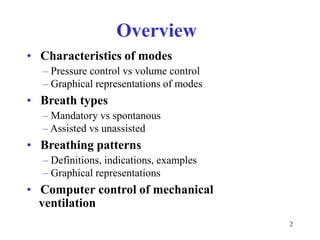
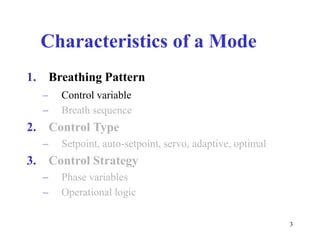
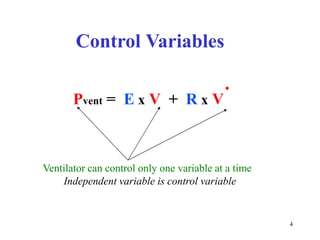
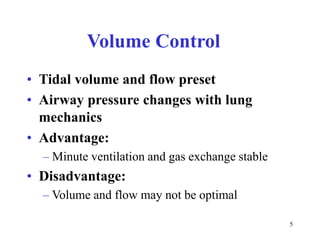
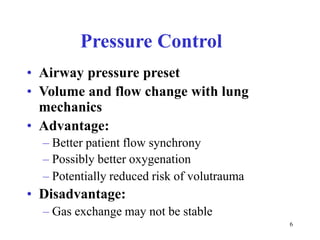
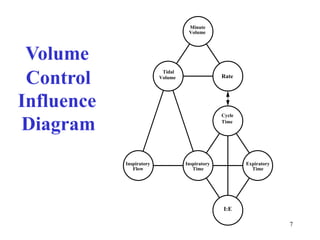
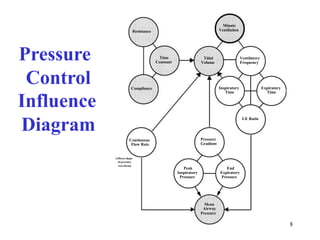
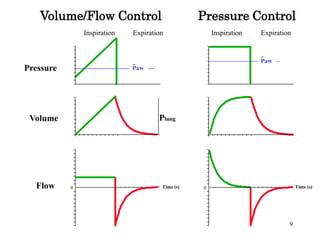
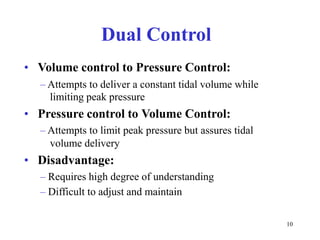
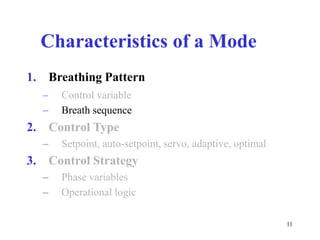
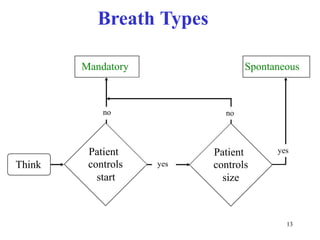
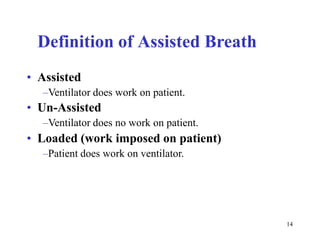
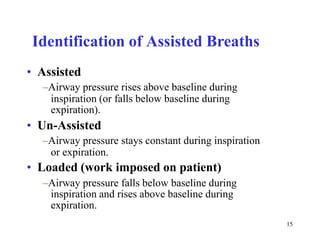
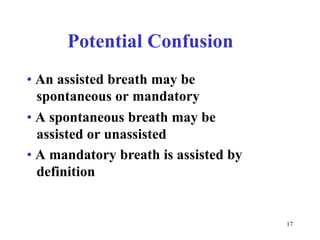
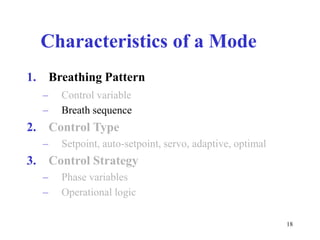
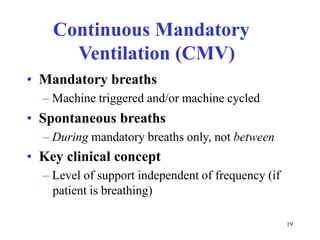
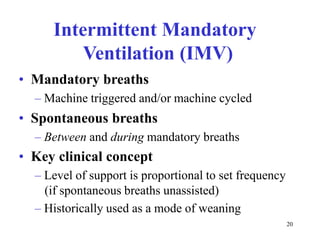
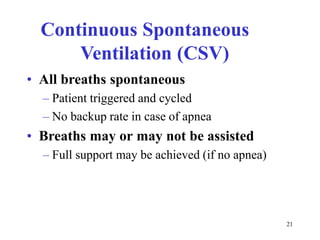
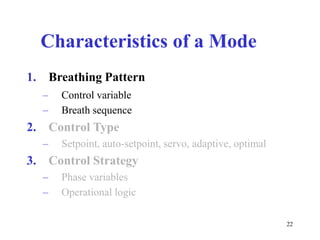
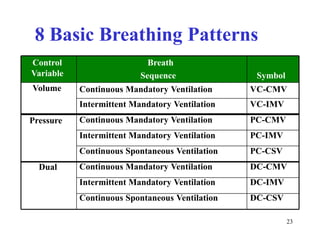
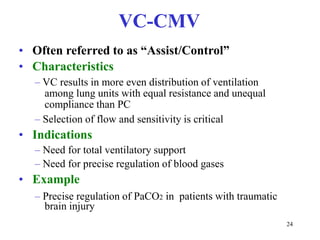
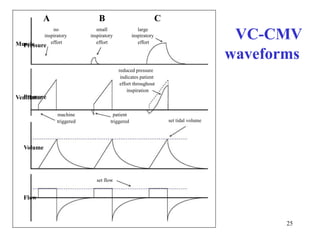
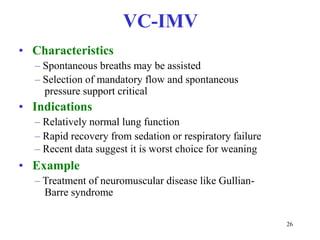
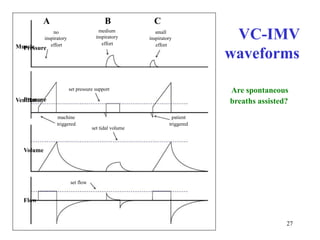
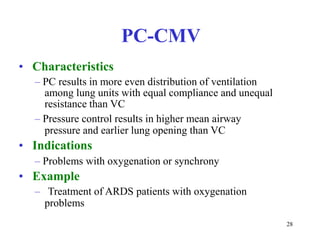
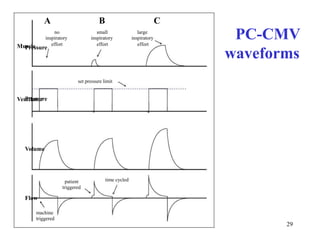
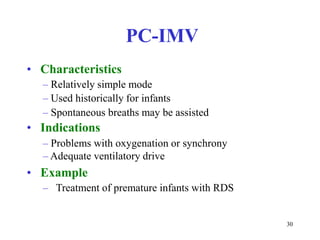
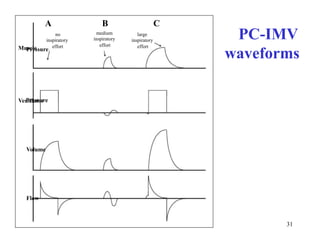
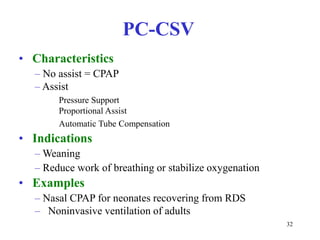
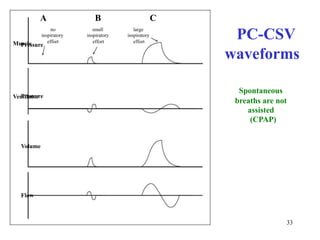
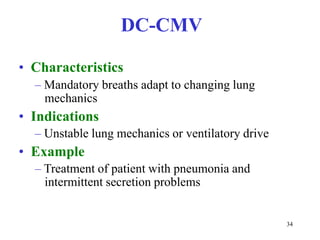
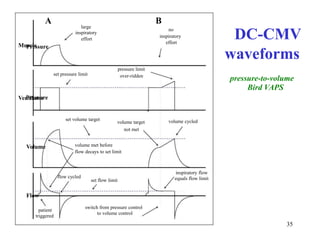
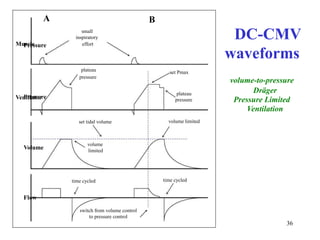
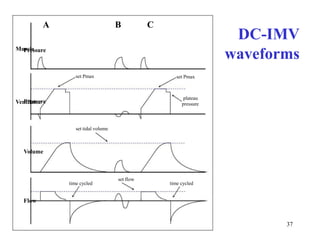
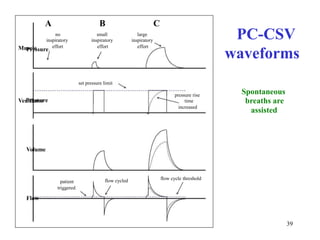
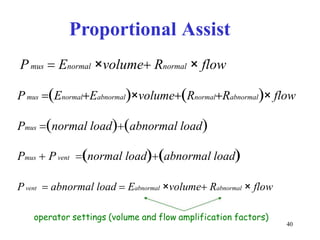
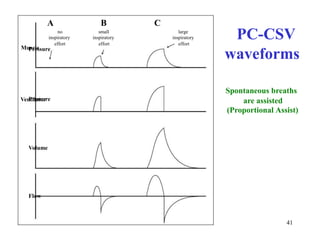
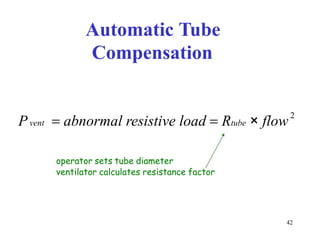
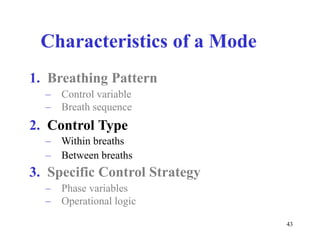
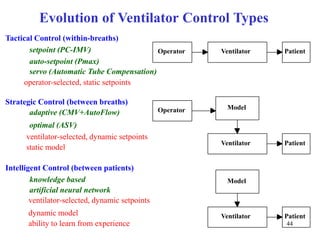
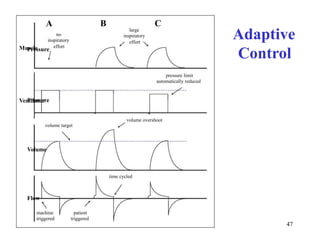
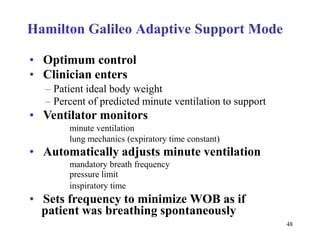
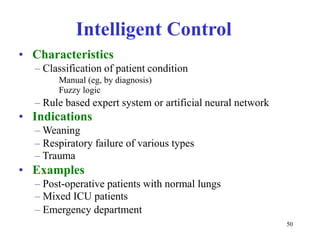
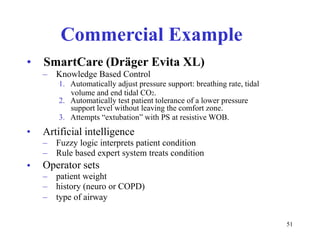
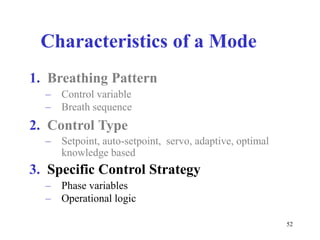
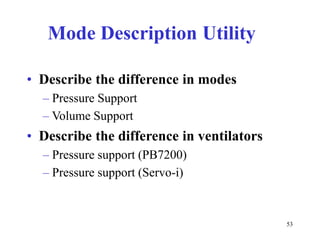
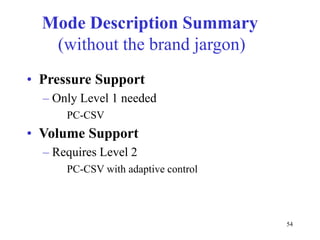
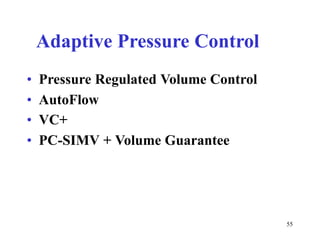
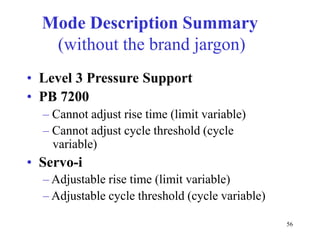
The document discusses various modes of mechanical ventilation. It defines key characteristics of ventilation modes including the control variable, breath sequence, control type, and specific control strategies. Pressure control and volume control modes are described and compared. Graphical representations of common breathing patterns like pressure control-continuous mandatory ventilation are provided. Advanced modes involving automatic adjustments are also outlined, such as adaptive control and intelligent modes using artificial intelligence.