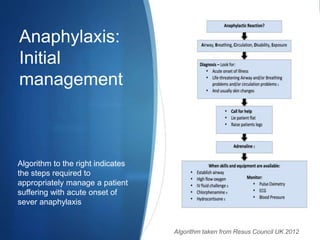
Anaphylaxis is a severe allergic reaction that can be life-threatening. It requires rapid identification, assessment, and on-scene management including epinephrine, oxygen, IV fluids, and transport to the emergency department. Proper treatment of anaphylaxis in the pre-hospital setting is vital to ensure positive patient outcomes.