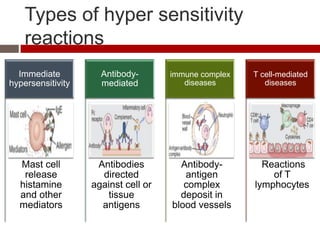
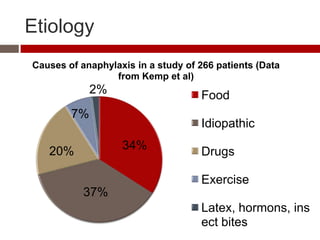
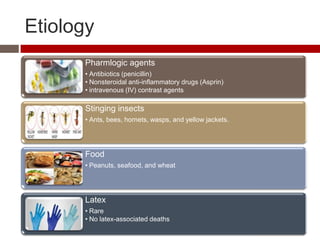
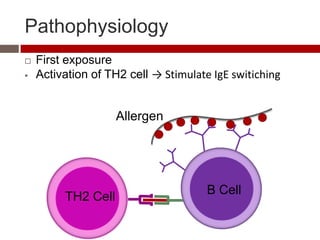
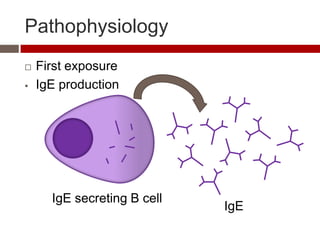
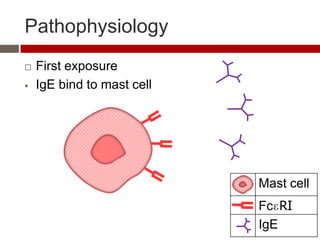
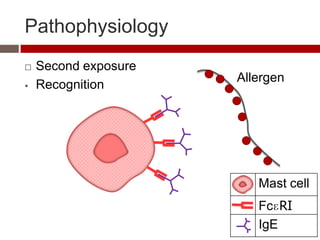
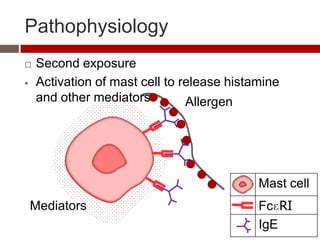
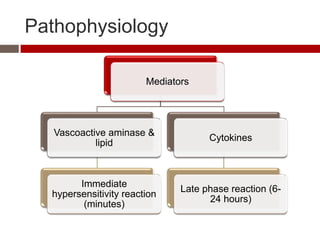
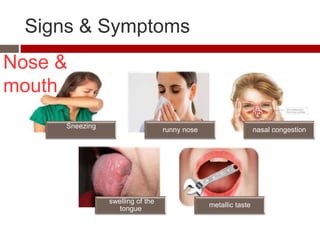
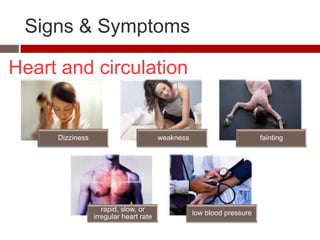
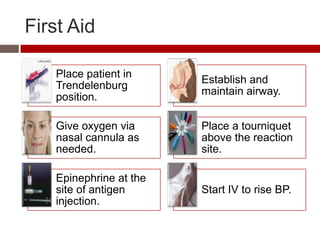
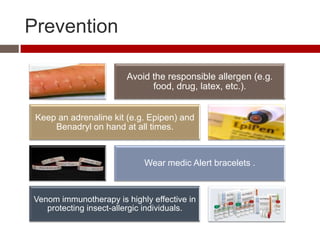
The document discusses anaphylaxis, a severe hypersensitivity reaction affecting multiple body systems, detailing its definitions, causes, pathophysiology, symptoms, diagnosis, and treatment methods. It emphasizes the role of allergens such as food, drugs, and insect stings, and outlines the critical need for immediate intervention, primarily using epinephrine. Additionally, prevention strategies, such as avoiding allergens and maintaining an adrenaline kit, are highlighted.