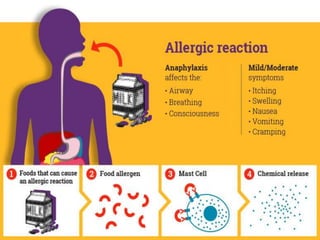
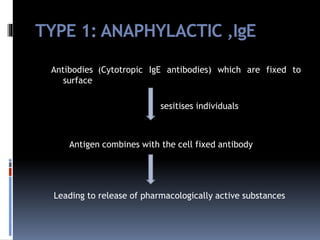
A 4-month-old baby boy presented to the emergency room with vomiting, hives, and cyanosis after his first exposure to a banana. He was diagnosed with anaphylaxis and improved after receiving an epinephrine injection. Skin tests confirmed a banana allergy. While banana is not highly allergenic, food allergies are becoming more common, so banana may need to be considered as a potential allergen for babies presenting with anaphylaxis.