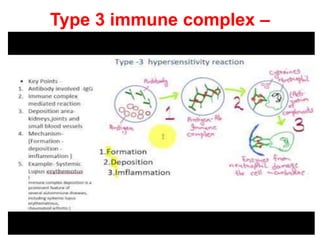
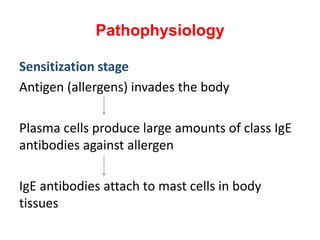
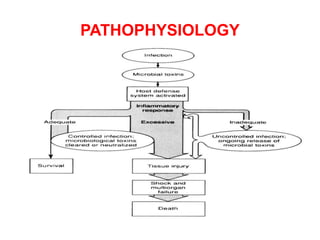
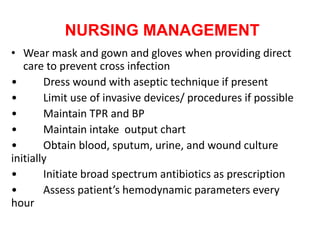
The document discusses different types of hypersensitivity and anaphylaxis. It defines anaphylaxis and describes its incidence, substances that can trigger it, pathophysiology, clinical manifestations, diagnostic evaluation, and management. Nursing management focuses on maintaining airway, supporting circulation, preventing complications, and providing patient education. The document also discusses septicemia, defining it, outlining risk factors, etiology, pathophysiology, clinical signs, diagnostic tests, and treatment including antibiotics and supportive care. Nursing management of septicemia includes infection control, supporting tissue perfusion, and preventing complications.