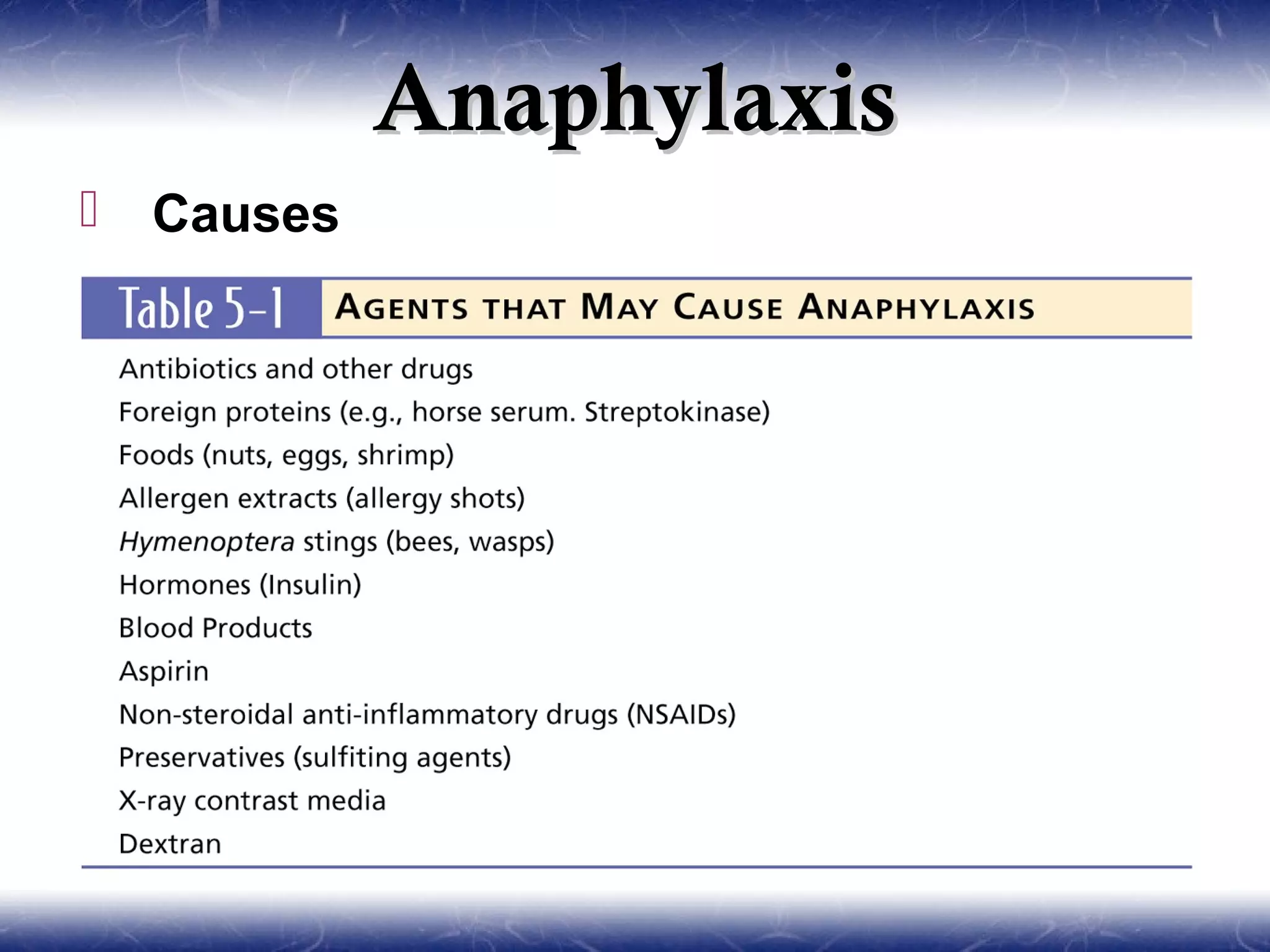
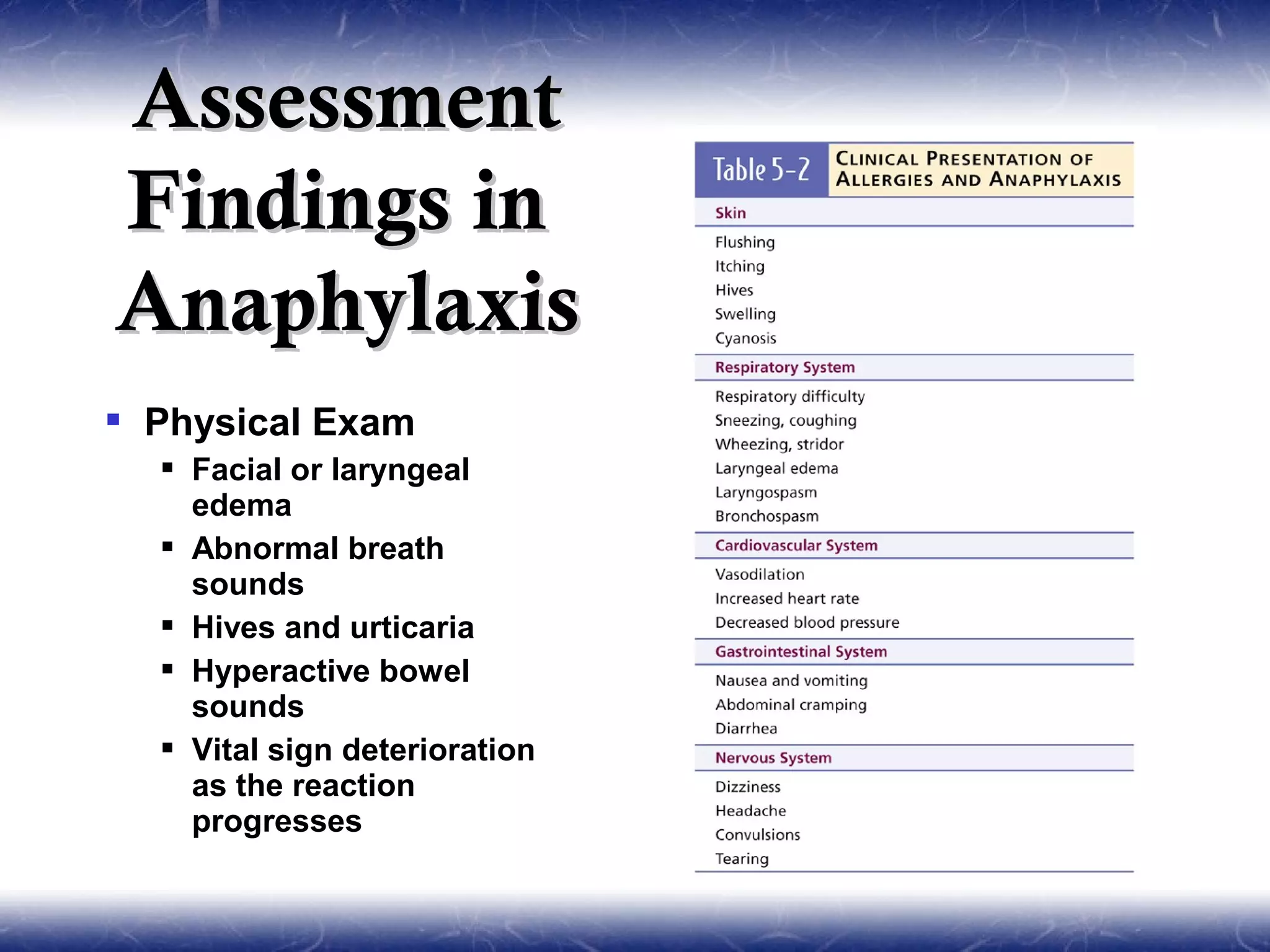
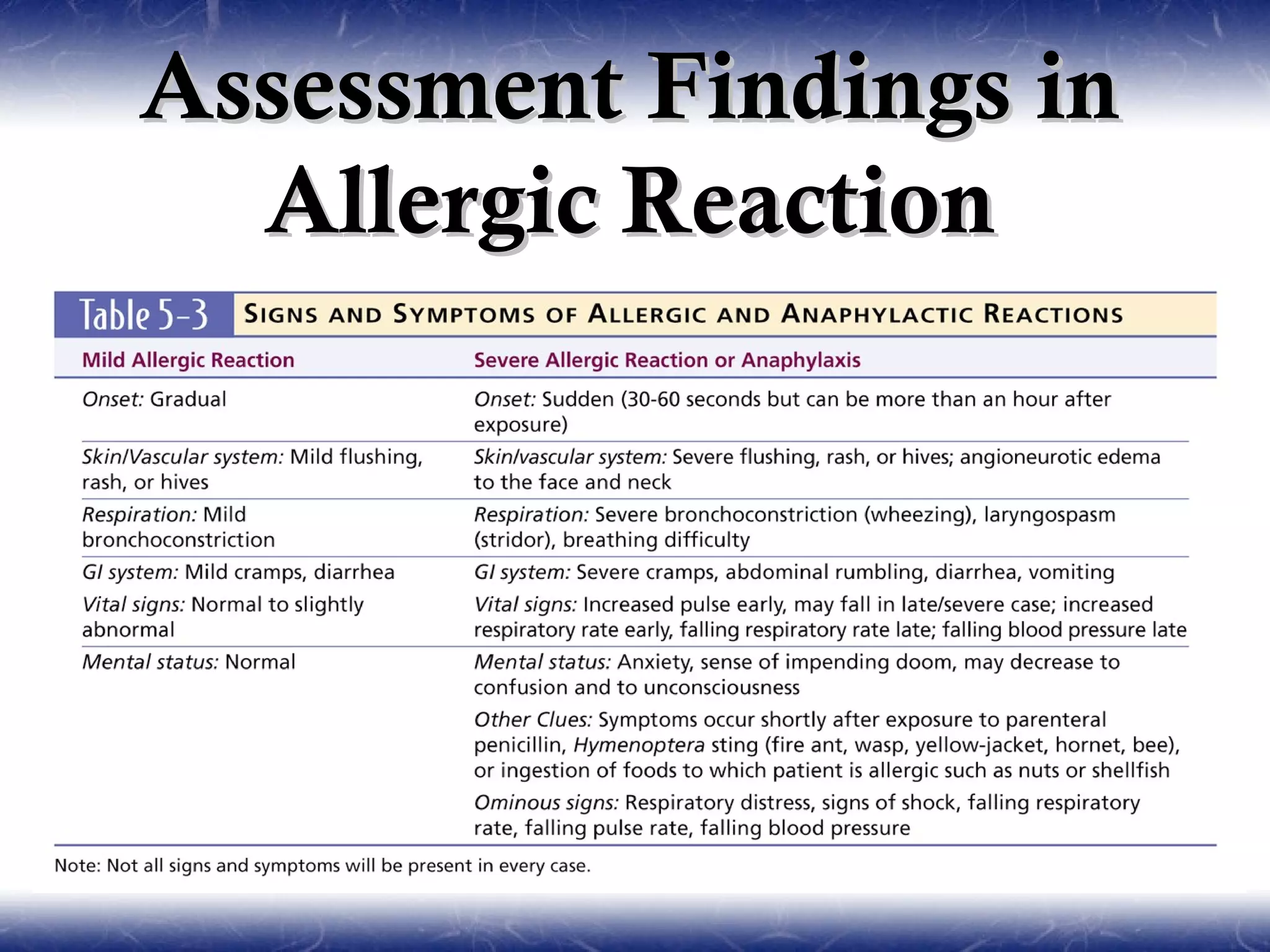
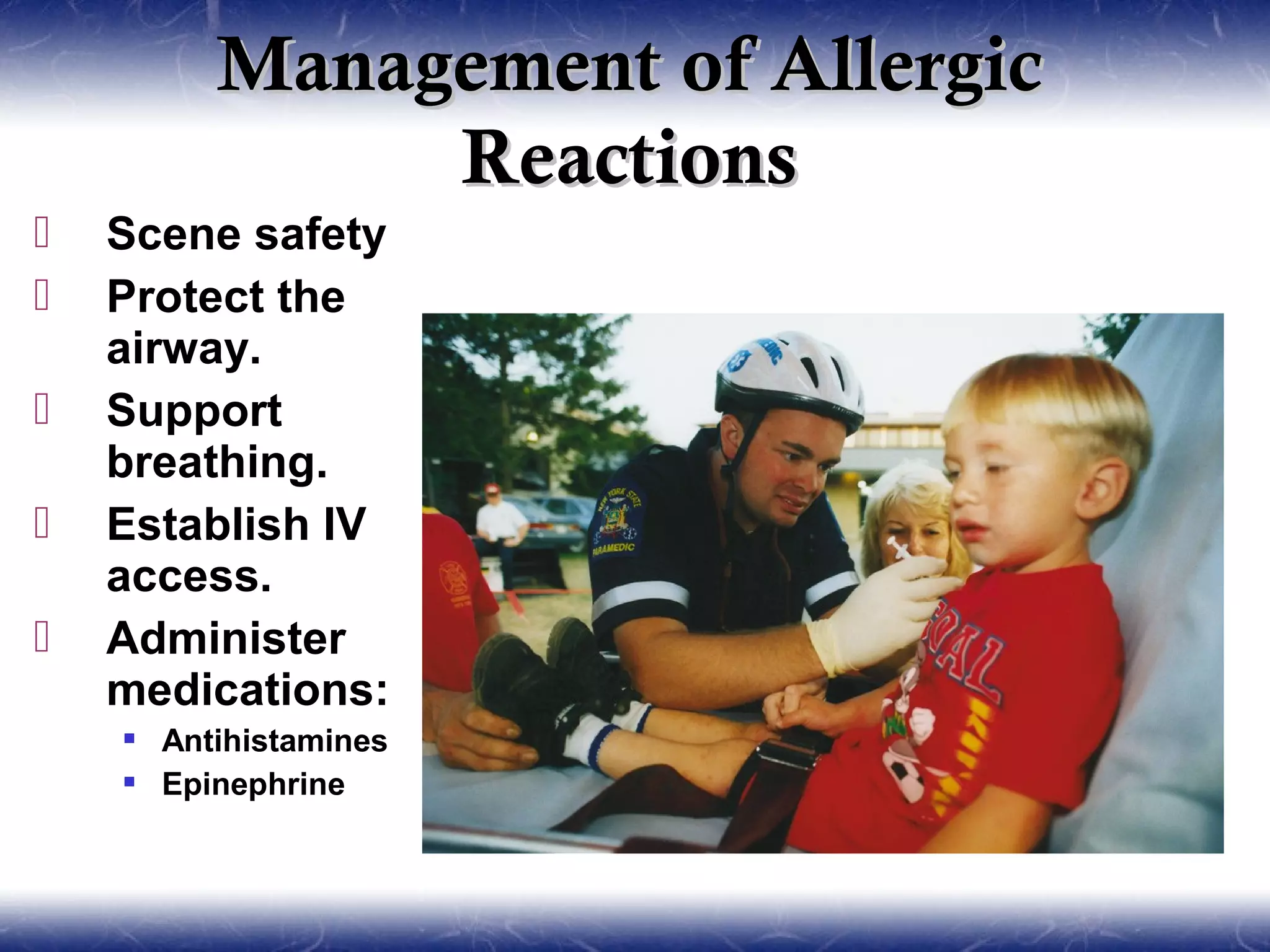
This document discusses allergies and anaphylaxis, including their pathophysiology, assessment findings, and management. It describes anaphylaxis as a life-threatening allergic reaction caused by exposure to an allergen, which results in widespread histamine release and affects multiple body systems. Key treatments for anaphylaxis include epinephrine, antihistamines, corticosteroids, oxygen, IV fluids and airway management. Allergic reactions involve similar symptoms but are typically less severe. Patient education focuses on prevention, recognition of symptoms and self-treatment options.