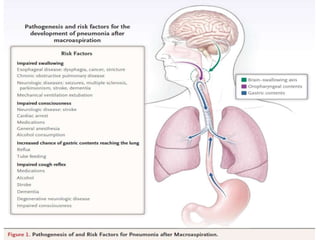
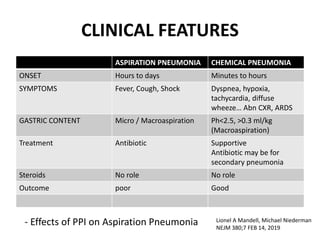
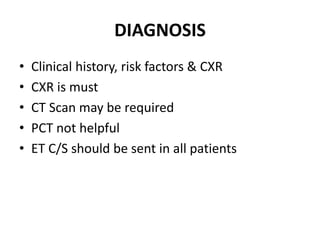
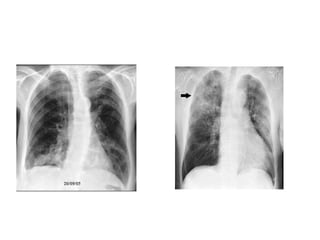
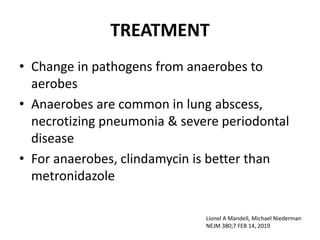
Aspiration pneumonia is caused by bacteria from the mouth or stomach entering the lungs. It can develop hours to days after aspiration occurs. The most common pathogens have changed from anaerobic bacteria to aerobic bacteria. Diagnosis is based on clinical history, risk factors, and chest x-ray. Treatment depends on whether it is community-acquired or hospital-acquired pneumonia. Antibiotics are used but duration depends on severity and response. Preventive measures focus on oral hygiene and early mobilization of high-risk patients like stroke patients.