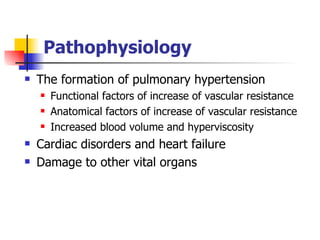
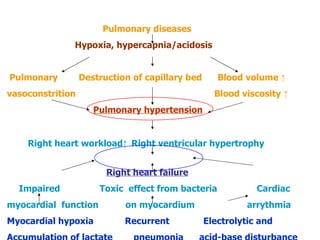
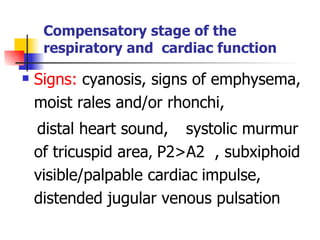
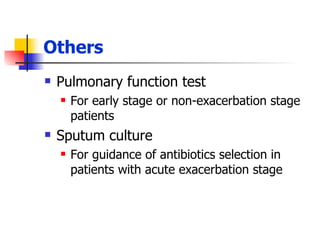
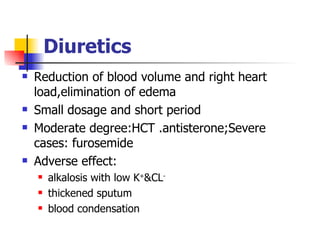
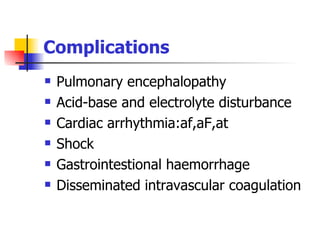
Cor Pulmonale, also known as pulmonary heart disease, is caused by high blood pressure in the lungs secondary to diseases affecting the lungs, chest wall, or pulmonary vasculature. It is characterized by hypertrophy and dilation of the right ventricle of the heart in response to the elevated pulmonary pressures. The main symptoms include cough, sputum production, shortness of breath, fatigue, and leg swelling. Diagnosis involves assessing the patient's medical history along with tests such as chest x-rays, electrocardiograms, echocardiograms, and blood gas analysis. Treatment focuses on controlling infections, improving oxygen levels, managing heart failure, and preventing complications through patient monitoring and education.