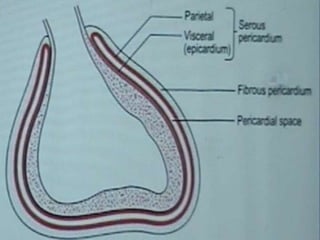
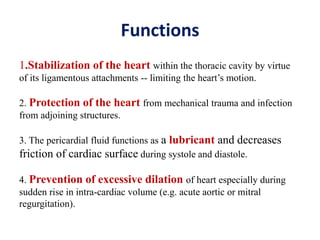
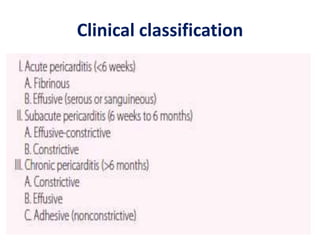
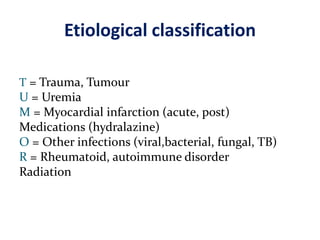
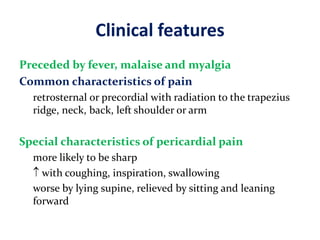
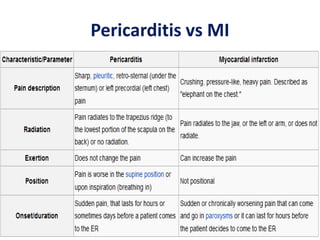
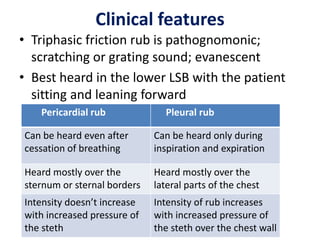
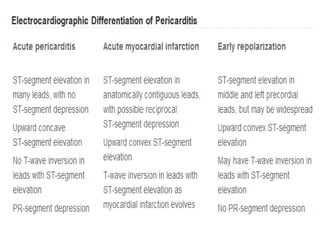
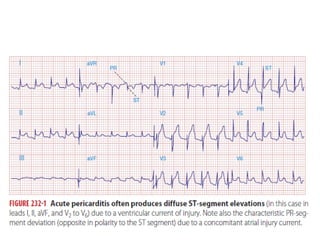
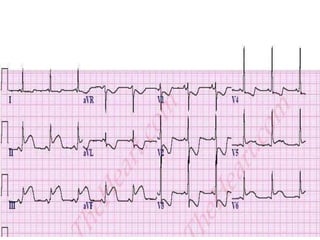
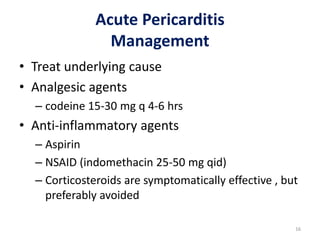
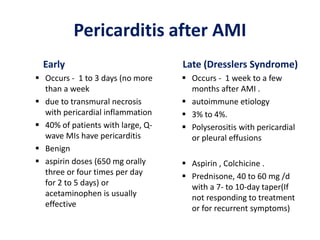
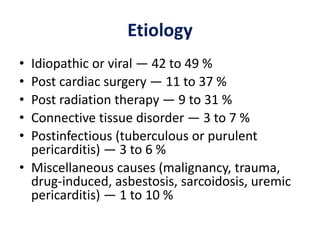
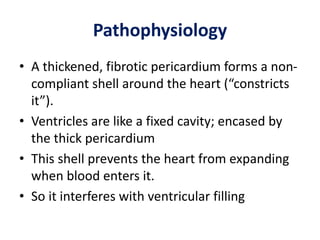
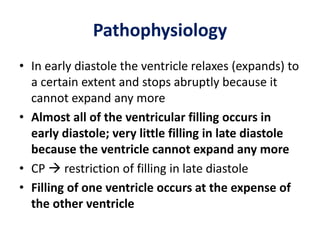
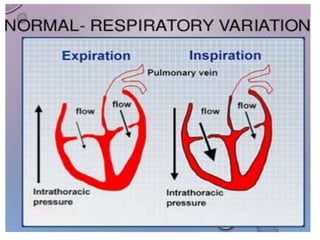
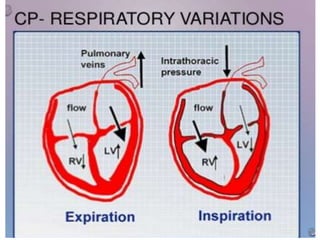
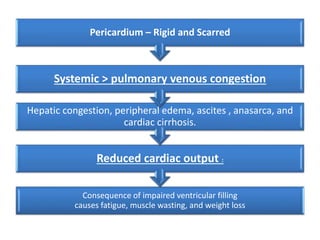
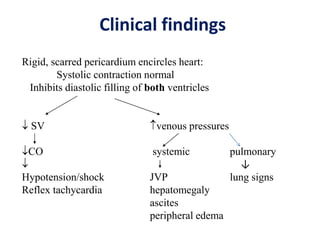
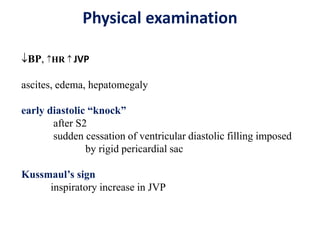
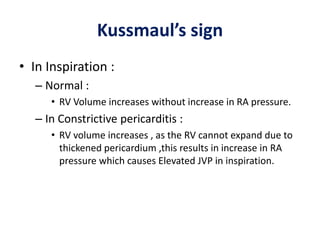
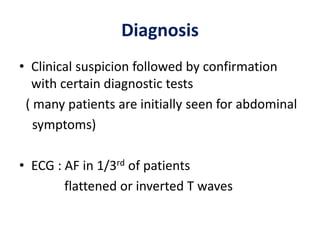
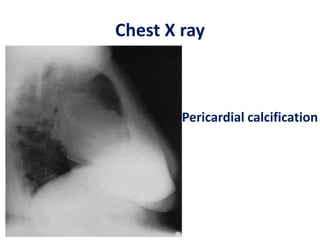
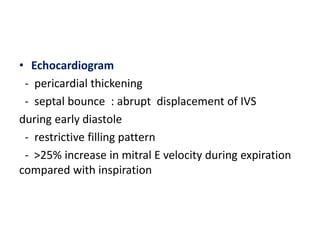
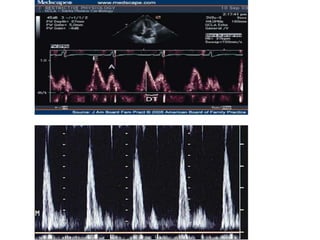
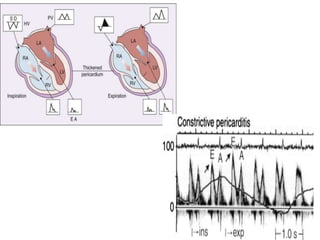
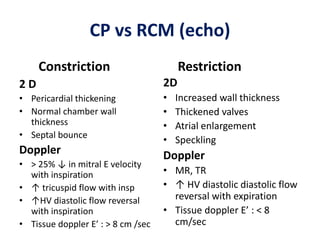
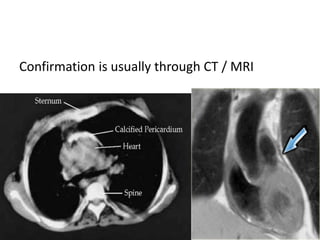
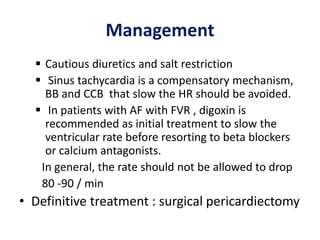
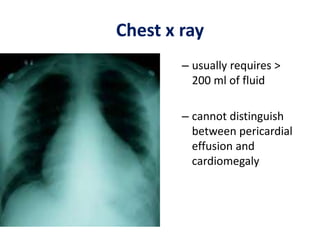
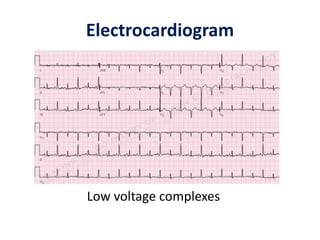
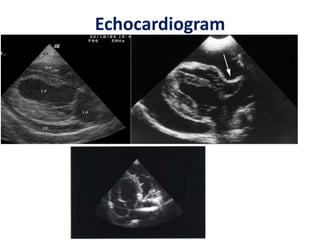
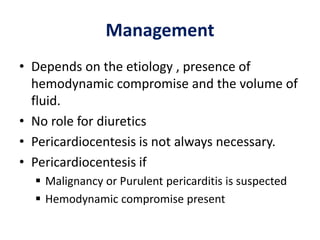
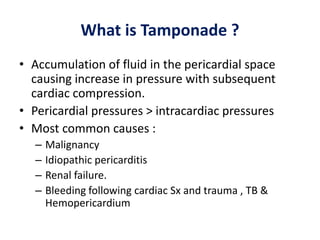
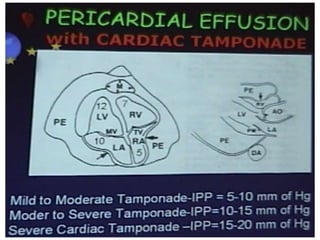
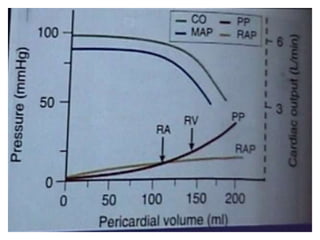
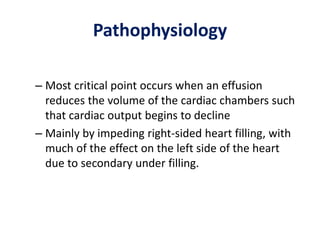
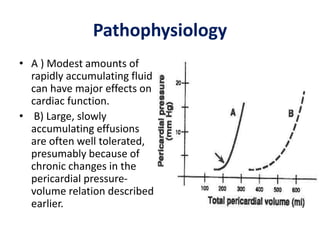
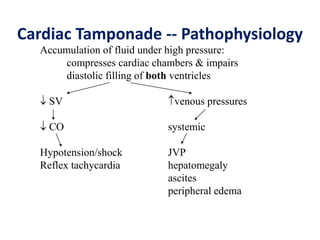
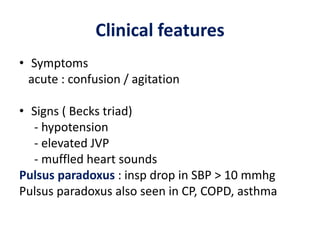
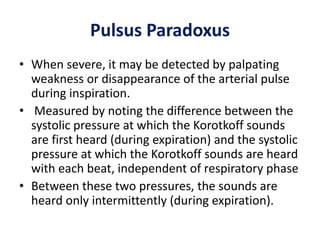
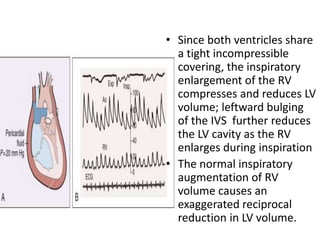
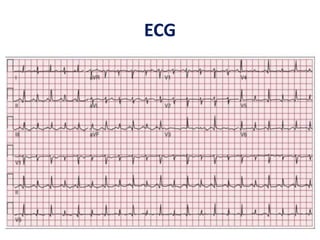
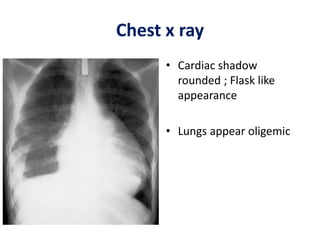
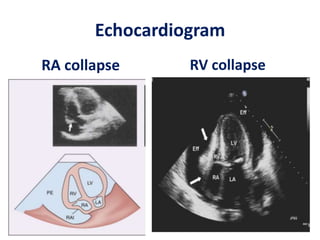
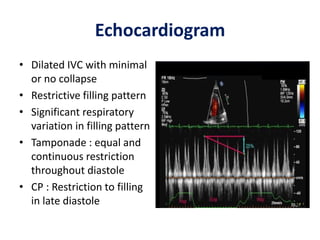
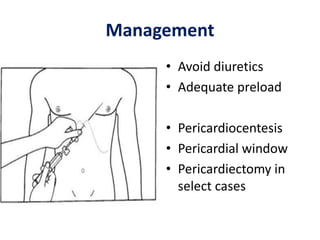
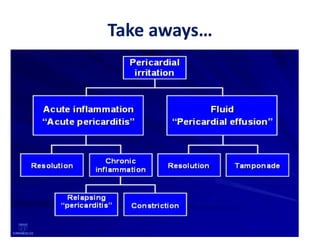
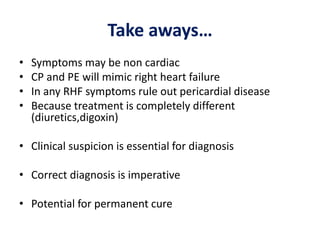
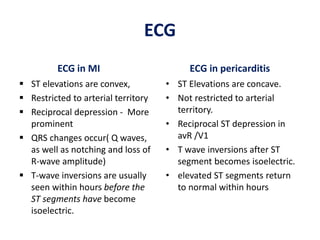
The document discusses various pericardial diseases including acute pericarditis, constrictive pericarditis, pericardial effusion, and cardiac tamponade. It provides details on the anatomy and functions of the pericardium, pathophysiology, clinical features, diagnostic tests, and management of these conditions. Key points include that pericardial diseases can present with non-specific symptoms, clinical suspicion is important for diagnosis, and treatment depends on underlying etiology and presence of hemodynamic compromise. Differentiating constrictive pericarditis from restrictive cardiomyopathy is important as treatment approaches differ significantly.