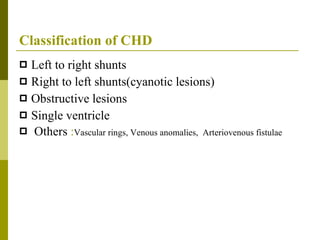
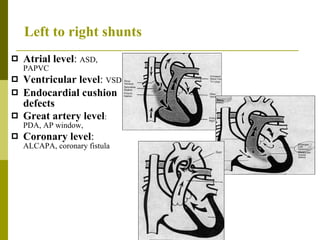
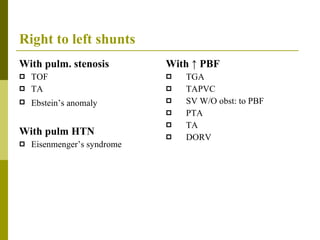
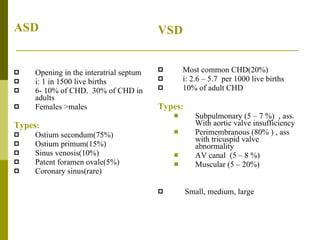
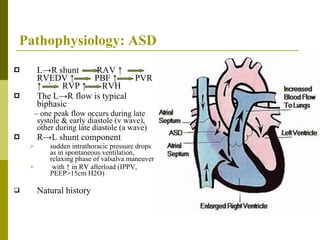
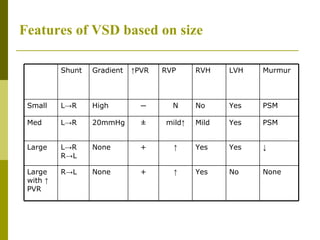
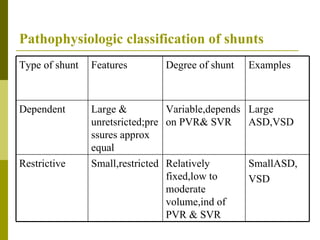
This document provides an overview of the classification, pathophysiology, preoperative evaluation, and anesthetic management considerations for patients undergoing surgery with congenital heart defects such as atrial septal defects (ASD) and ventricular septal defects (VSD). It discusses the pathophysiology of left-to-right and right-to-left shunting, preoperative assessment including history, examination, investigations, and risk factors. It also outlines goals and techniques for anesthesia including bubble avoidance, optimizing oxygen delivery and ventilation, and avoiding hypovolemia and increases in left-to-right shunting. Specific considerations for inhalational and intravenous induction agents, central neuraxial blockade, pregnancy, and Eisenmenger