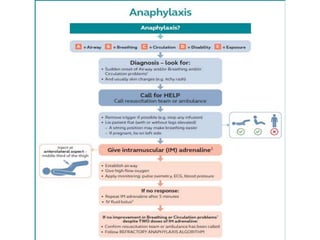
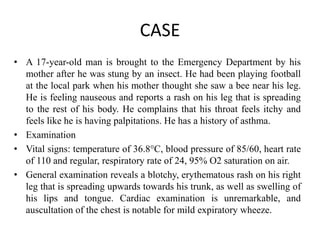
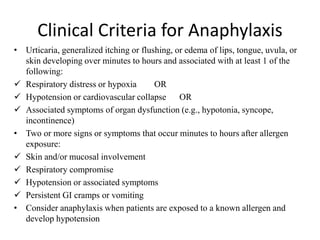
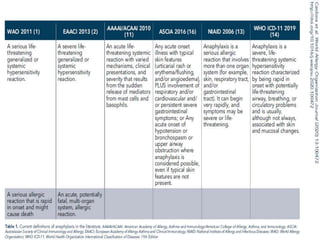
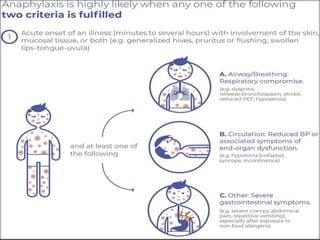
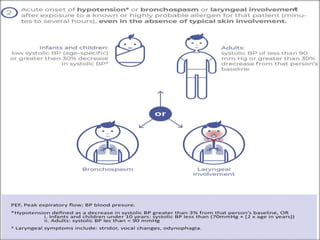
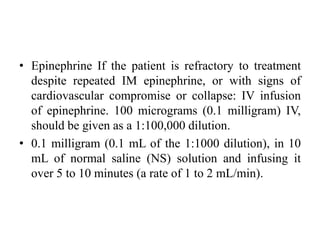
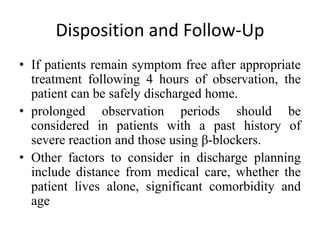
A 17-year-old boy presents with symptoms consistent with anaphylaxis following an insect sting, including a spreading rash, nausea, and respiratory distress. Diagnosis is based on clinical criteria that include skin involvement and hypotension, and management focuses on immediate administration of epinephrine, airway management, and fluid resuscitation. Post-treatment, observation is necessary to monitor for biphasic reactions, and discharge planning involves patient education on allergen avoidance and use of an epinephrine auto-injector.























![• Patients with anaphylactic reactions should be
offered educational options [e.g., Web sites]
advice on advocacy groups, and education
regarding food contamination for food
allergies, and encouraged to wear personal
identification of this condition (e.g.,
MedicAlert ® bracelets).
• β-blocker should be changed.](https://image.slidesharecdn.com/anaphylaxiskeyurbhimani2-240706104702-efe53b0b/85/ANAPHYLAXIS-KEYUR-BHIMANI-anaphylaxispptx-46-320.jpg)