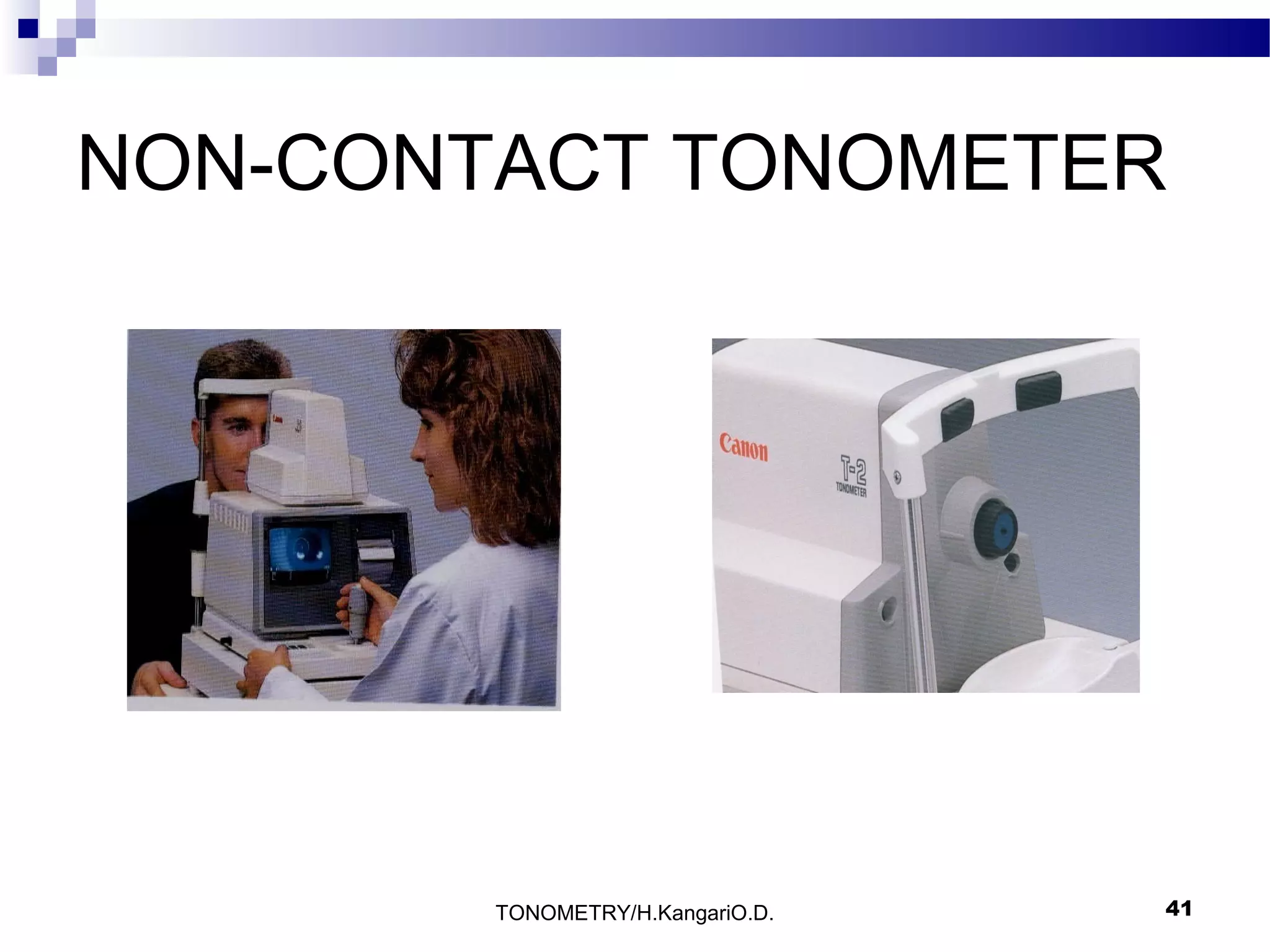
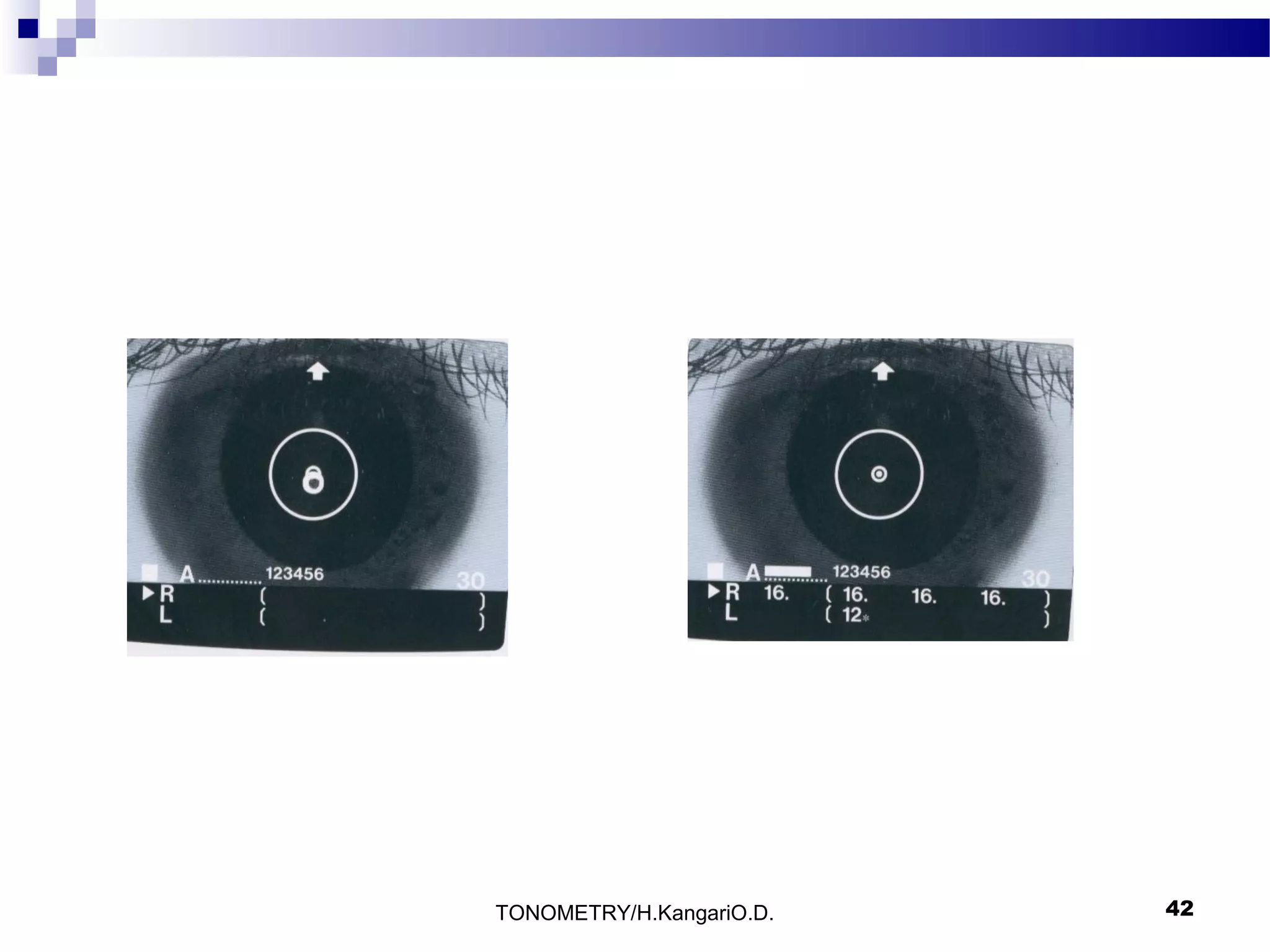
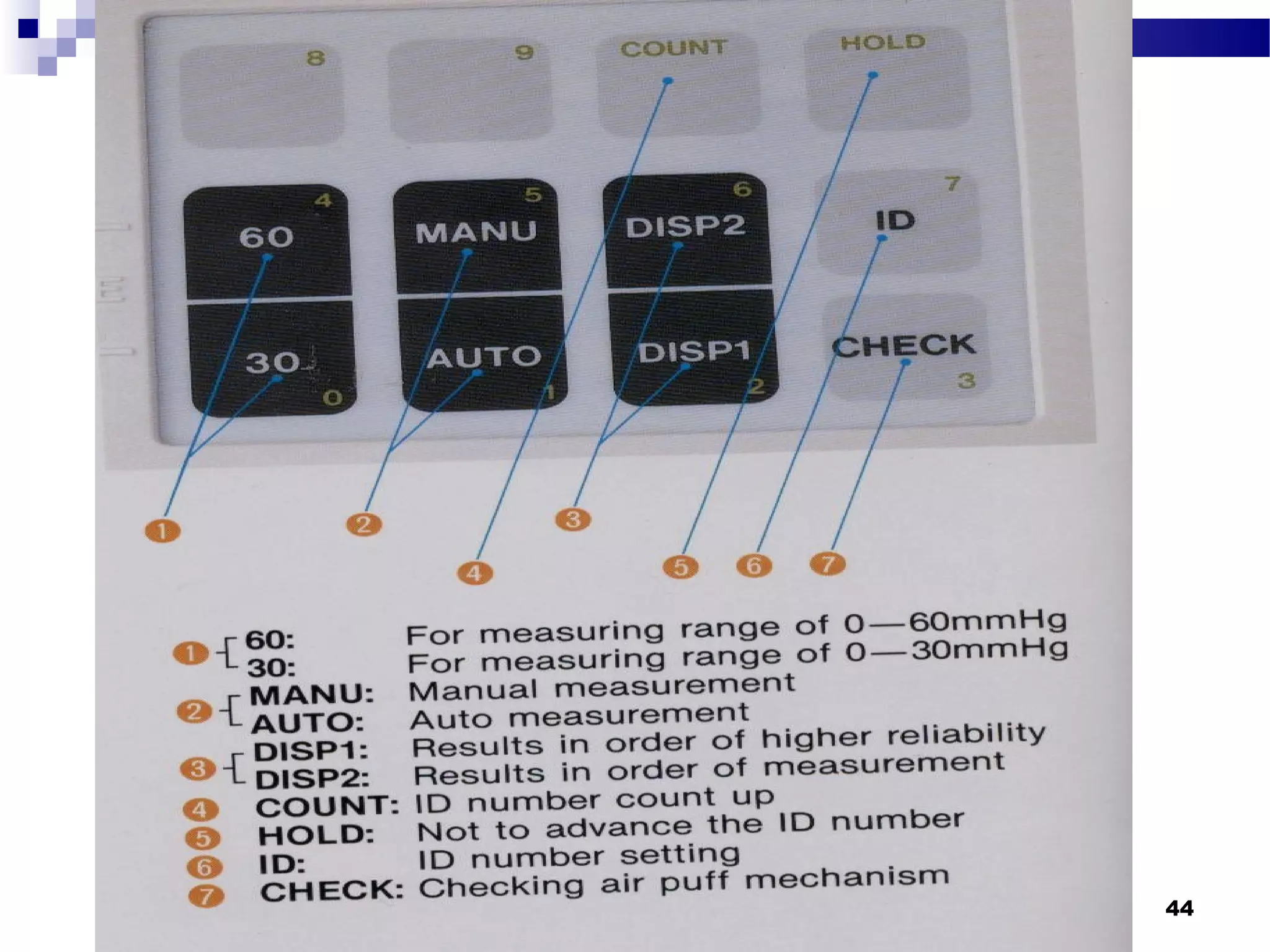
The document discusses various techniques for measuring intraocular pressure (IOP), including Goldmann applanation tonometry, Perkins tonometry, non-contact tonometry, and digital evaluation. Goldmann applanation tonometry is described as the most accurate method. The document provides details on properly using Goldmann tonometry, including preparing the patient, aligning the probe, applying the correct amount of force, and interpreting the results. Contraindications and sources of error are also reviewed.