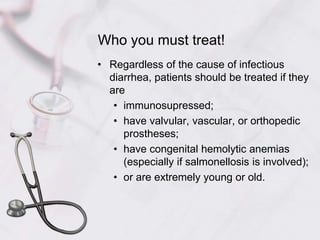
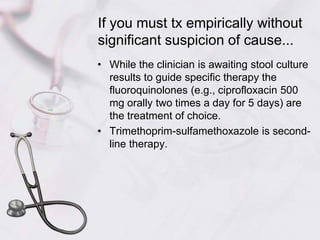
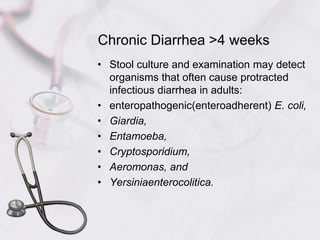
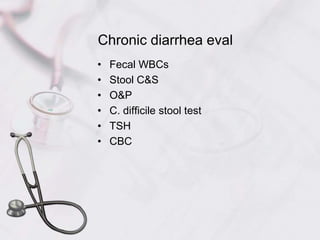
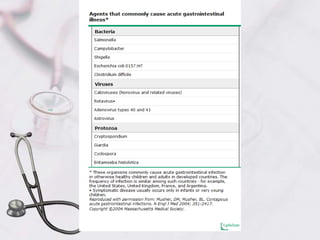
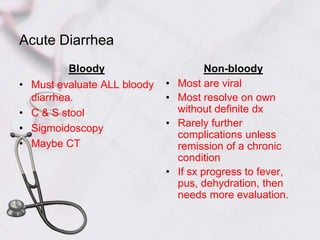
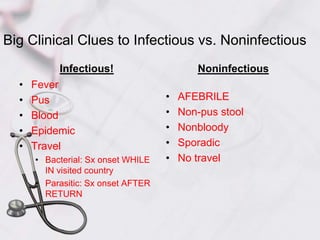
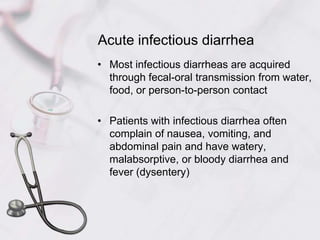
This document defines acute and chronic diarrhea and outlines their etiologies and treatment approaches. Acute diarrhea is typically infectious in nature and lasts less than 3 weeks, with the most common causes being viruses, bacteria, parasites, and protozoa. Chronic diarrhea lasts over 4 weeks and can be due to malabsorption, secretory causes, or inflammation. The document provides detailed information on evaluating, diagnosing, and managing different causes of acute and chronic diarrhea.

![Anxiolytics (e.g., diazepam 2 mg orally two to four times daily) and antiemetics (e.g., promethazine 12.5 to 25 mg orally once or twice daily) that decrease sensory perception may make symptoms more tolerable and are safe.Some foods or food-derived substances (green bananas, pectins [amylase-resistant starch], zinc) lessen the amount and/or duration of diarrhea. Zinc supplementation (20 mg of elemental zinc orally once a day) is effective in preventing recurrences of diarrhea in malnourished children.](https://image.slidesharecdn.com/acuteandchronicdiarrheapspa2011-111002100853-phpapp02/85/Acute-and-chronic-diarrhea-summary-43-320.jpg)
![Probiotics are live, nonpathogenic, human microorganisms that provide a health benefit. Level 1 evidence has been reported for the therapeutic use of probiotics.Most species are lactic acid bacteria. Lactobacillus GG (1010 colony-forming units [CFU]/250 mL ORS daily until diarrhea stops) added to an ORS decreases the duration of diarrhea in children with acute diarrhea, particularly with rotavirus infection.](https://image.slidesharecdn.com/acuteandchronicdiarrheapspa2011-111002100853-phpapp02/85/Acute-and-chronic-diarrhea-summary-44-320.jpg)