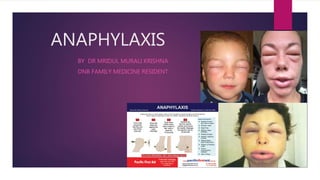
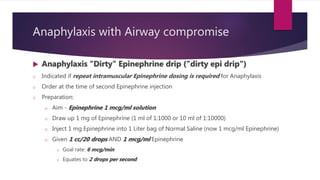
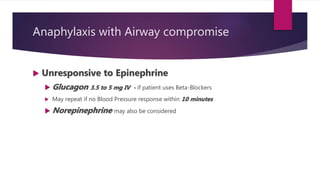
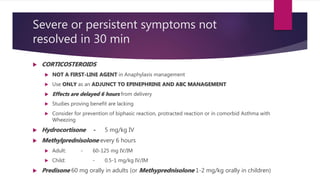
Anaphylaxis is a severe, life-threatening allergic reaction that requires immediate treatment to prevent harm or death. Epinephrine injection is the first-line treatment and should be administered promptly if anaphylaxis criteria are met. Symptoms may involve multiple organ systems such as the skin, respiratory tract, gastrointestinal tract, and cardiovascular system. Precautions must be taken to monitor for potential biphasic reactions in the hours after the initial episode. Strict allergen avoidance and use of medical alert devices can help prevent future dangerous reactions.