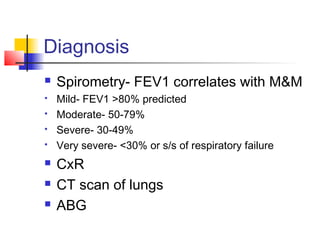
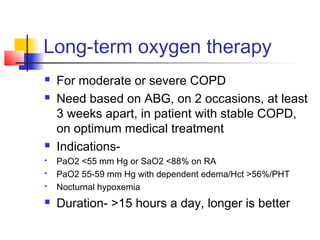
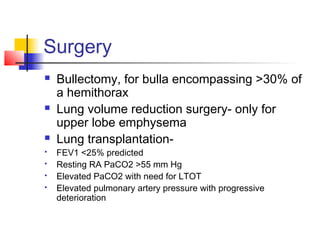
COPD is the 6th leading cause of death worldwide characterized by narrowing of airways. The two main types are chronic bronchitis, causing inflammation and fibrosis of airways, and emphysema, causing enlargement of airspaces. Smoking is the primary cause. Diagnosis involves spirometry showing reduced FEV1. Treatment focuses on smoking cessation, bronchodilators, steroids, oxygen therapy, and managing exacerbations.