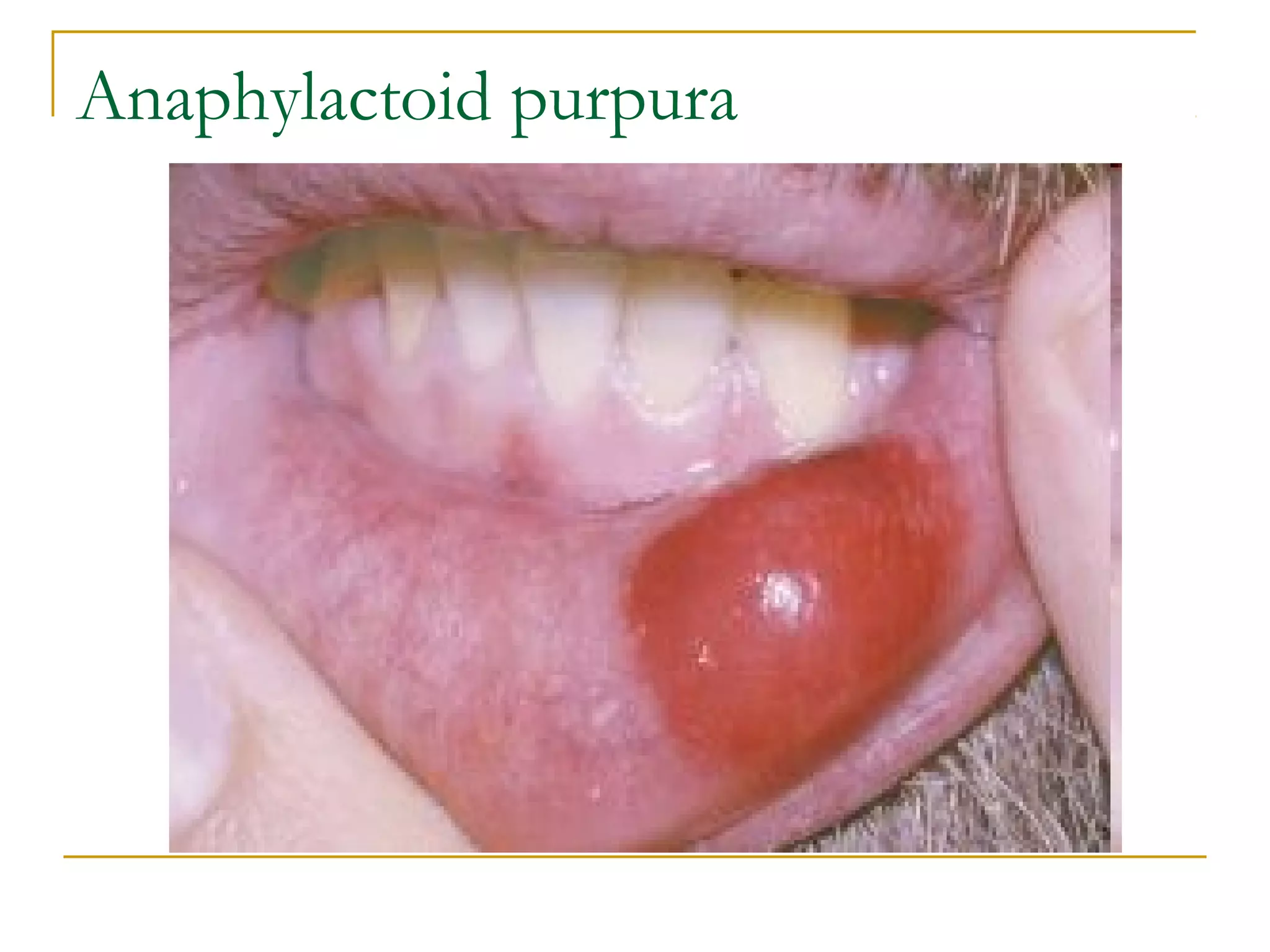
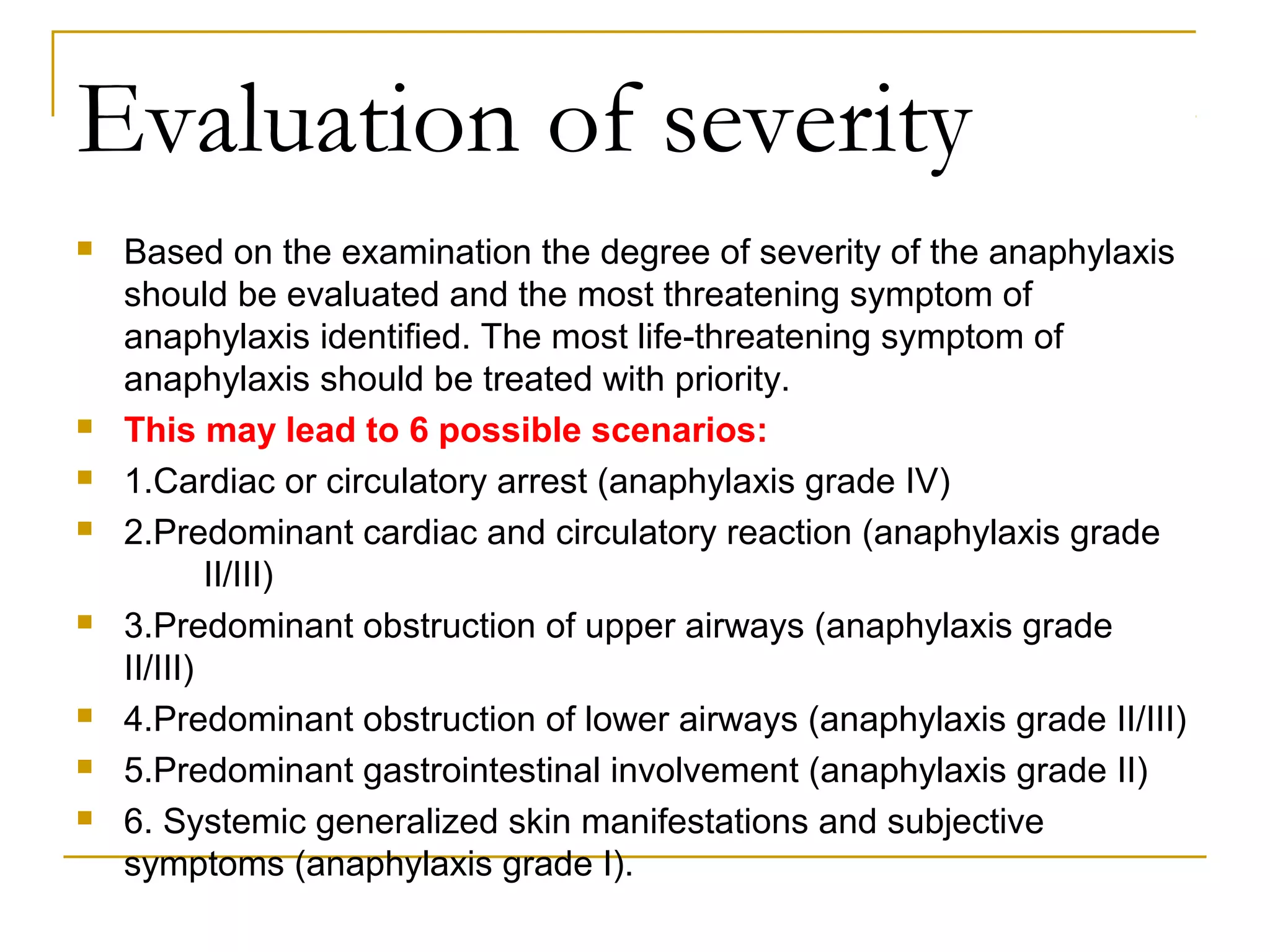
This document provides information about anaphylaxis including its definition, types, causes, signs and symptoms, evaluation, treatment, and prognosis. Anaphylaxis is a severe, potentially life-threatening allergic reaction affecting multiple body systems. It can be triggered by foods, medications, insect stings, or latex. Treatment involves epinephrine, fluids, airway management, oxygen, antihistamines, steroids, and monitoring for biphasic reactions. Refractory anaphylaxis may require vasopressors, methylene blue, or extracorporeal membrane oxygenation. Prognosis is generally excellent if the trigger can be avoided.