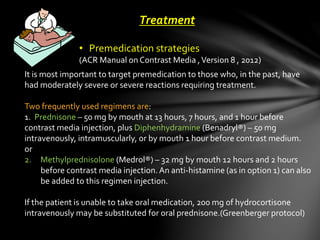
1. Premedication for contrast reactions involves administering prednisone and diphenhydramine prior to the procedure. Methylprednisolone can also be used. For severe cases, hydrocortisone may be given intravenously.
2. In evaluating a contrast reaction, the patient's appearance, speech, breathing, pulse, and blood pressure should be assessed to determine the severity and type of reaction.
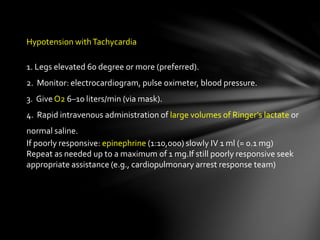
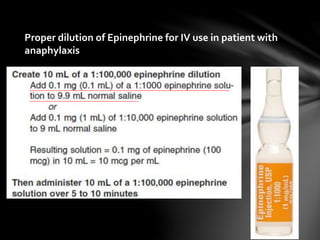
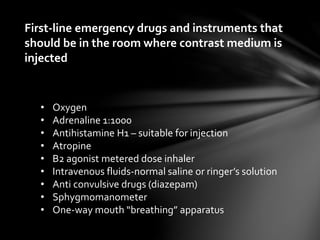
3. Treatment for acute reactions includes epinephrine for hives or facial/laryngeal edema. Hypotension is treated with fluids and epinephrine, while bradycardia may require atropine. Oxygen is also provided.