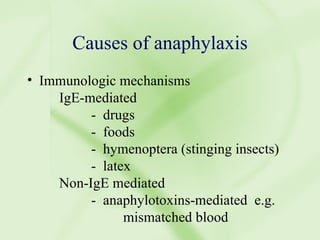
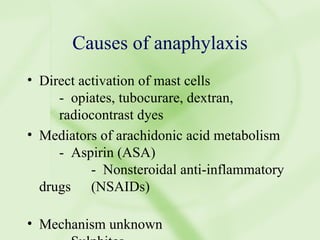
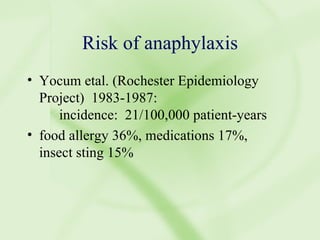
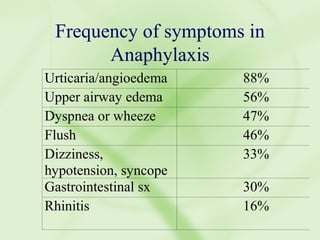
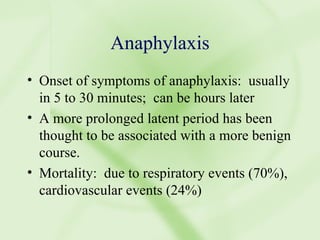
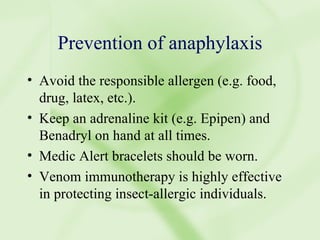
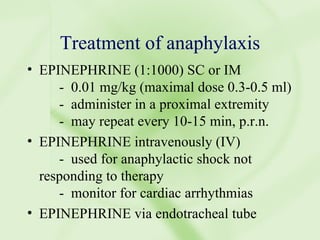
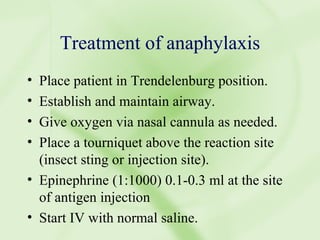
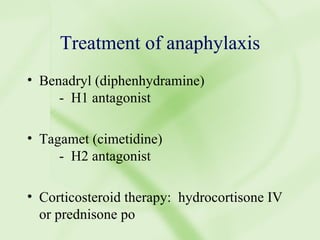
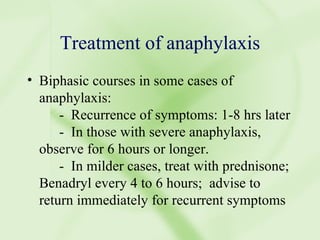
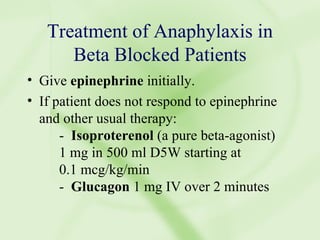
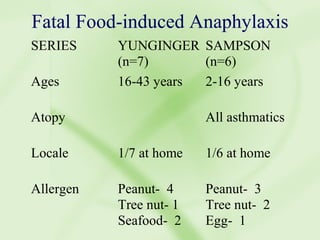
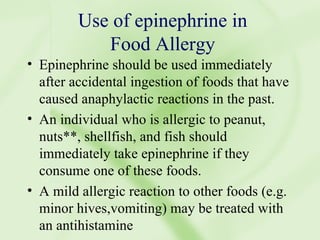
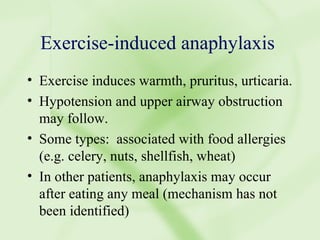
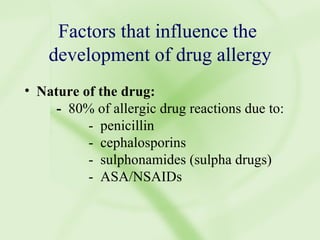
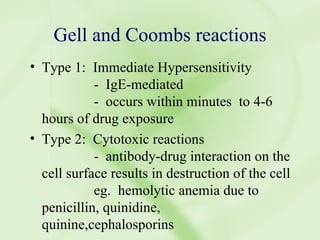
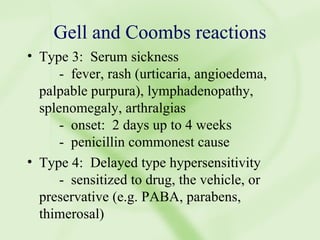
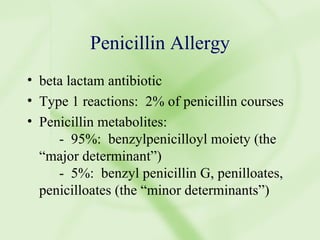
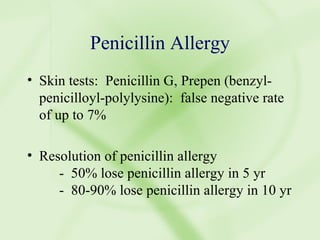
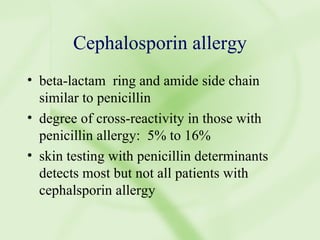
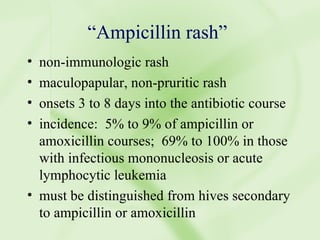
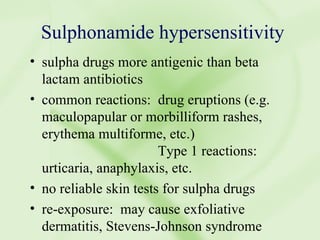
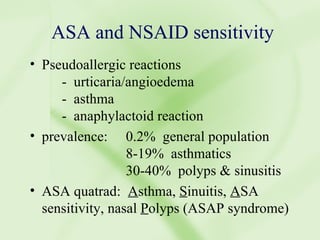
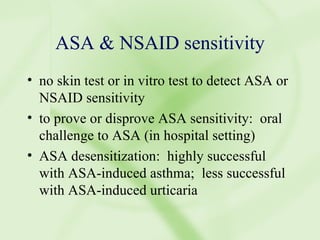
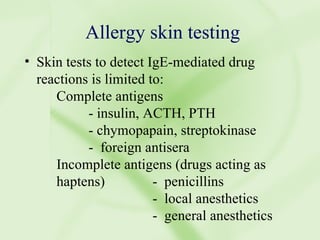
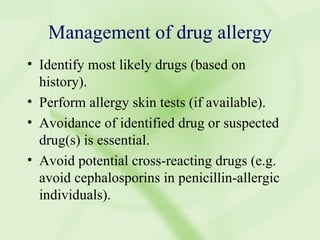
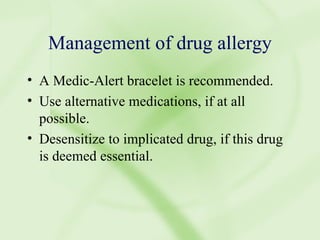
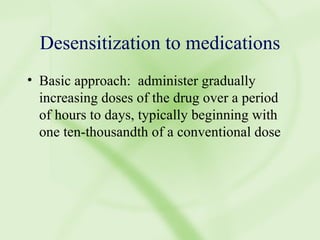
The document discusses anaphylaxis, including its causes, risk factors, symptoms, prevention, and treatment. It causes include IgE-mediated reactions to foods, drugs, insects, as well as non-IgE mediated reactions. Symptom onset is usually within 5-30 minutes. Prevention involves avoiding allergens and carrying epinephrine. Treatment involves epinephrine, antihistamines, corticosteroids, and monitoring for biphasic reactions. Drug allergies can also cause anaphylaxis and involve skin testing to identify culprit drugs when possible. Management includes avoidance, alternative medications, and potential desensitization.