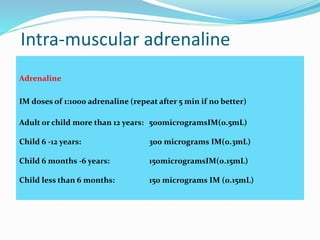
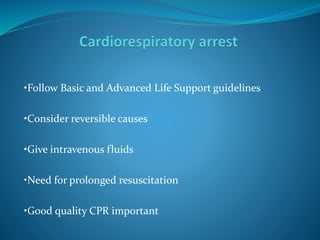
Anaphylaxis is a severe, life-threatening allergic reaction characterized by rapidly developing symptoms that affect the airway, breathing, and circulation. It is usually caused by exposure to an allergen that triggers an immune response involving immunoglobulin E (IgE) antibodies. Common triggers include stings, nuts, foods, medications, and latex. Treatment involves rapidly assessing the airway, breathing, circulation, disability, and exposure, administering epinephrine, supplemental oxygen, intravenous fluids, antihistamines, and corticosteroids, and monitoring the patient closely. Prompt recognition and treatment of anaphylaxis is critical in preventing fatalities.