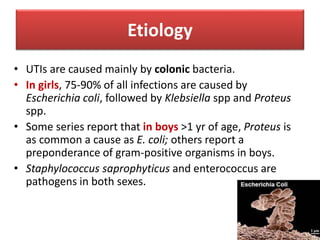
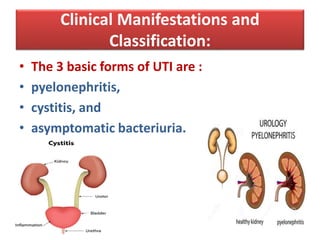
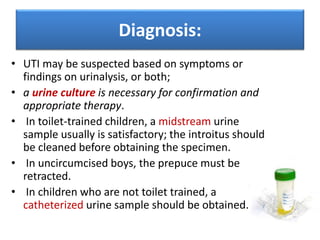
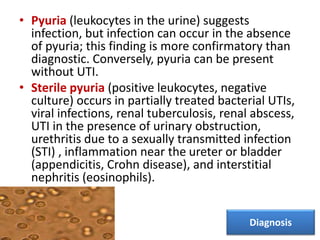
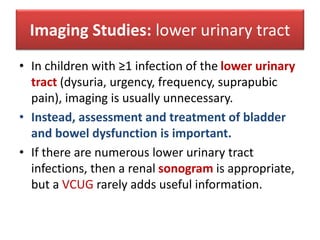
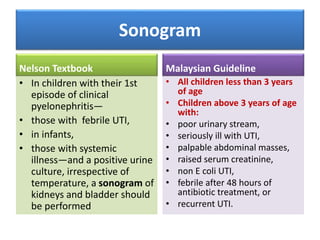
Urinary tract infections are common in children, especially girls. The most common cause is Escherichia coli bacteria spreading from the intestines. Symptoms vary from mild cystitis to severe pyelonephritis. Diagnosis involves urinalysis and urine culture. Treatment depends on severity but commonly involves antibiotics like trimethoprim-sulfamethoxazole. Imaging with ultrasound is recommended for the first UTI in infants and children under 3, or those with fever or systemic illness, to check for anatomical abnormalities.