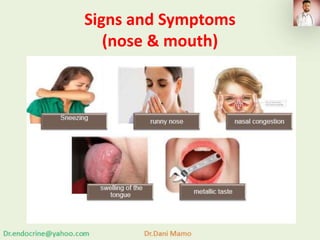
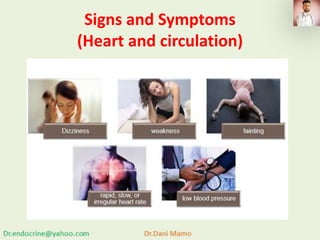
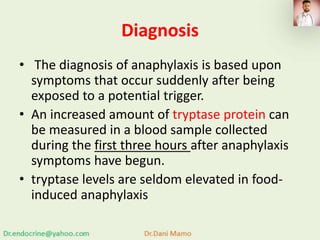
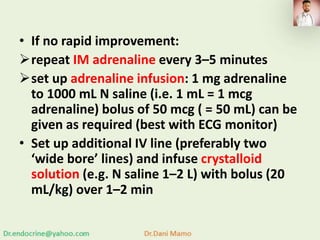
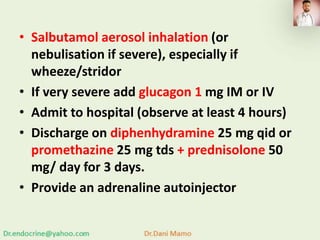
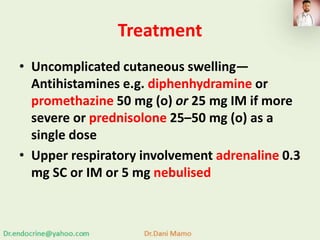
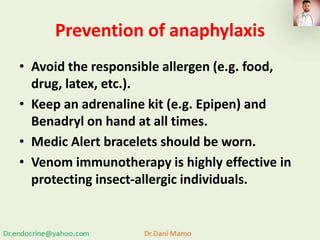
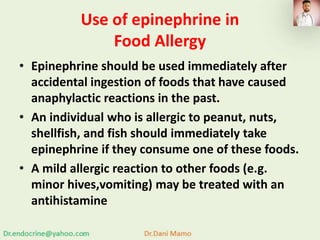
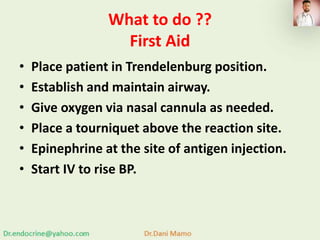
Anaphylaxis is a severe, potentially fatal allergic reaction characterized by rapid onset symptoms such as itching, hives, difficulty breathing, and circulatory issues, often triggered by allergens like insect stings, medications, or specific foods. Diagnosis occurs through observed symptoms and tryptase protein levels, with immediate treatment involving adrenaline and supportive care. Preventative measures include allergen avoidance, carrying an epinephrine autoinjector, and, in some cases, venom immunotherapy.