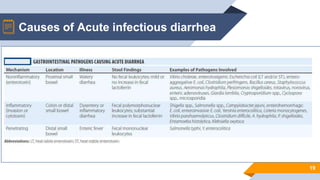
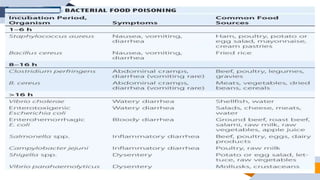
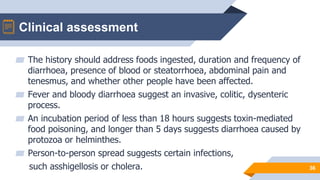
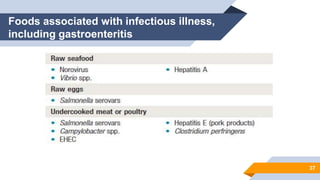
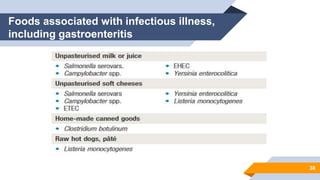
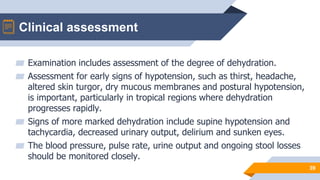
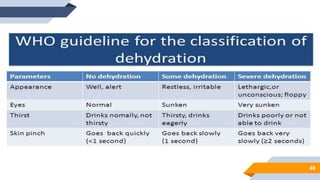
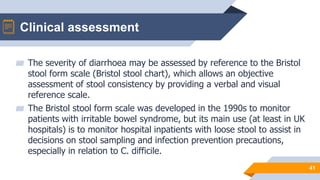
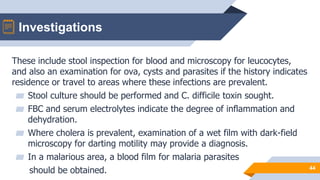
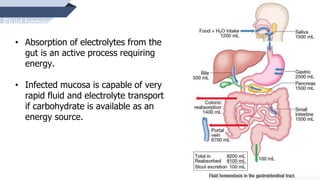
Acute infectious diarrhea is usually caused by faecal–oral transmission of bacteria or their toxins, viruses or parasites. It is typically short-lived and presents with acute diarrhea, sometimes with vomiting, as the predominant symptom. Clinical assessment involves evaluating the history of illness, examining the patient for dehydration, and investigating stool and blood samples. Management focuses on fluid replacement to treat dehydration as well as controlling symptoms, while antibiotics are usually not needed except for specific invasive bacterial infections.