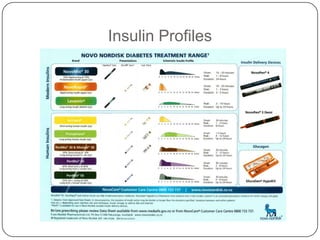
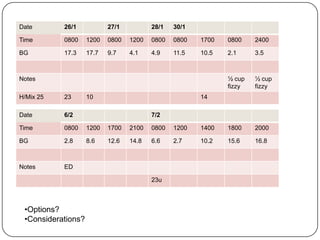
This document describes several clinical scenarios involving patients with diabetes. The first scenario describes a 42-year-old Māori man presenting with hyperglycemic hyperosmolar syndrome. The second discusses an 80-year-old man with unstable blood sugars on his current insulin regimen. The third involves a 20-year-old man newly diagnosed with latent autoimmune diabetes of adults. The fourth outlines a 69-year-old man with unstable blood sugars while tapering prednisone. Each scenario provides background on the patient's history and current treatment, with blood glucose readings and considerations for modifying insulin therapy.