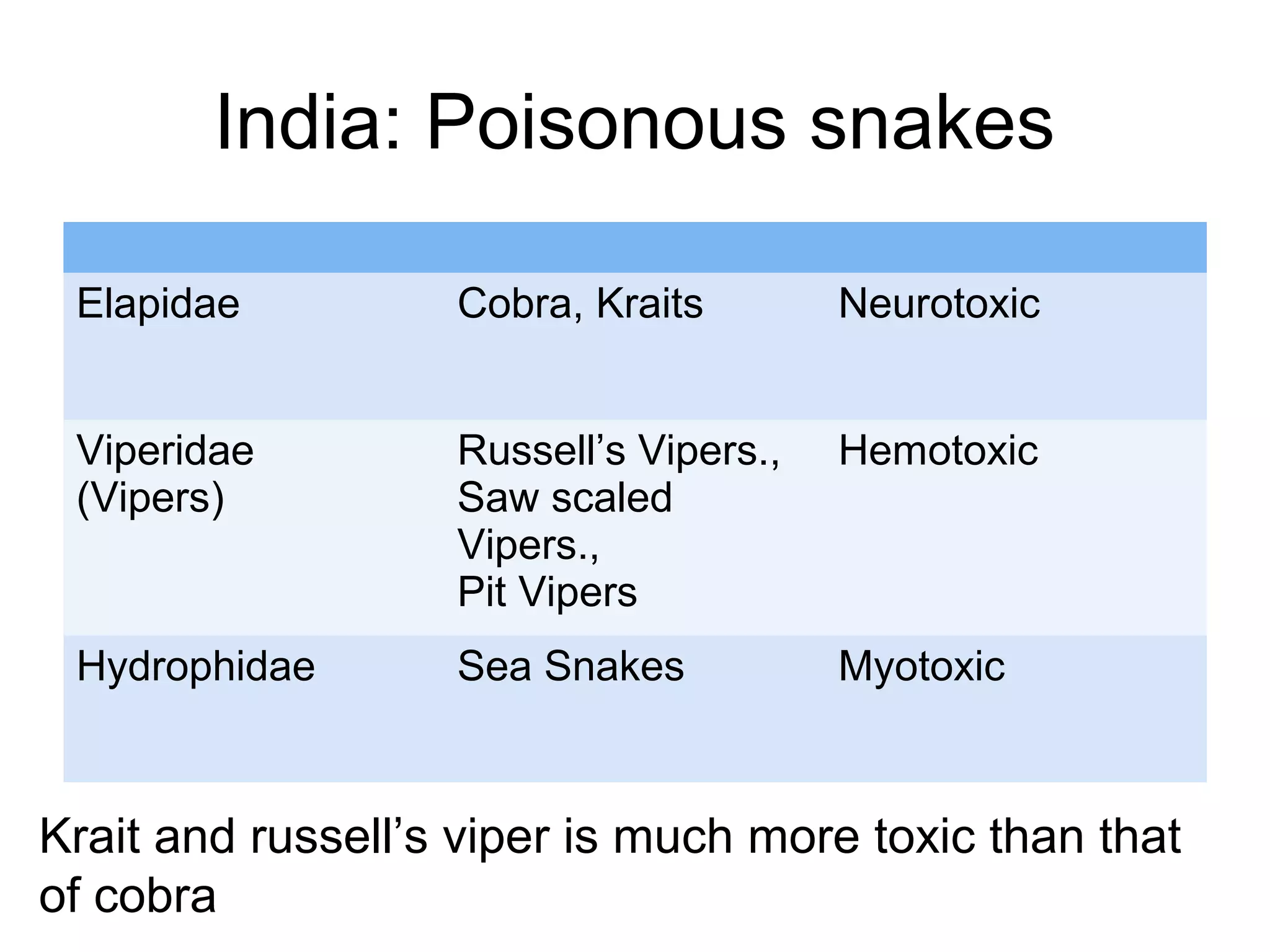
This document provides information about snake bites in India. It notes that India has an estimated 200,000 snake bites per year resulting in 35,000-50,000 deaths. The four most dangerous venomous snakes in India are the common cobra, Russell's viper, saw-scaled viper, and common krait. Snake venom contains various toxins that can cause neurotoxic, hemotoxic, or cytotoxic effects depending on the species. Proper first aid includes reassuring the victim, immobilizing the bitten area, seeking immediate medical care, and informing doctors of any symptoms. Antivenom is the primary treatment and works by neutralizing free venom, with lyophilized antivenom administered via intravenous injection or infusion.











































![Anti-snake venom (ASV)
• Anti-snake venom (ASV)is the mainstay of treatment.
Antivenom is immunoglobulin [usually pepsin-refined F(ab’)2
fragment of whole IgG] purified from the plasma of a horse,
mule or donkey (equine) or sheep (ovine) that has been
immunized with the venoms of one or more species of snake.
• In India, polyvalent ASV, i.e. effective against all the four
common species; Russell’s viper, common cobra, common
Krait and saw-scaled Viper and no monovalent ASVs are
available](https://image.slidesharecdn.com/snakebite-180727162557/75/Snake-bite-in-pediatrics-51-2048.jpg)























