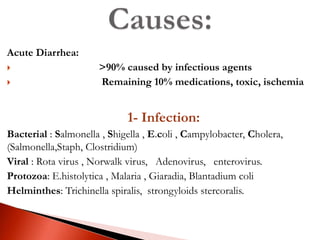
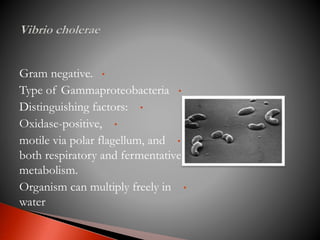
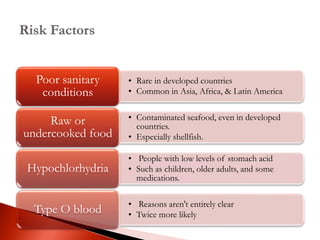
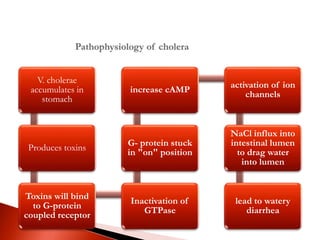
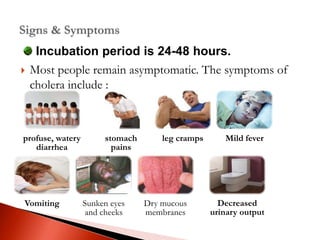
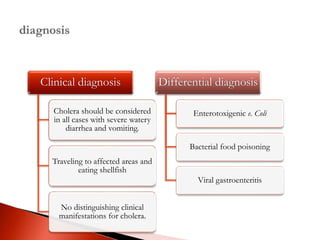
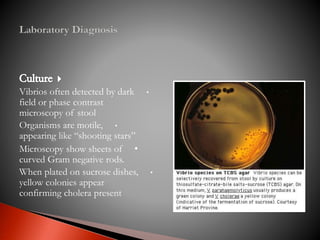
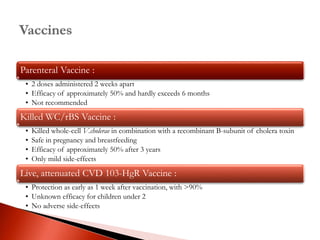
This document defines diarrhea and classifies it as acute, persistent, or chronic based on duration. It then discusses the various causes of acute diarrhea including infectious agents like bacteria, viruses, protozoa, and helminths. Other potential causes mentioned are medications, toxins, diet, ischemia, and psychological stress. The document goes on to discuss specific infectious causes like cholera in more detail, describing the organism, transmission, pathogenesis, signs and symptoms, diagnosis, and treatment options. Prevention strategies discussed include education, sanitation improvements, and vaccination.