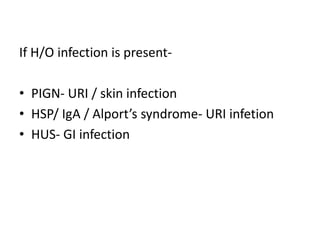
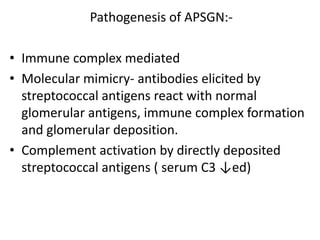
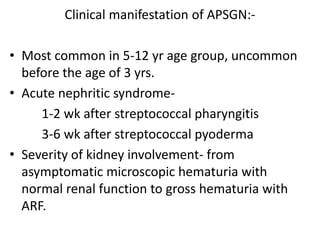
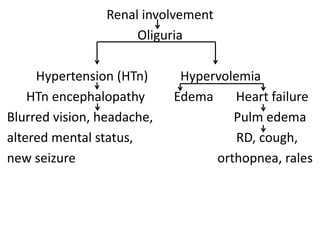
This document discusses the diagnosis and management of acute glomerulonephritis (AGN) in a 6-year-old girl presenting with red urine, edema, and headache following a sore throat. It details differential diagnoses such as post-infectious glomerulonephritis (PIGN) and IgA nephropathy, along with diagnostic investigations, clinical manifestations, and treatment approaches for various complications. The management includes addressing fluid overload, hypertension, anemia, and nutritional needs, with specific considerations for potential renal biopsy indications.