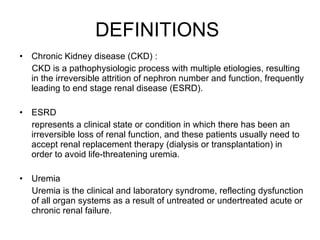
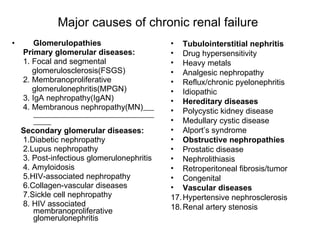
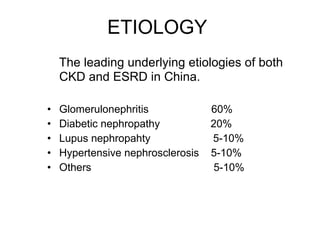
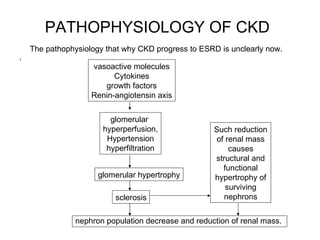
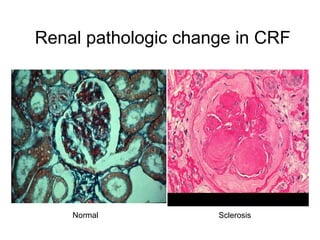
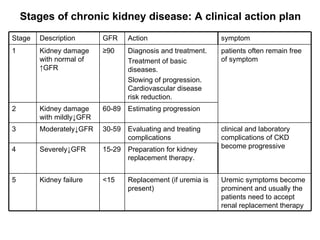
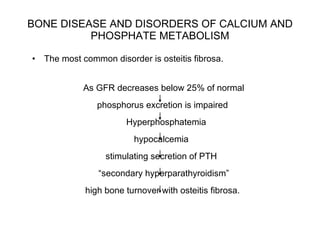
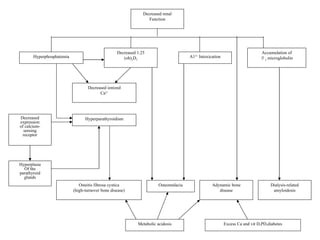
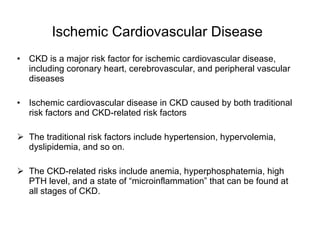
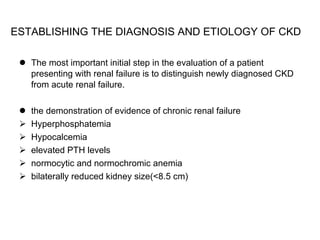
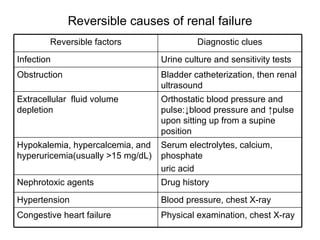
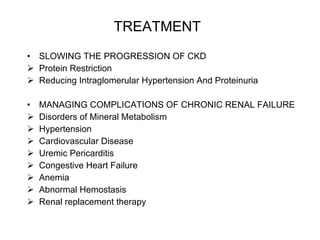
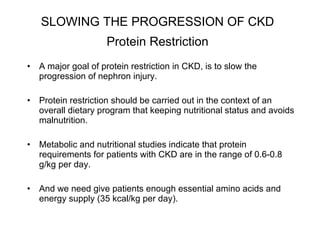
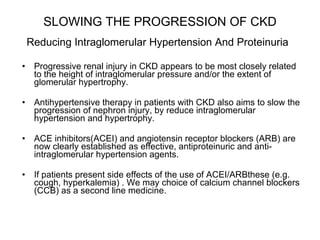
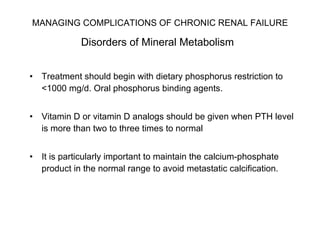
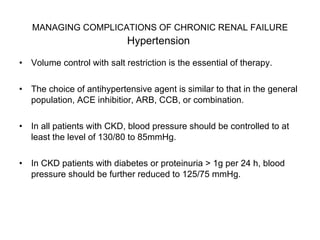
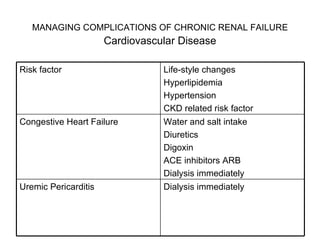
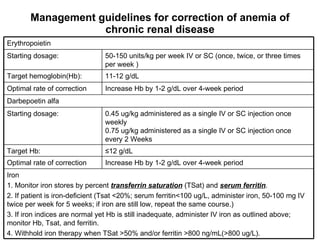
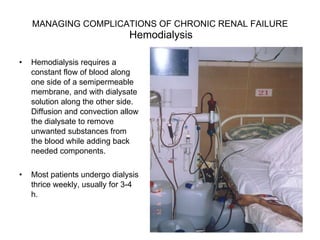
Chronic renal failure is caused by various etiologies and leads to progressive loss of kidney function. It is characterized by fluid and electrolyte abnormalities, bone disease, cardiovascular complications, anemia, and other systemic effects. Treatment focuses on slowing progression through blood pressure control and protein restriction, and managing complications through treatment of mineral metabolism disorders, anemia, and other issues.