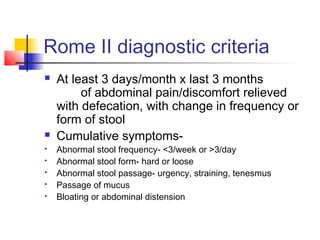
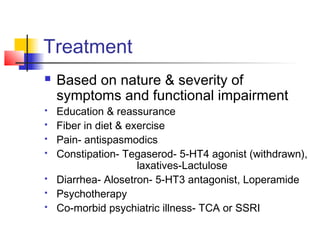
Irritable bowel syndrome (IBS) is a functional bowel disorder that is common, affecting around 20% of patients presenting to outpatient departments. IBS symptoms are not due to any underlying pathological cause, but rather are influenced by factors like altered gut motility or secretion in response to stimuli, hypersensitivity of the gut, and dysregulation of the brain-gut axis associated with greater stress reactivity. Diagnosis is based on Rome II criteria of abdominal pain relieved by defecation and changes in stool frequency or form occurring for at least 3 days per month over the past 3 months. Treatment focuses on education, diet, exercise, antispasmodics, laxatives, antidepressants, and psychotherapy depending on