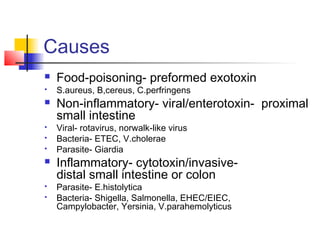
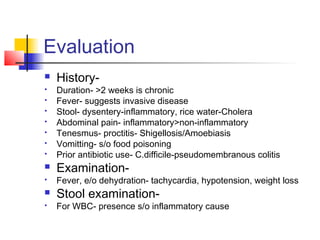
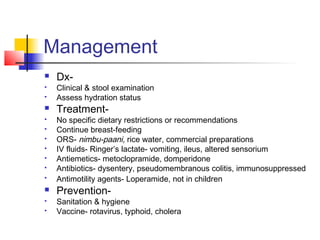
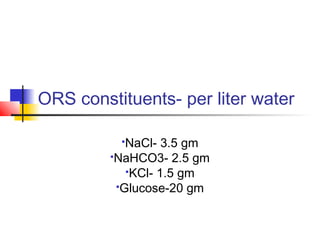
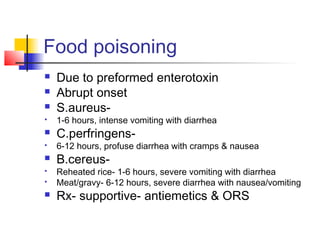
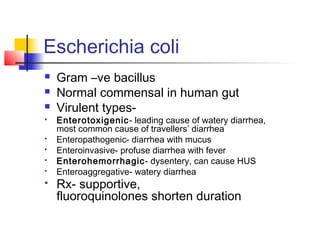
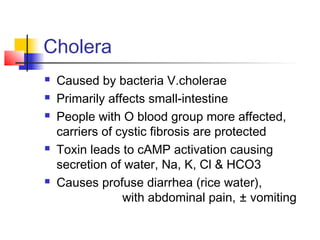
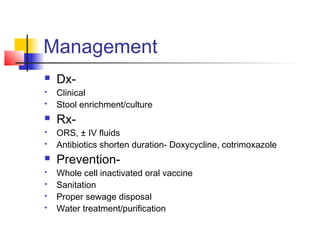
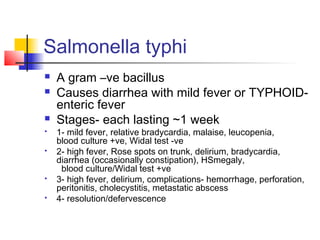
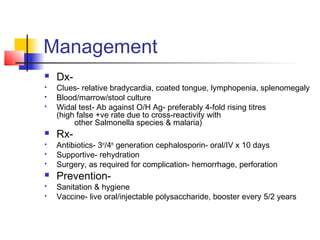
This document discusses various causes of acute infectious diarrhea including food poisoning caused by Staphylococcus aureus and Bacillus cereus producing preformed exotoxins as well as viral and bacterial pathogens like rotavirus, ETEC, and Vibrio cholerae producing enterotoxins. Evaluation involves assessing duration of symptoms, stool characteristics, and signs of dehydration or inflammation. Management consists of oral rehydration with solutions like ORS, antiemetics, antibiotics for invasive causes, and prevention through hygiene and vaccination. Specific conditions discussed in more detail include cholera, E. coli pathotypes, Salmonella Typhi causing typhoid fever, and constituents of ORS.