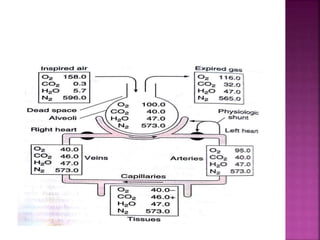
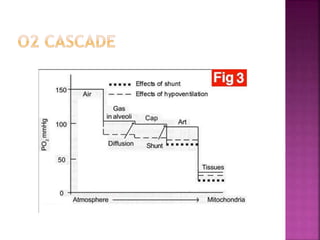
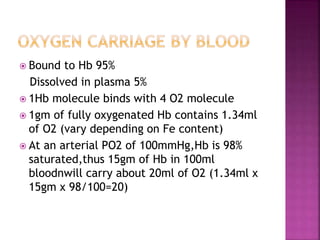
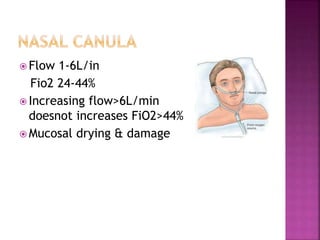
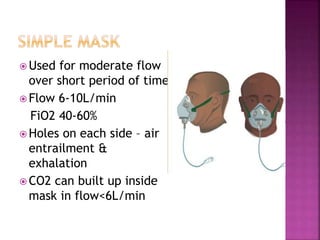
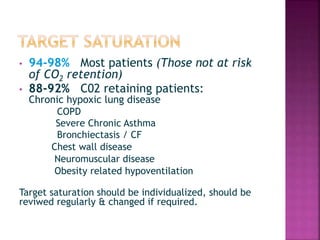
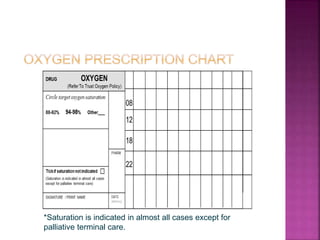
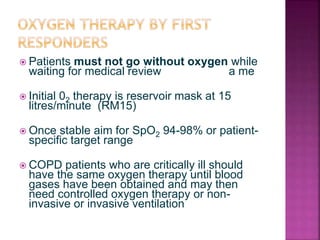
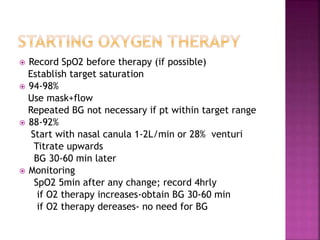
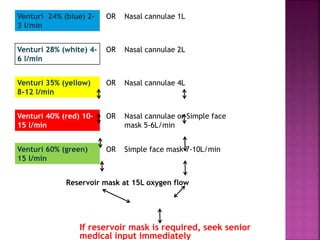
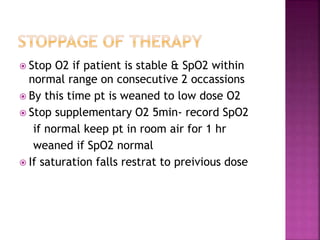
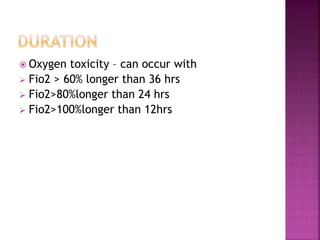
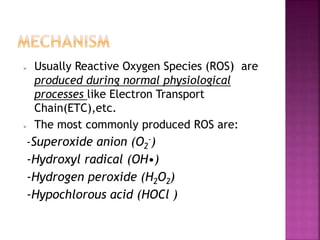
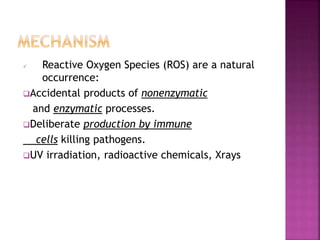
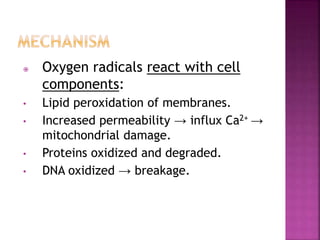
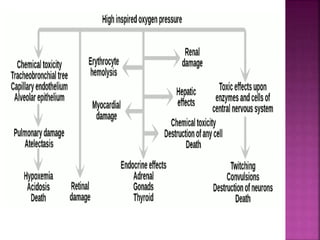
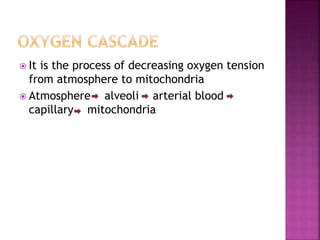
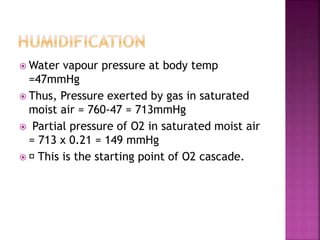
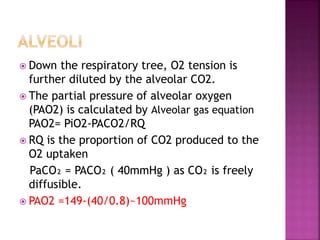
The document discusses the mechanics of gas exchange and oxygen transportation in the human body, emphasizing the significance of partial pressures, the oxygen cascade, and hemoglobin's oxygen-binding properties. It also covers the clinical aspects of oxygen therapy, including indications, delivery systems, and the importance of individual target saturation levels for different patient populations. It concludes with a warning about the potential toxic effects of prolonged high concentrations of oxygen.
![ Hb mediated + dissolved state
O2 carrying capacity of blood= [(1.34 x
HbxSaO2)+(0.003xPaO2)] x Q
O2 delivery to tissues depends on
1. Hb concentration
2. O2 binding capacity of Hb
3. saturation of Hb
4. amount of dissolved O2
5. cardiac output (Q)](https://image.slidesharecdn.com/oxygencascadetherapy-190801140904/85/Oxygen-cascade-therapy-8-320.jpg)