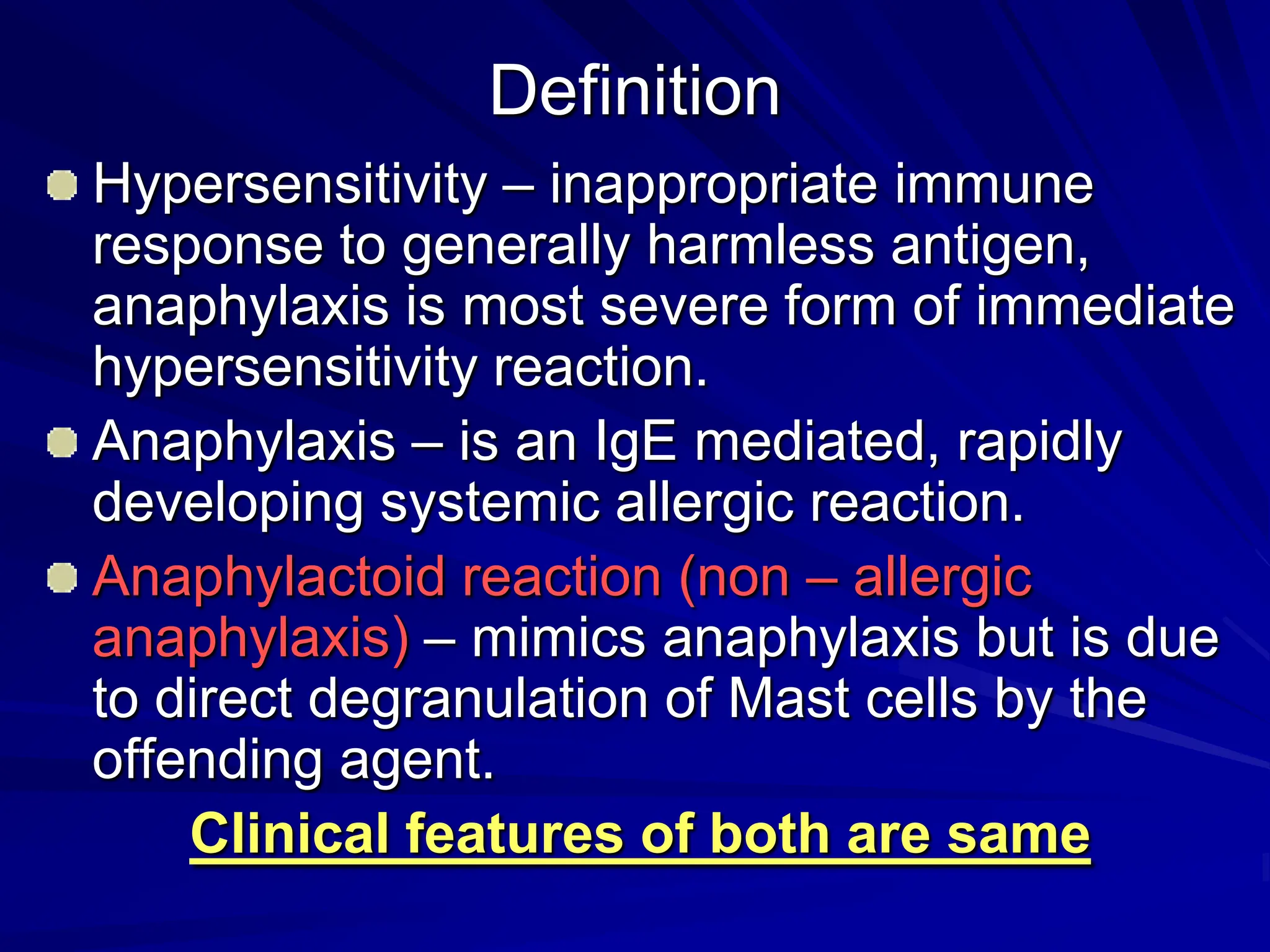
The document defines anaphylaxis as an IgE-mediated, systemic allergic reaction and anaphylactoid reaction as a similar reaction that is non-allergic. It describes the epidemiology, etiology, pathophysiology, clinical features, diagnosis, and treatment of anaphylaxis. Common causes include antibiotics, hymenoptera stings, and foods. Diagnosis involves history and physical exam. Epinephrine is the first-line treatment to reverse symptoms. Prevention strategies include skin testing for IgE-mediated reactions and avoiding triggers for those with a history of allergic reactions.