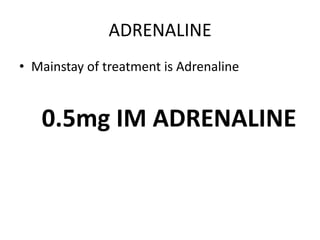
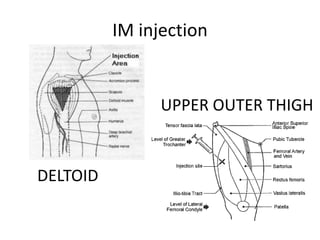
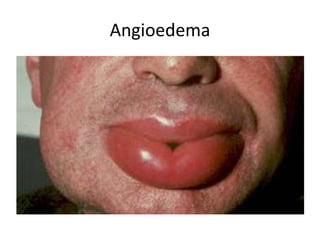
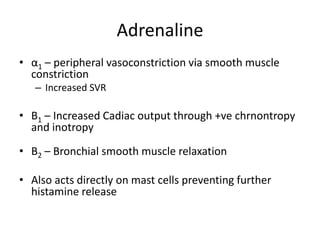
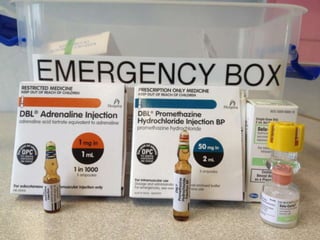
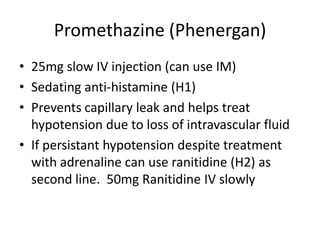
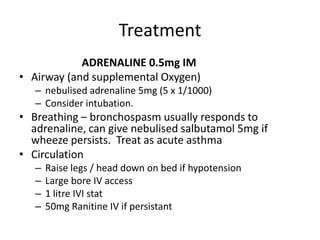
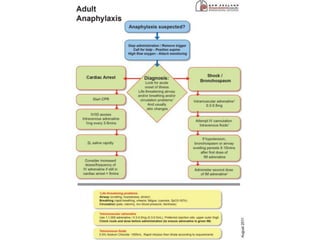
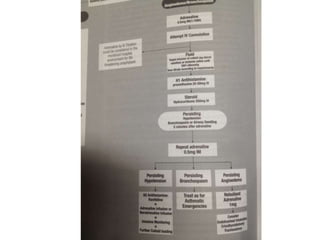
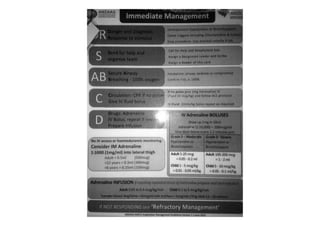
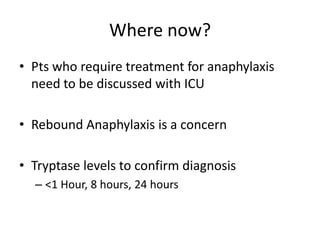
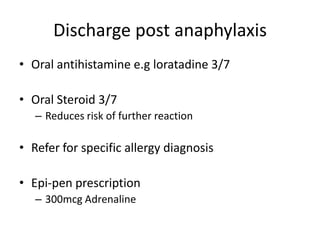
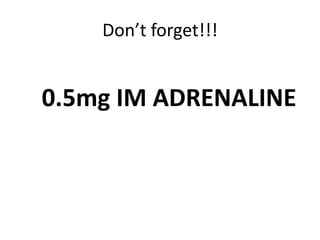
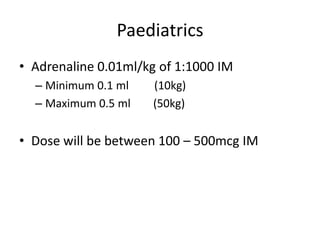
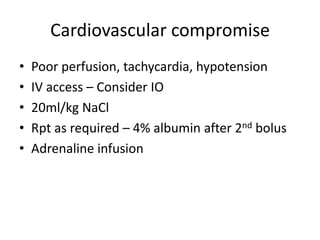
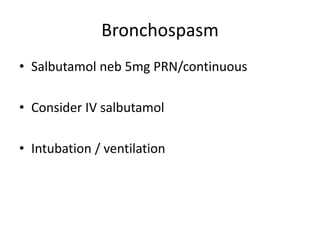
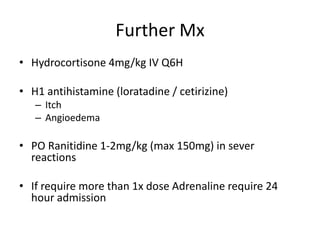
This document provides information on the treatment of anaphylaxis. It begins by defining anaphylaxis as an acute hypersensitivity reaction and describes the pathophysiology involving the release of histamine. The mainstay treatment is identified as adrenaline (epinephrine) injected intramuscularly. Common causes and signs/symptoms are outlined involving the airways, breathing and circulation. Additional treatment steps are described including IV fluids, antihistamines, steroids, and monitoring. Guidance is provided on discharge instructions and managing pediatric cases.