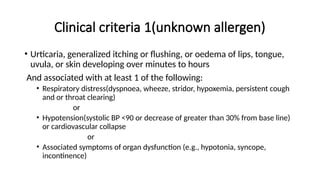
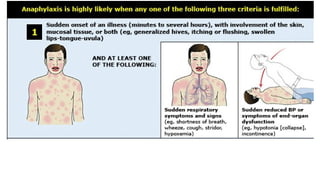
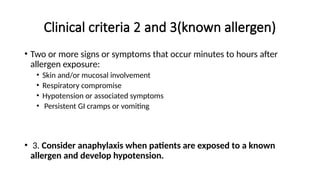
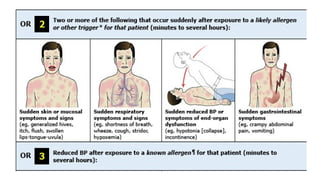
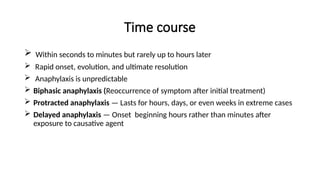
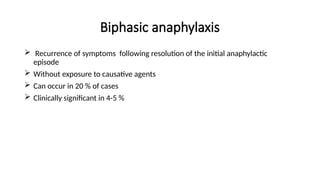
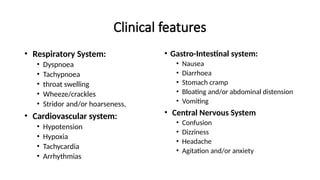
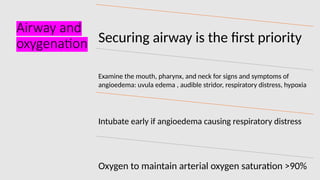
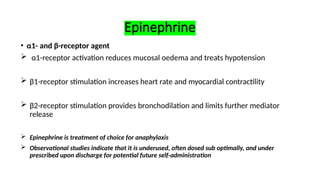
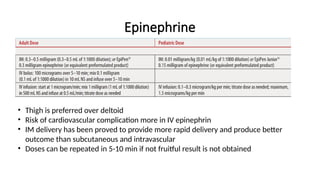
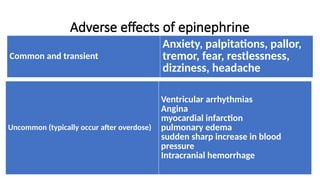
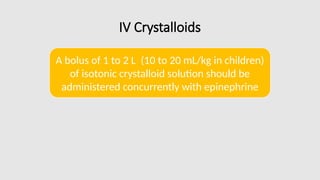
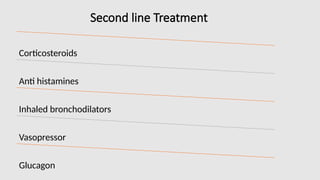
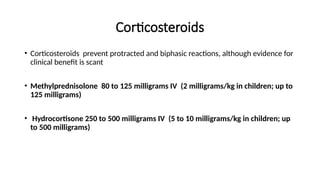
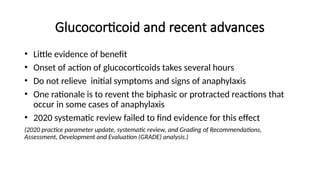
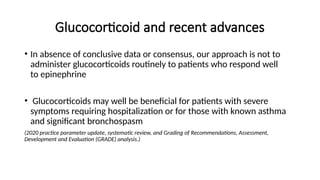
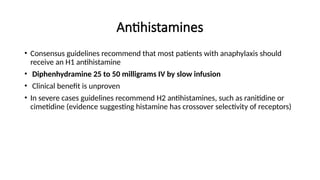
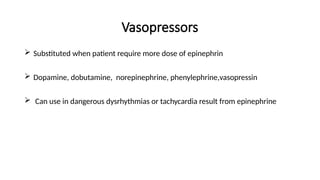
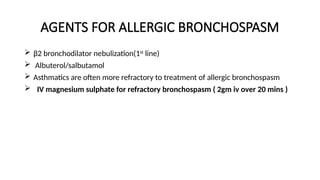
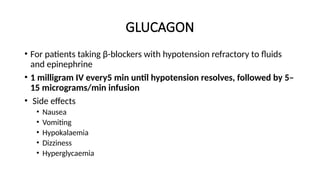
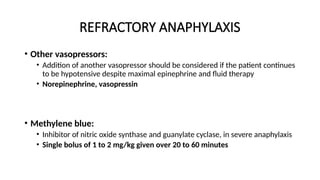
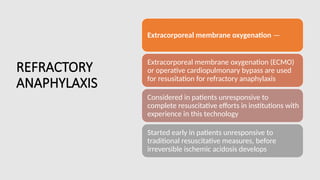
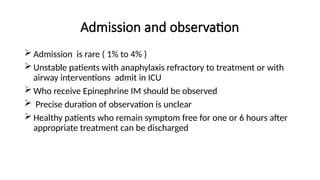
This presentation by Dr. Bishal Sapkota provides a detailed clinical overview of anaphylaxis, a life-threatening allergic reaction. It covers historical background, clinical criteria for diagnosis, time course, common causes, and multi-system clinical manifestations. Special emphasis is placed on emergency management, including the use of epinephrine, second-line treatments like corticosteroids and antihistamines, and approaches for refractory cases. Ideal for medical professionals, emergency responders, and students in healthcare, this resource draws from authoritative texts such as Tintinalli’s Emergency Medicine (9th edition) and UpToDate (2025).