The document discusses advanced mechanical ventilation techniques including:
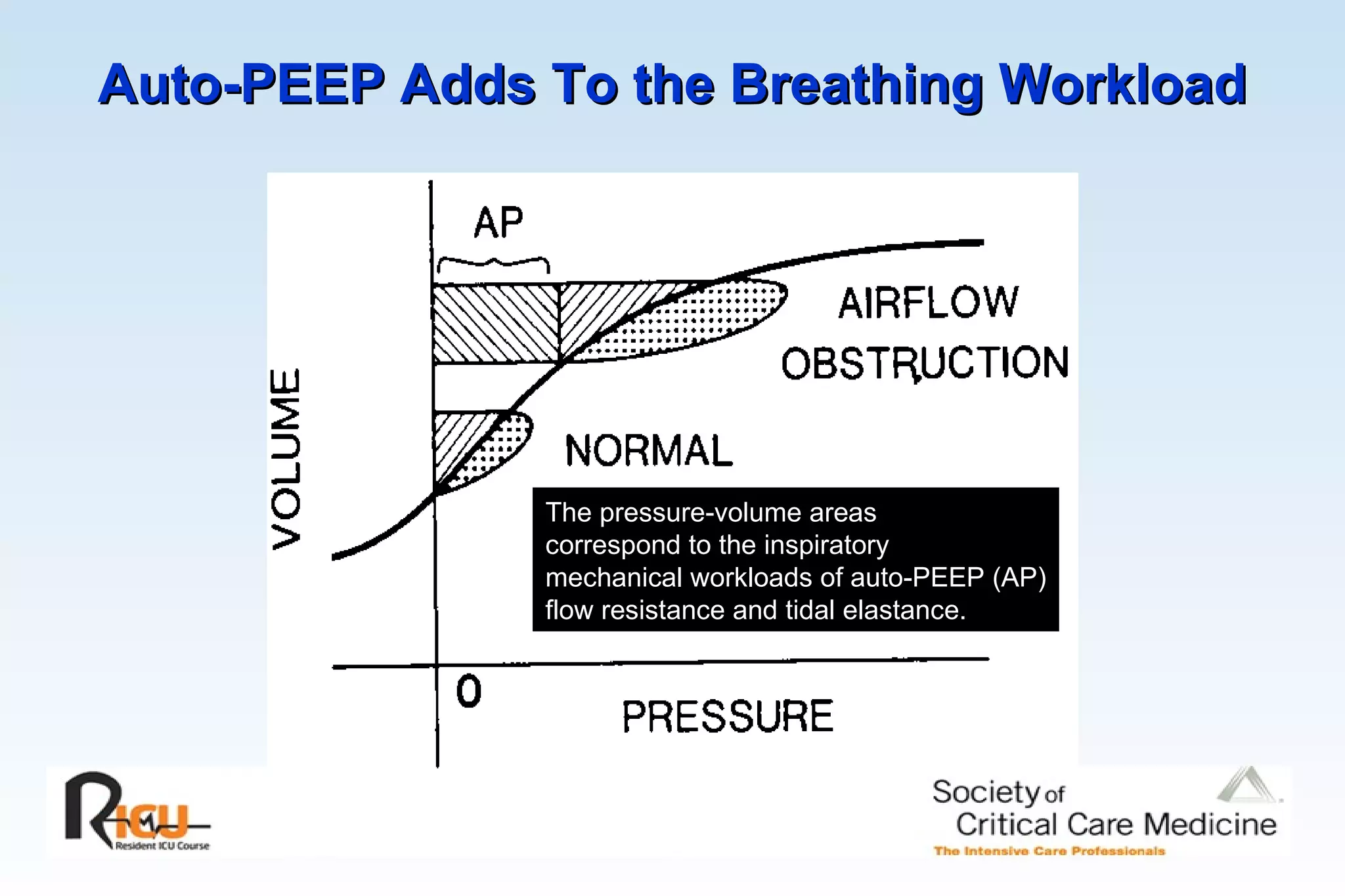
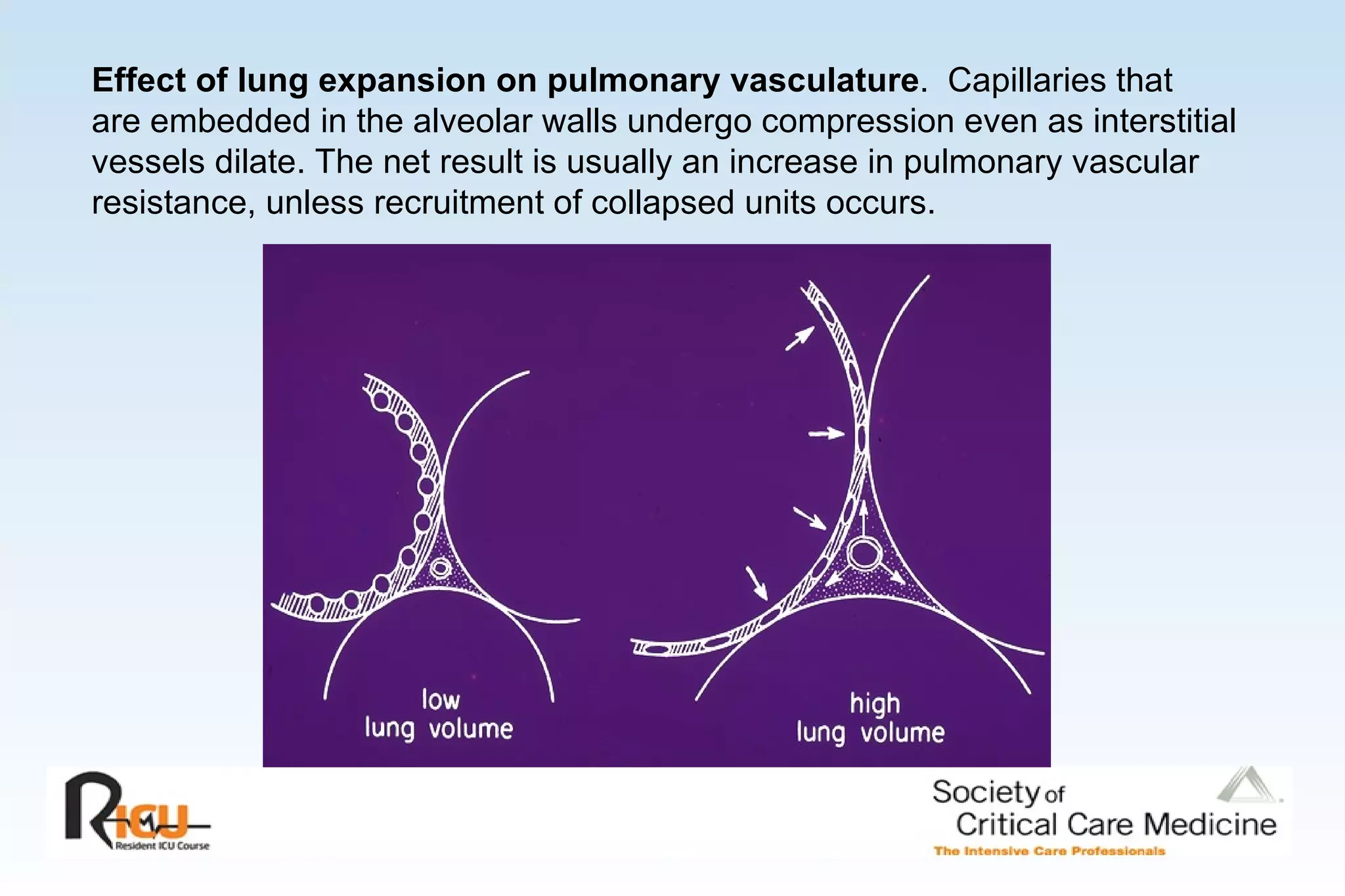
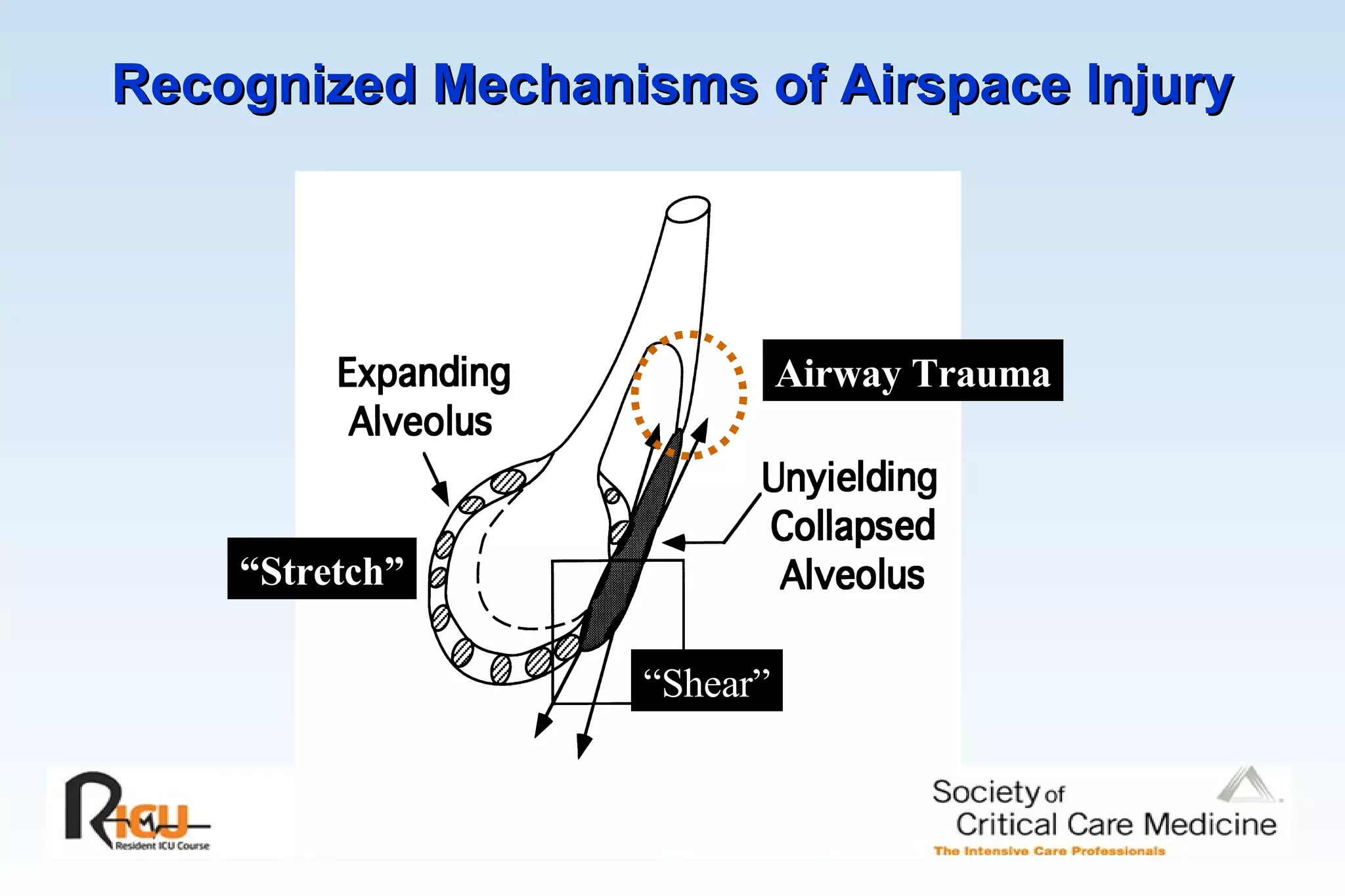
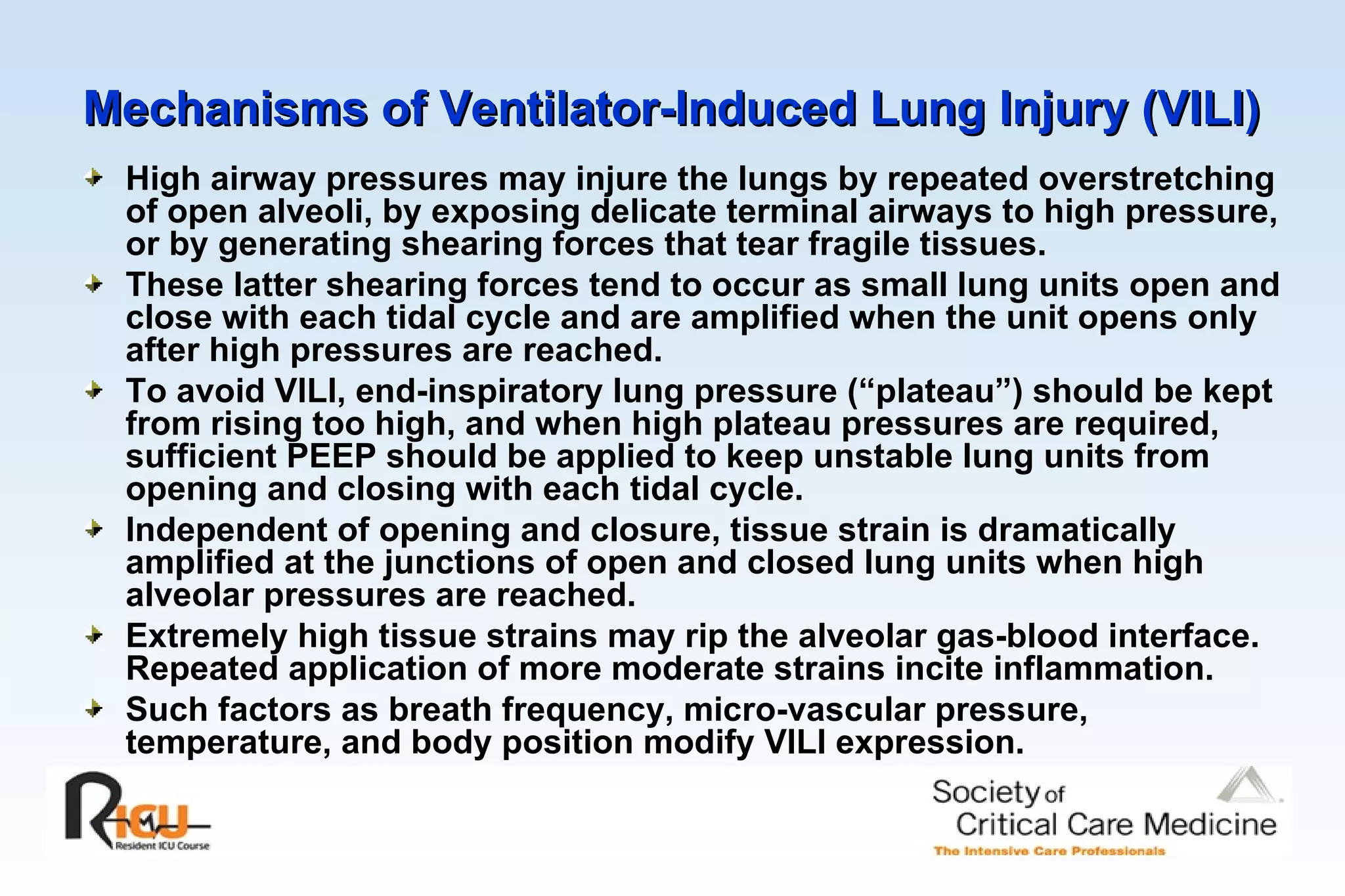
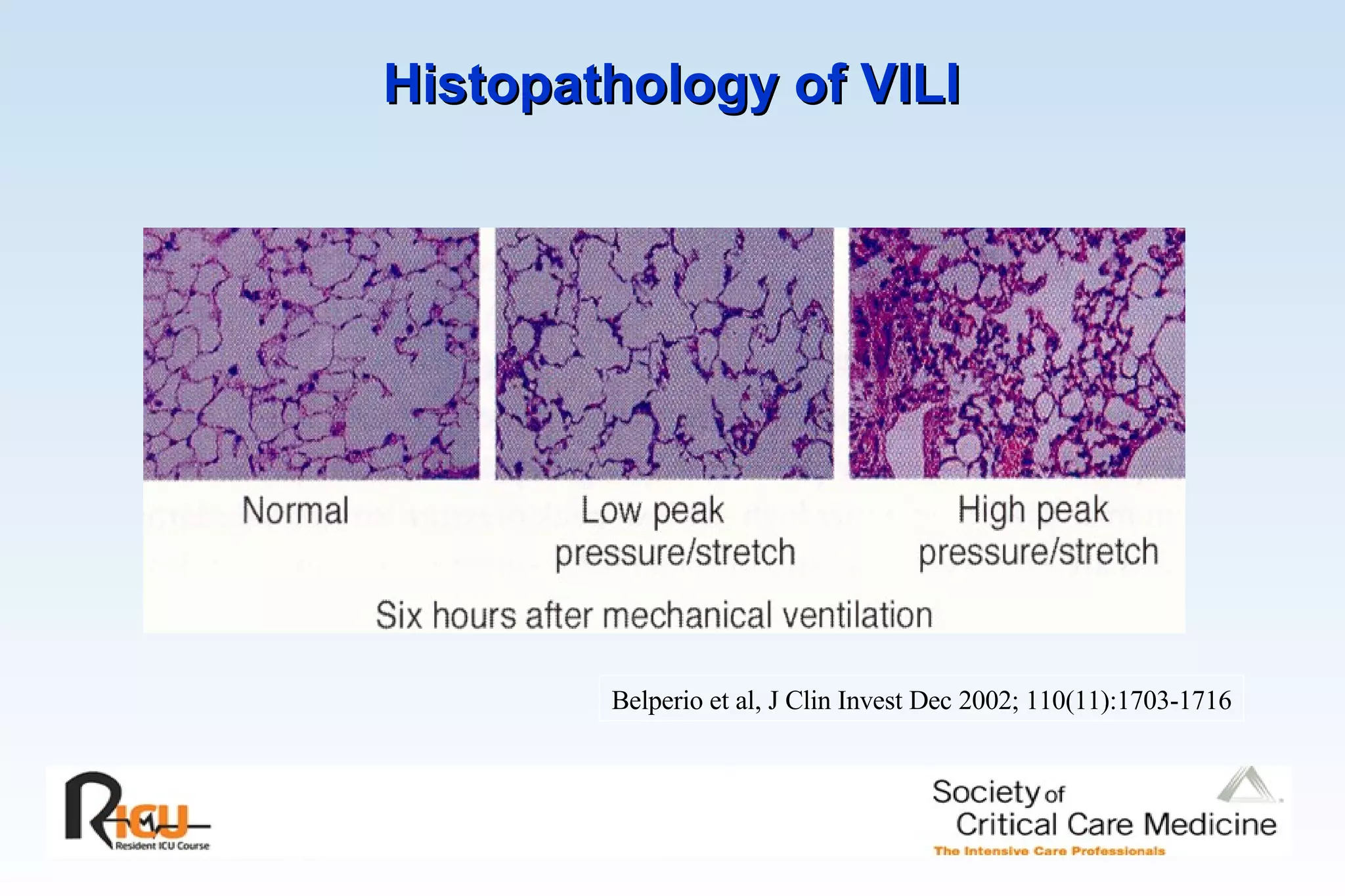
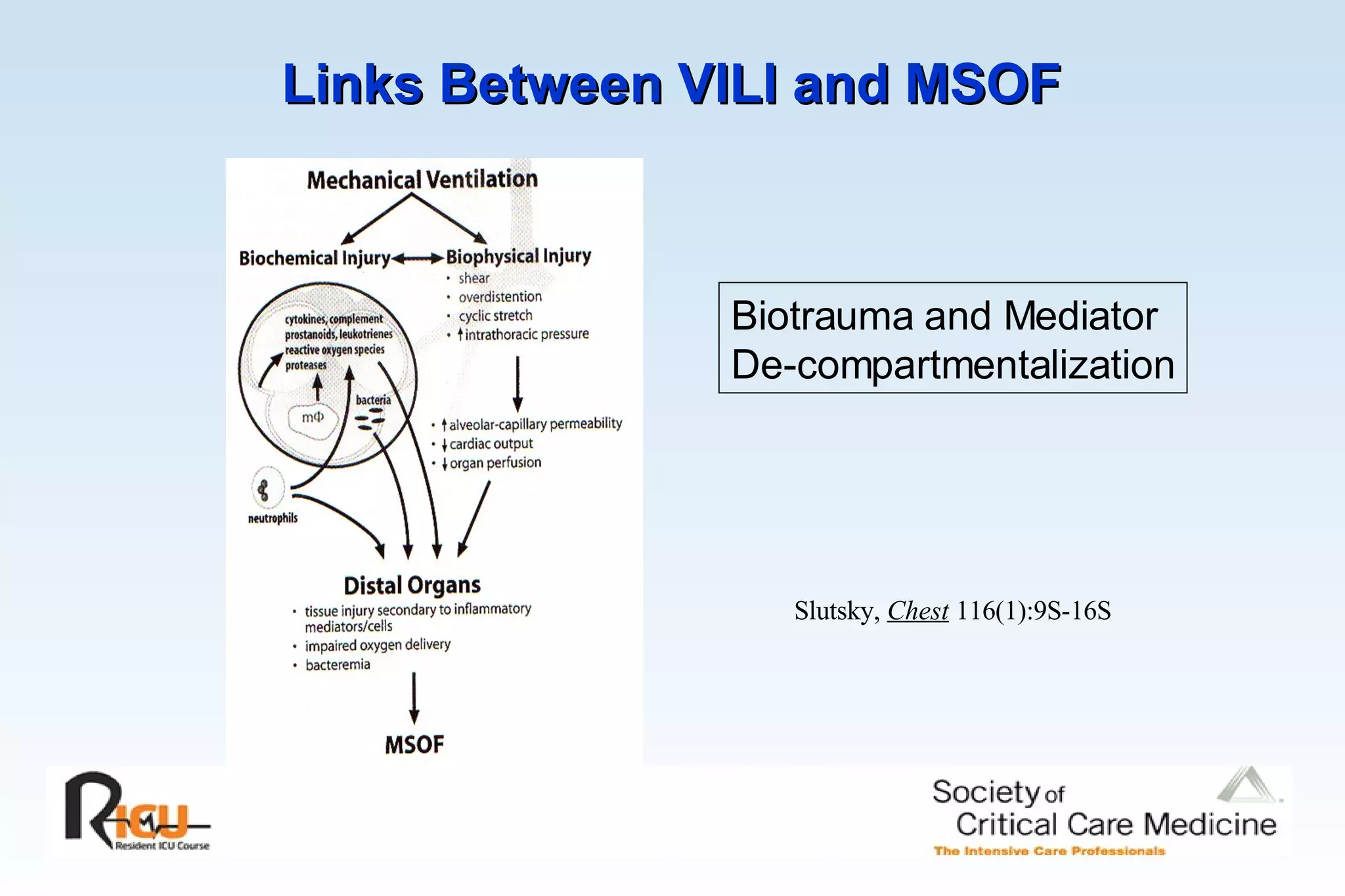
1) The consequences of elevated alveolar pressure such as barotrauma and ventilator-induced lung injury. Maintaining low tidal volumes and plateau pressures is important for lung protection.
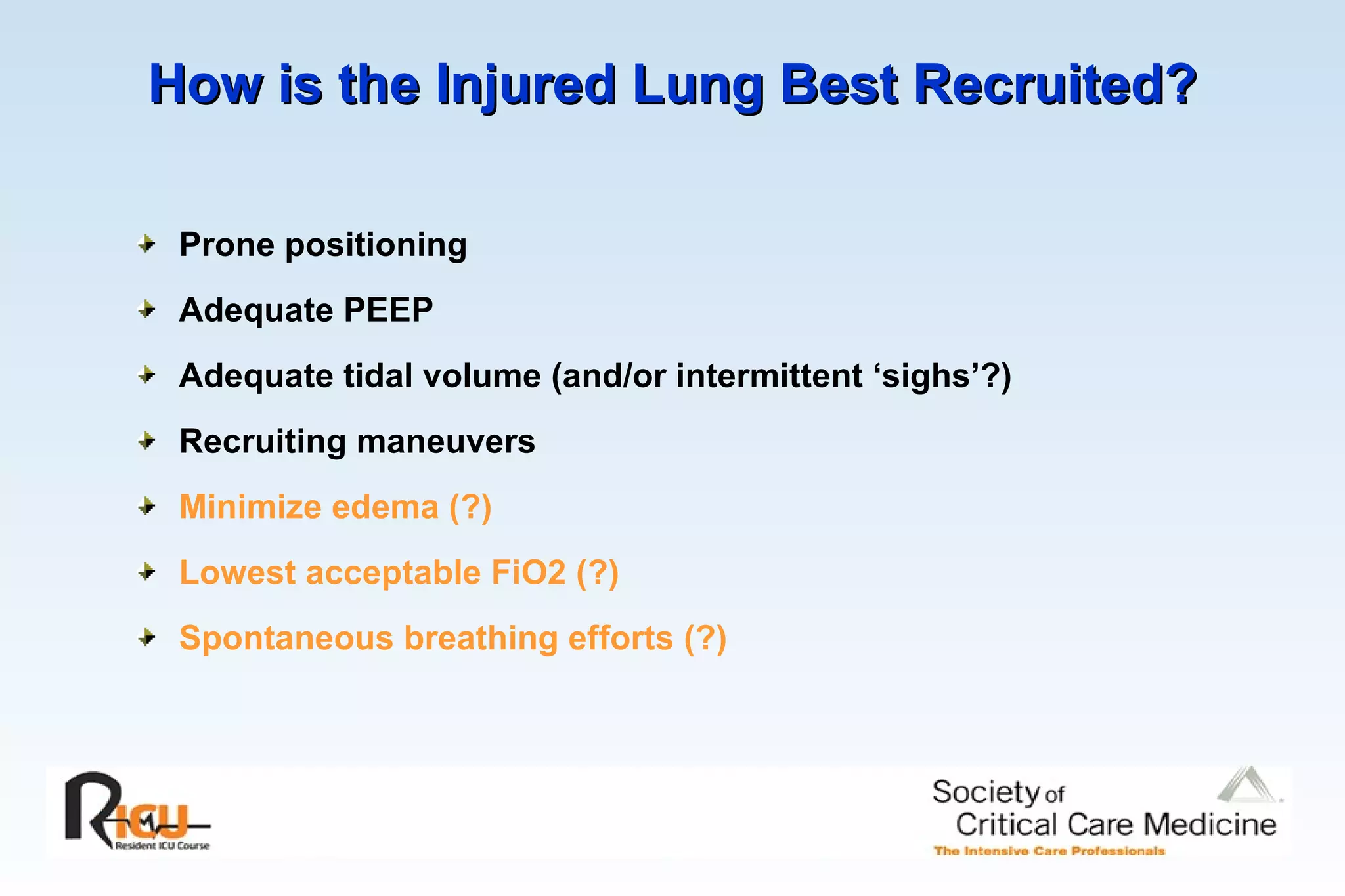
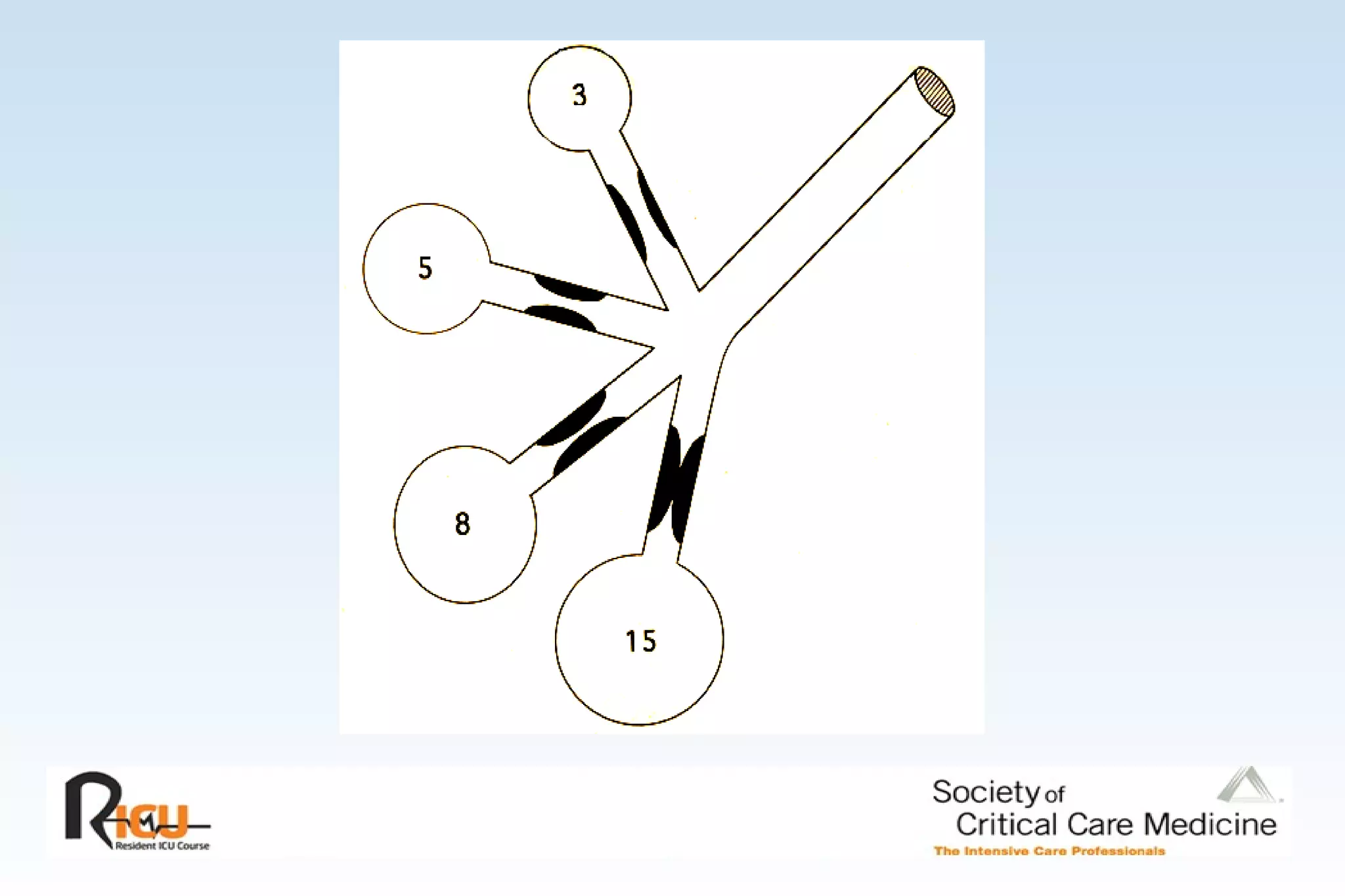
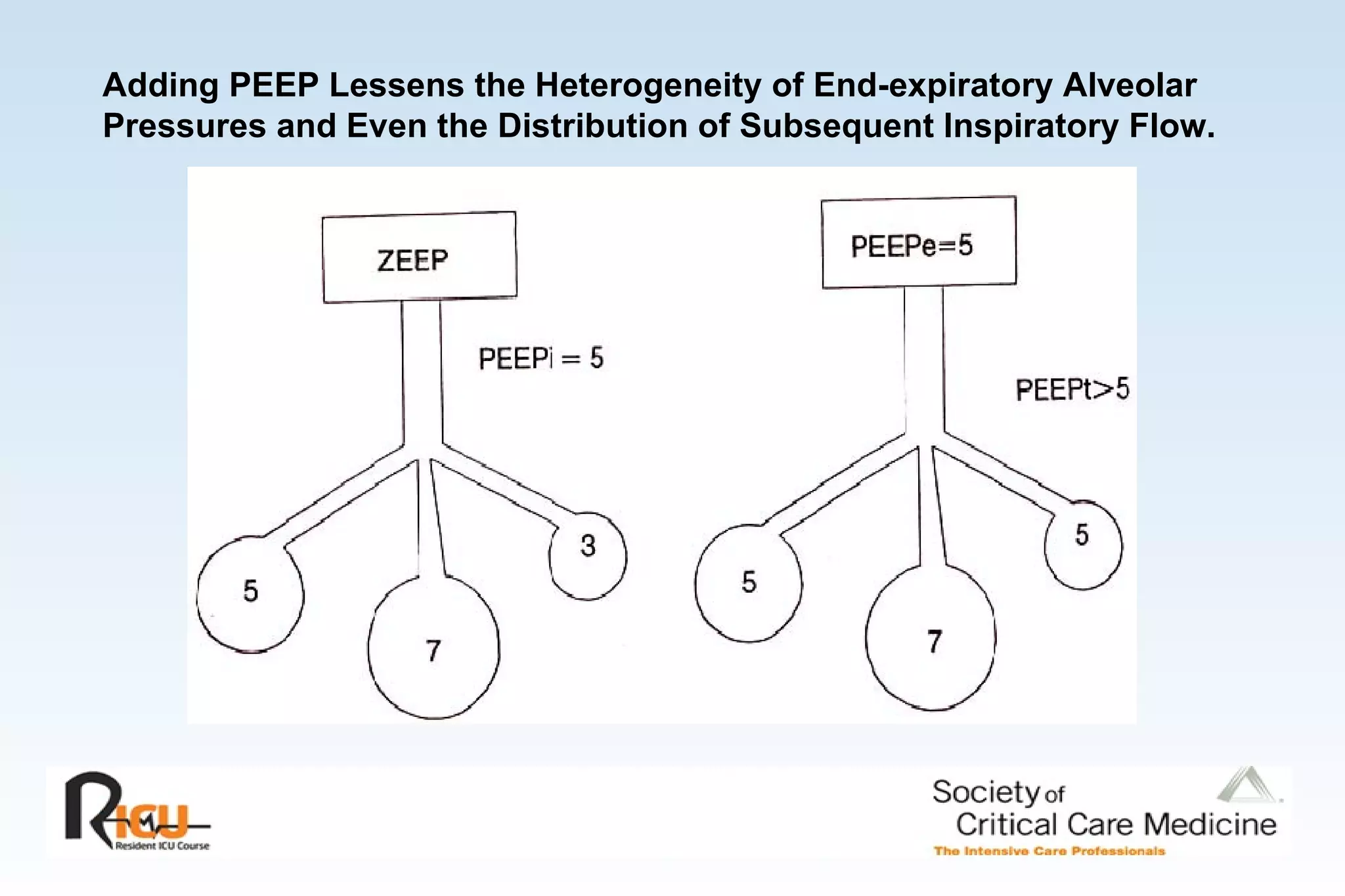
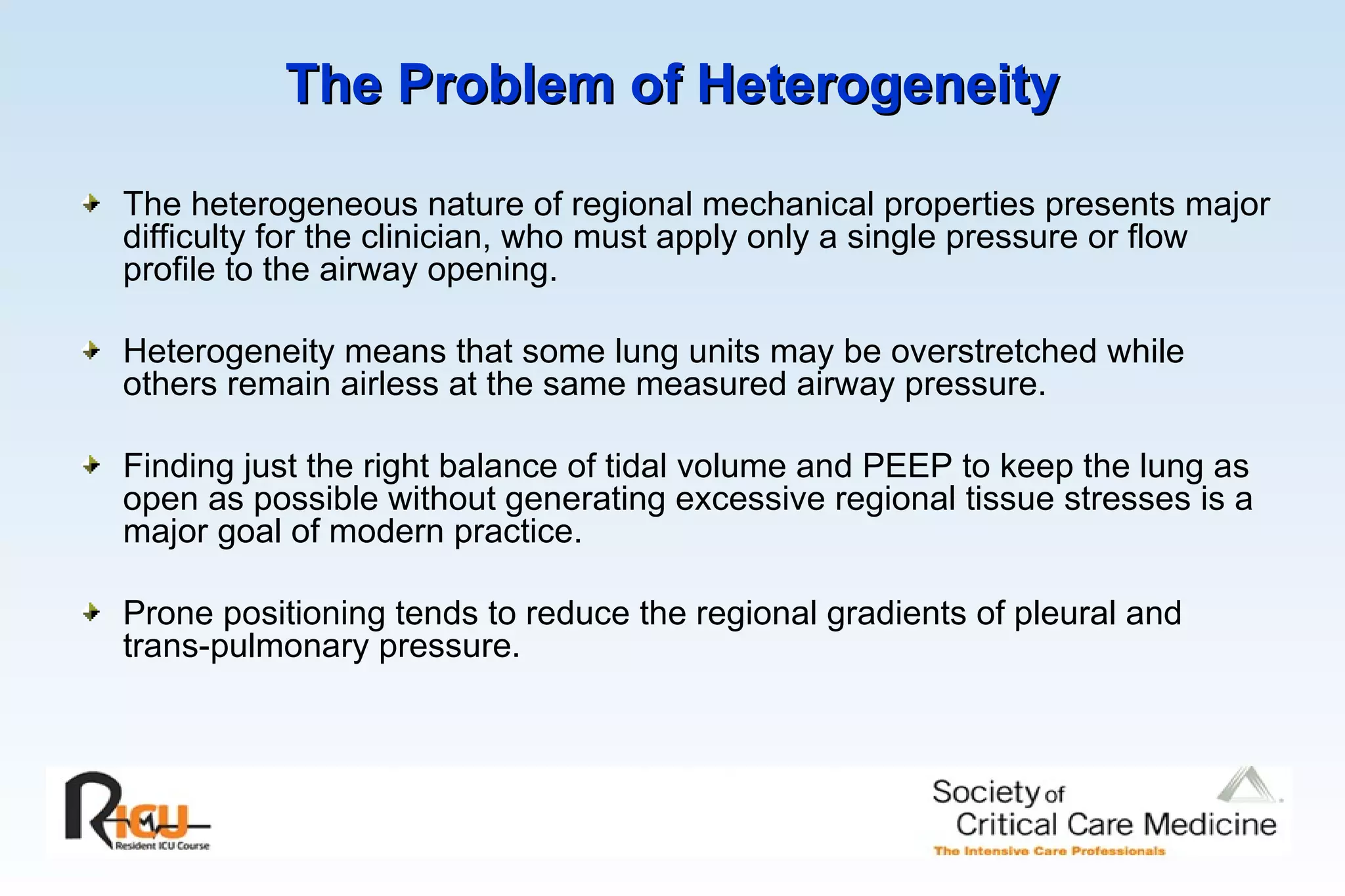
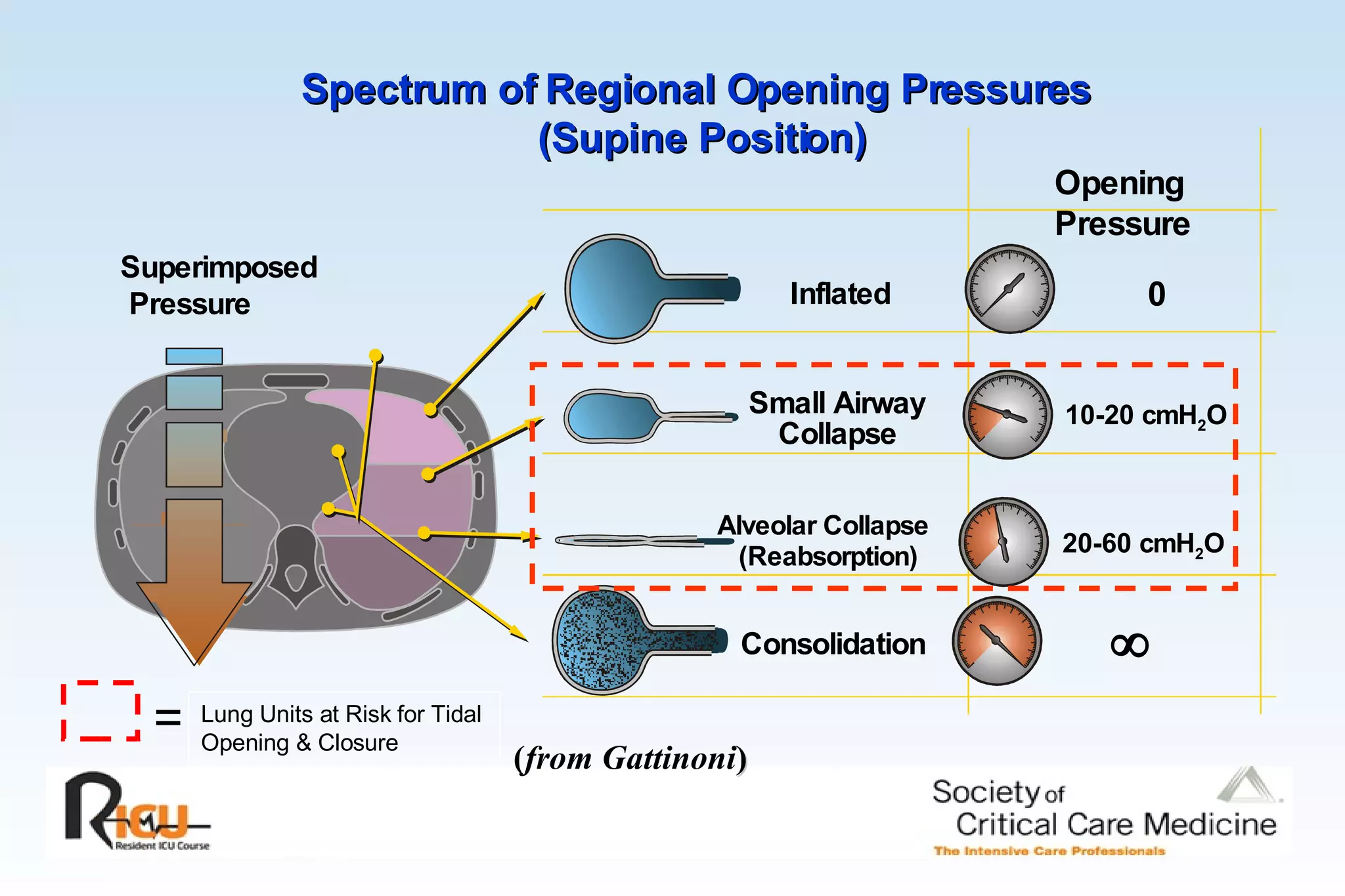
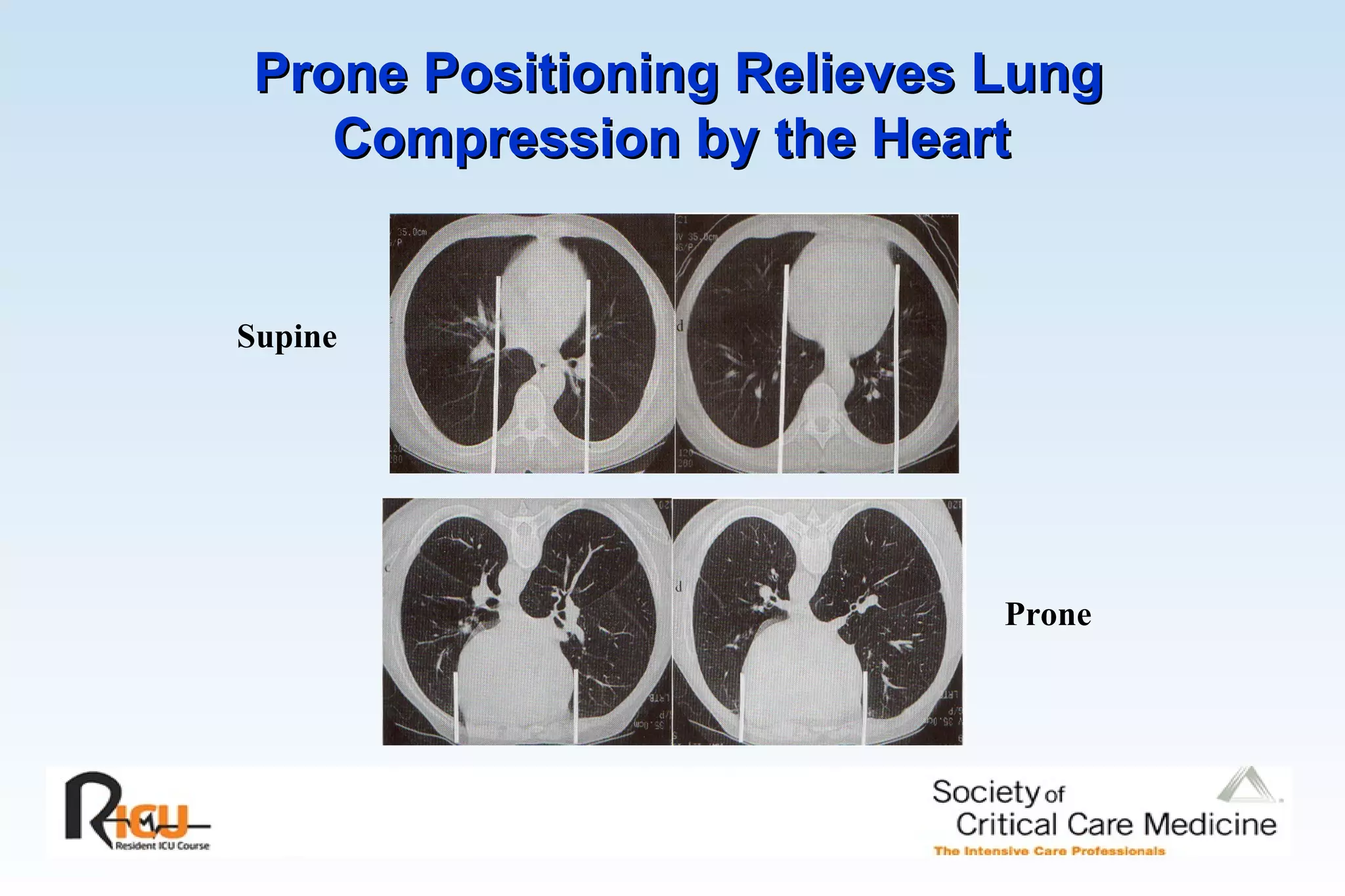
2) Heterogeneous lung inflation can lead to over- or under-inflation in different regions, even when total lung measures appear normal. Recruitment maneuvers and prone positioning can help address this.
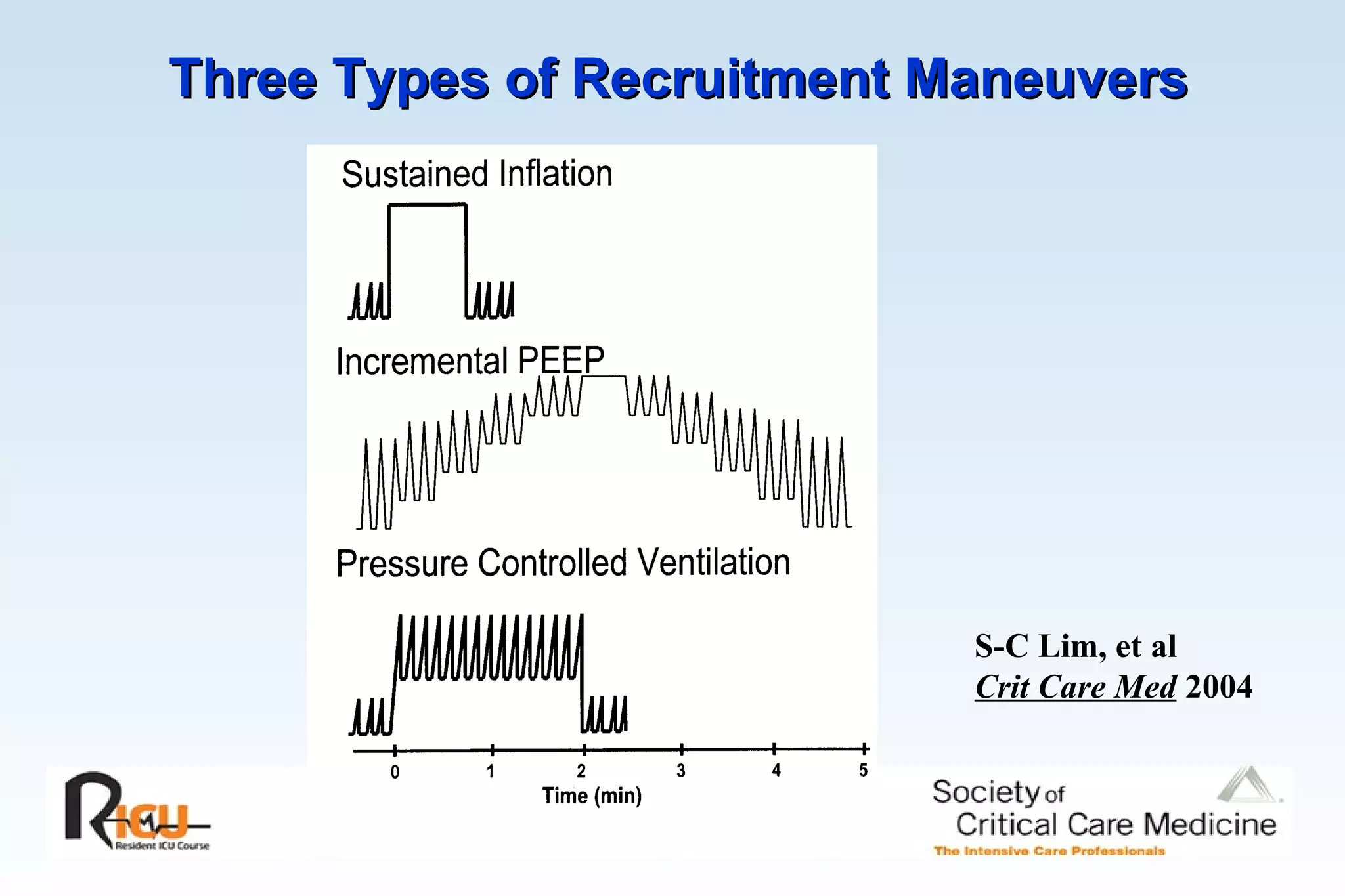
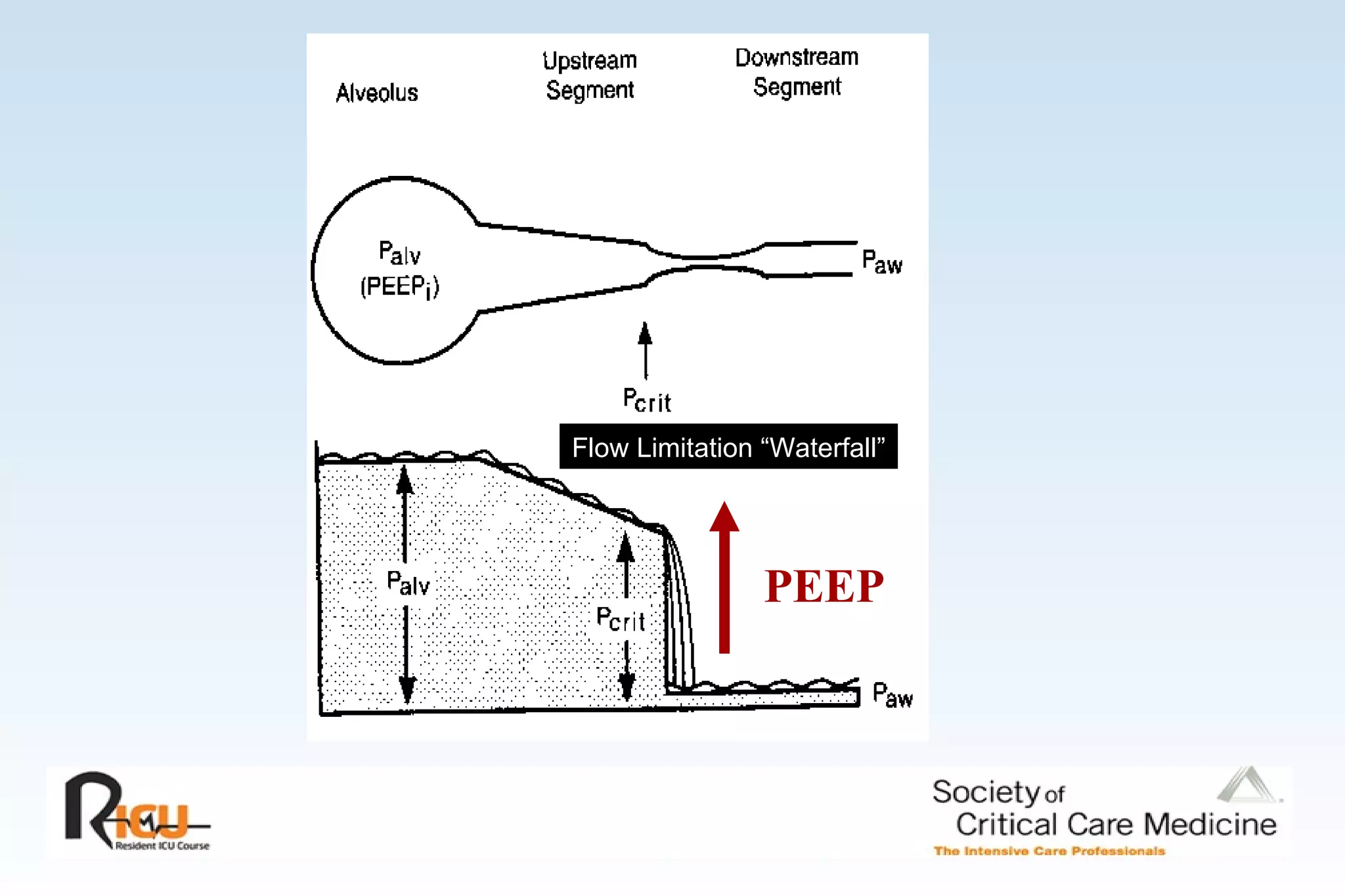
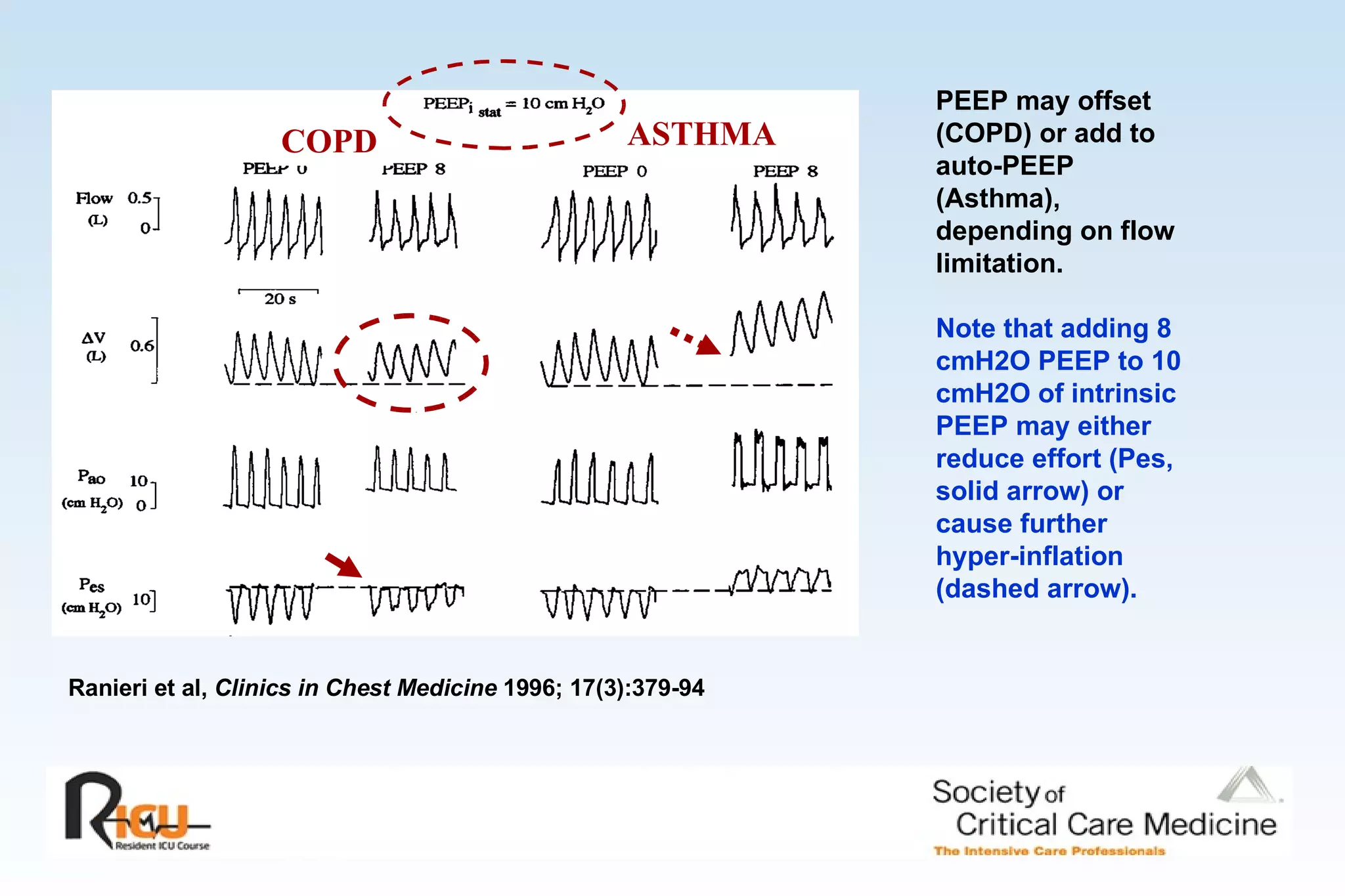
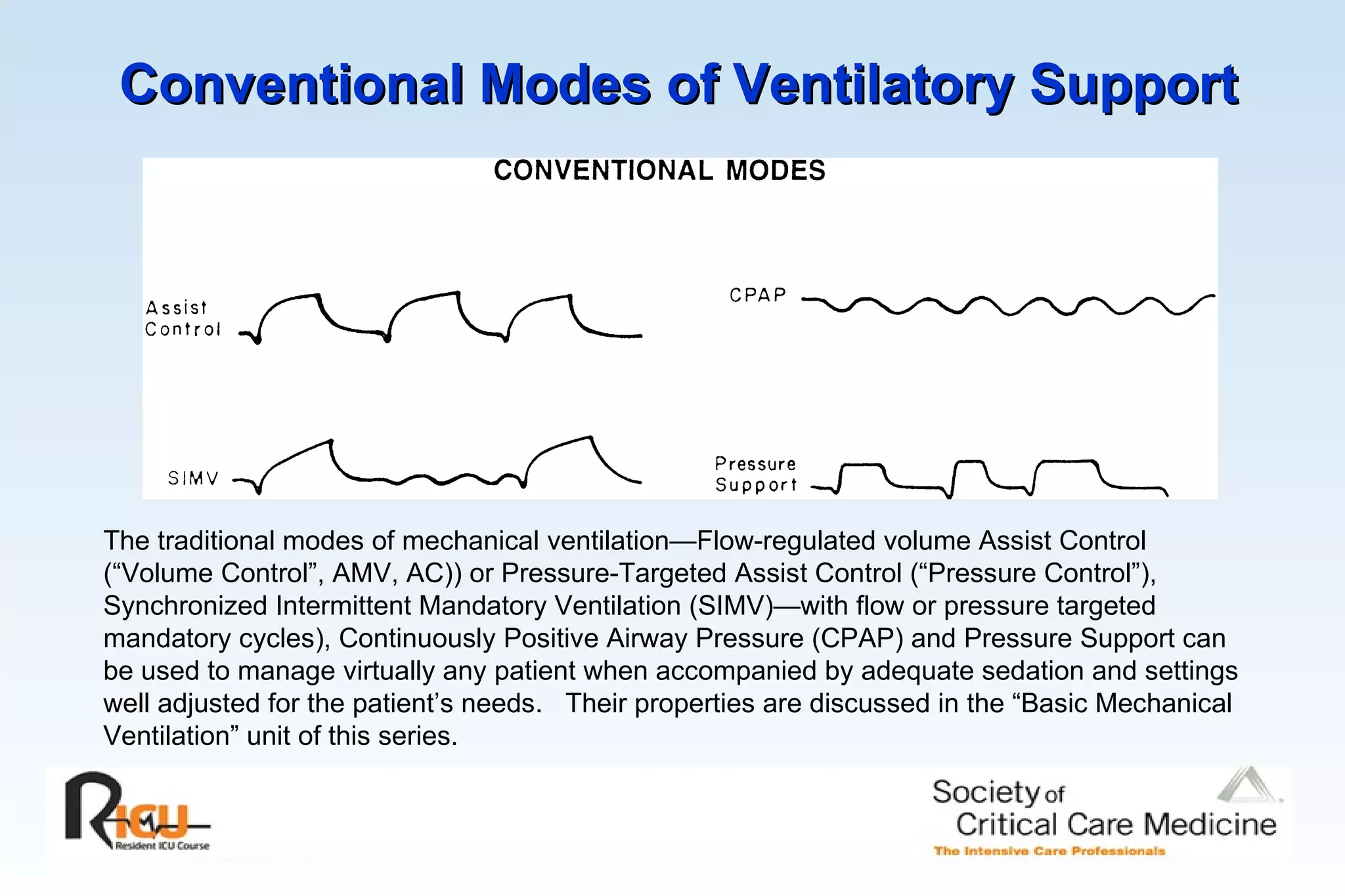
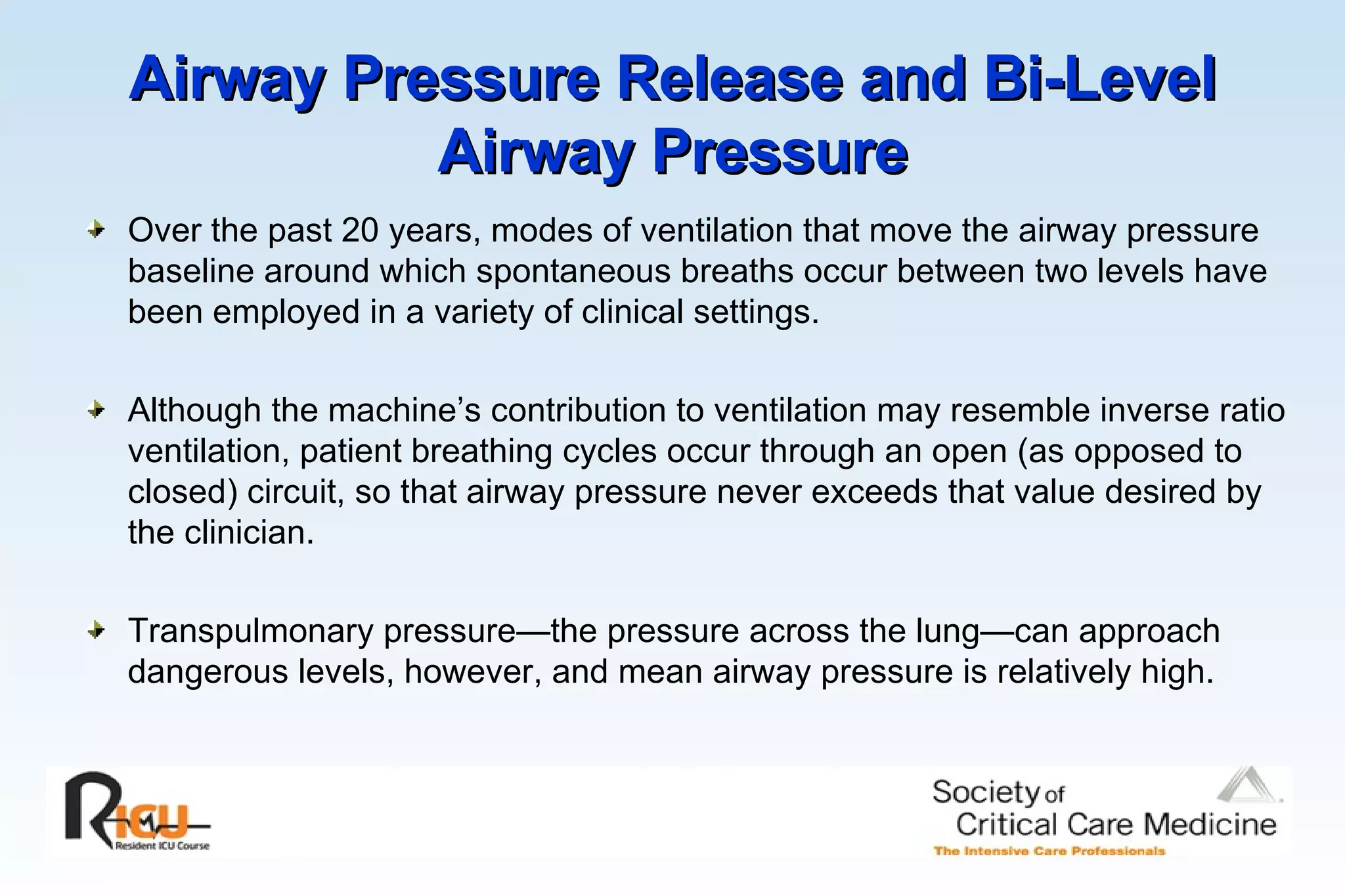
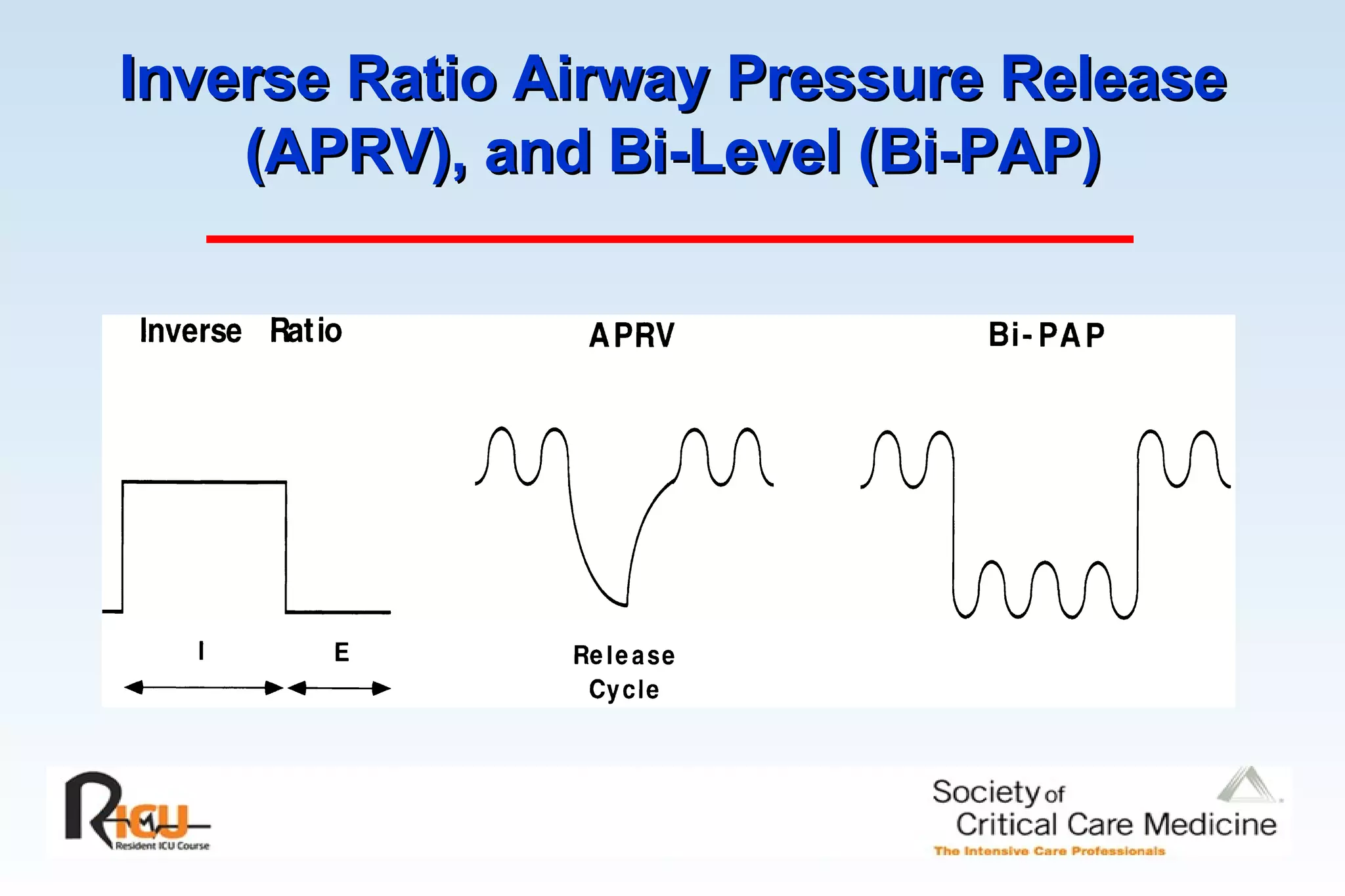
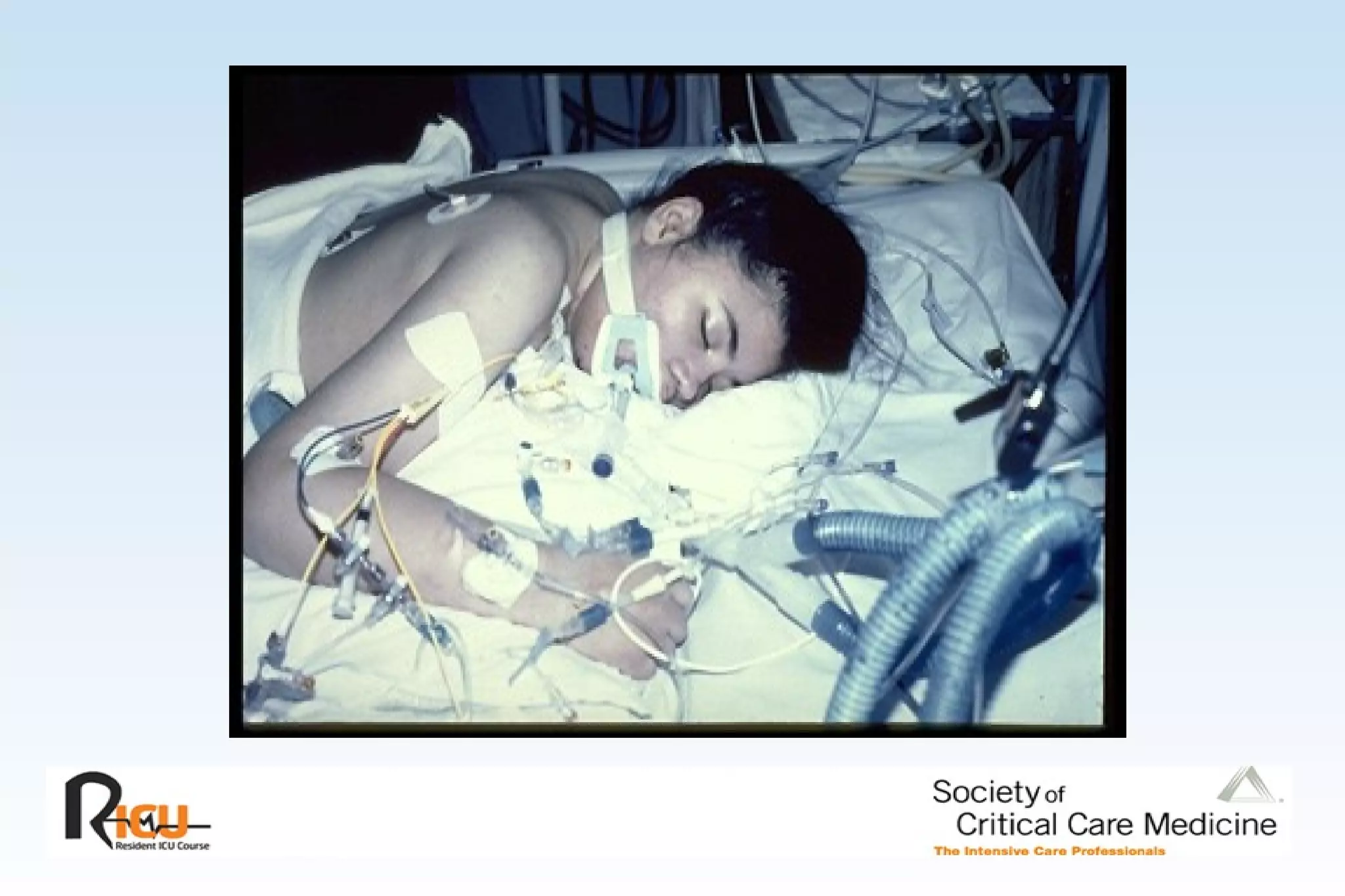
3) Adjuncts like recruitment maneuvers, prone positioning, and adjusting PEEP and modes of ventilation can help address challenges like acute lung injury, airflow obstruction, and withdrawing support.
















![% Opening and Closing Pressures in ARDS 50 High pressures may be needed to open some lung units, but once open, many units stay open at lower pressure. Paw [cmH 2 O] 0 5 10 15 20 25 30 35 40 45 50 0 10 20 30 40 Opening pressure Closing pressure From Crotti et al AJRCCM 2001.](https://image.slidesharecdn.com/advanced-mechanical-ventilation-1203110587561982-4/75/Advanced-Mechanical-Ventilation-22-2048.jpg)






![How Much Collapse Is Dangerous Depends on the Plateau R = 100% 20 60 100 Pressure [cmH 2 O] 20 40 60 Total Lung Capacity [%] R = 22% R = 81% R = 93% 0 0 R = 0% R = 59% From Pelosi et al AJRCCM 2001 Some potentially recruitable units open only at high pressure More Extensive Collapse But Lower P PLAT Less Extensive Collapse But Greater P PLAT](https://image.slidesharecdn.com/advanced-mechanical-ventilation-1203110587561982-4/75/Advanced-Mechanical-Ventilation-33-2048.jpg)