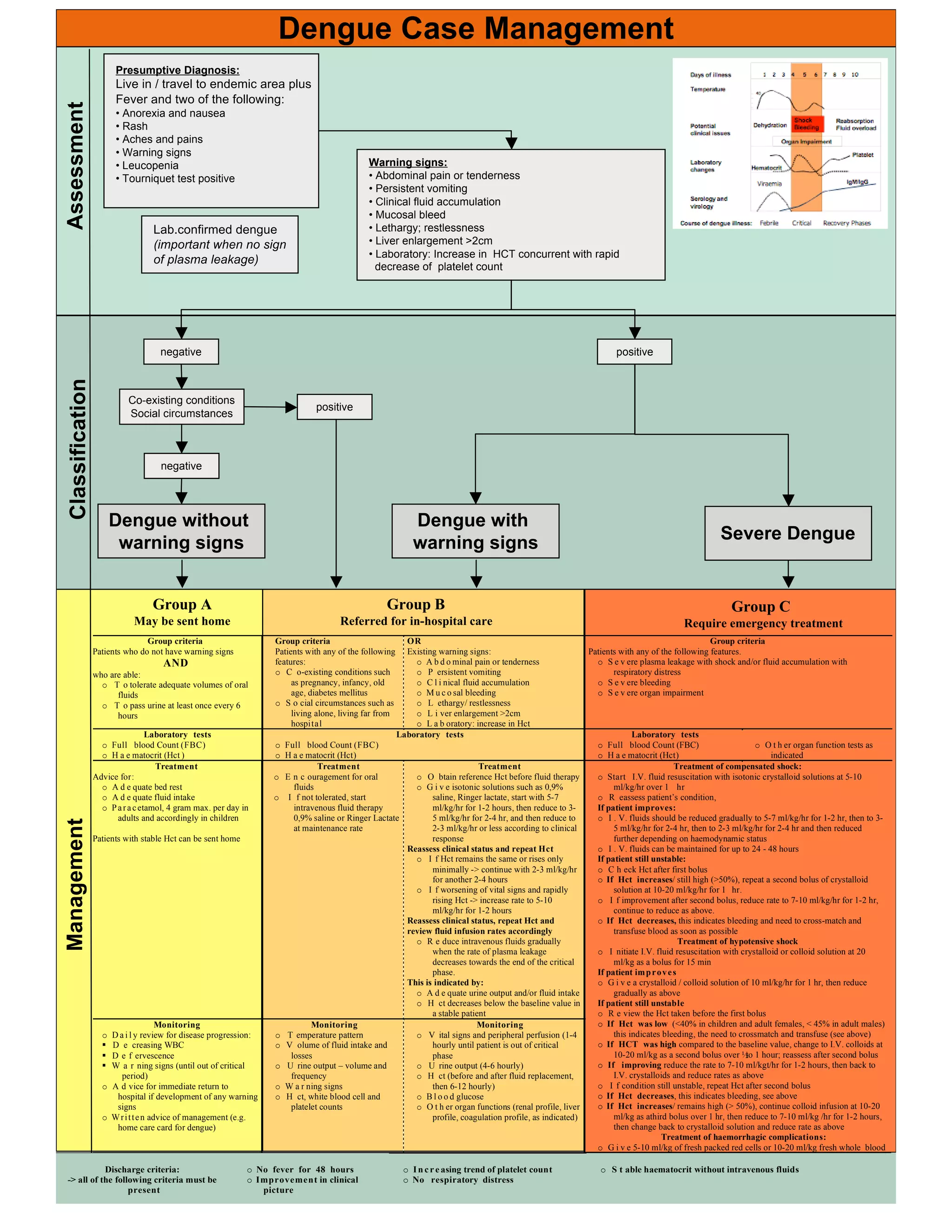
This document provides guidance on diagnosing and managing dengue fever and its potential complications. It outlines the criteria for presumptive diagnosis of dengue and distinguishing warning signs. It then categorizes dengue cases into three groups - dengue without warning signs, dengue with warning signs, and severe dengue - with different treatment protocols depending on the severity of symptoms and laboratory findings. The treatment sections provide detailed guidance on fluid management, monitoring, and treatment of complications like shock for each dengue case category.