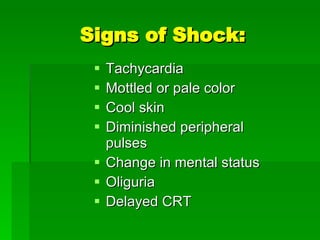
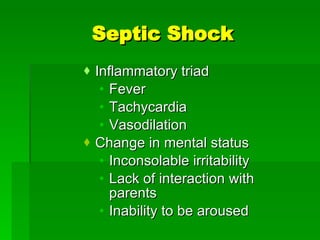
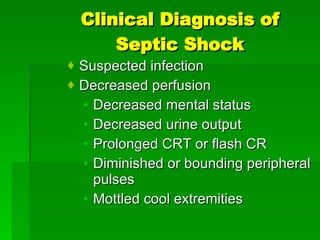
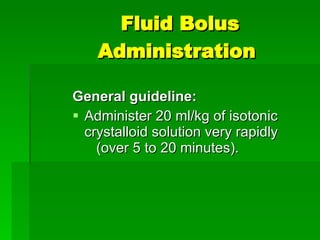
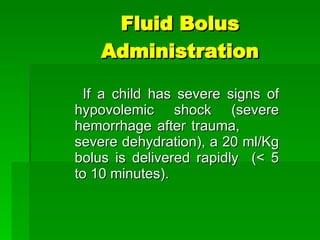
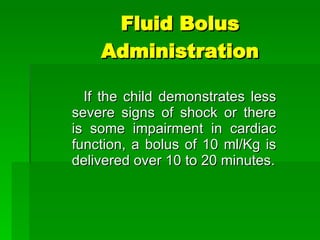
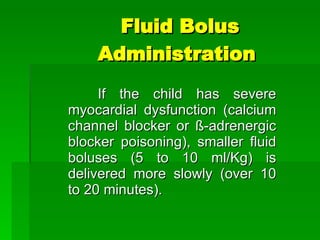
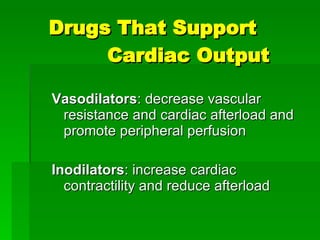
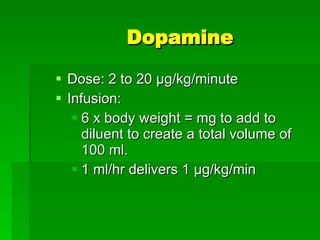
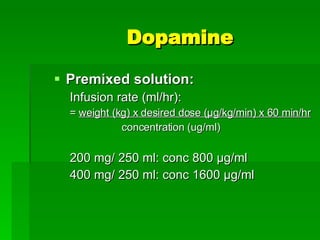
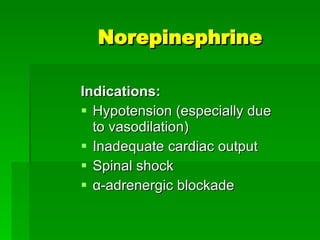
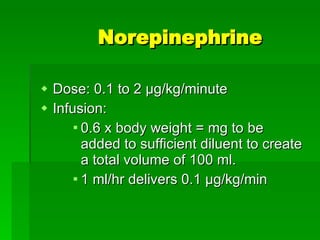
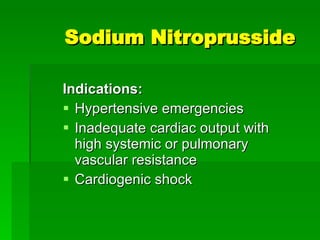
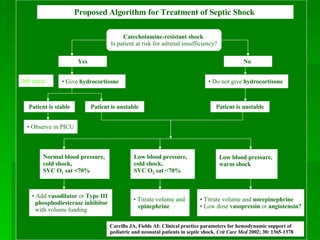
Shock is a clinical state characterized by inadequate tissue perfusion resulting from insufficient oxygen and substrate delivery to meet metabolic demands. There are several types of shock defined by etiology (hypovolemic, cardiogenic, distributive) and effects on blood pressure (compensated, decompensated). Signs of shock include tachycardia, altered mental status, and decreased urine output. Treatment involves rapid fluid resuscitation and vasoactive drugs like dopamine, epinephrine, and norepinephrine to support cardiac output as needed.