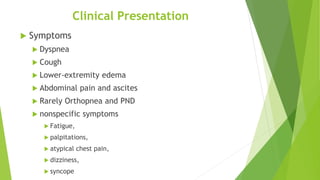
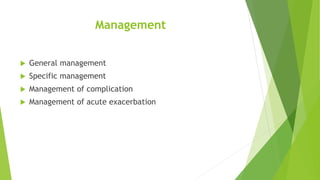
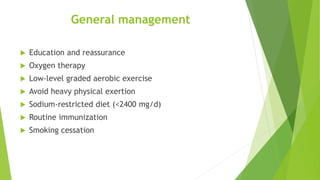
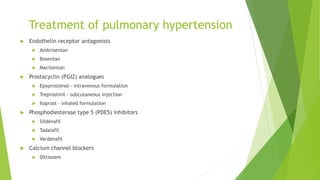
Cor pulmonale refers to the structural and functional alteration of the right ventricle caused by respiratory disorders, primarily chronic obstructive pulmonary disease (COPD), with symptoms including dyspnea and edema. It can be classified into acute and chronic forms, with the pathophysiology linked to pulmonary hypertension and various lung diseases leading to right ventricular overload. Management strategies include treating underlying causes, oxygen therapy, and medications to manage pulmonary hypertension, while prognosis varies based on the underlying condition.
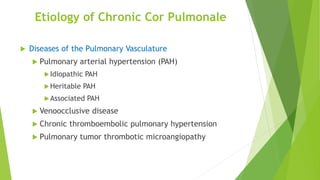
![ The World Health Organization (WHO) has five classifications for pulmonary
hypertension, and all except one of these groups can result in cor pulmonale
(WHO Classification group 2 is pulmonary artery hypertension due to left
ventricular [LV] dysfunction).
Group 1: Pulmonary artery hypertension, including heritable causes;
connective-tissue disorders, including scleroderma; and other idiopathic
causes.
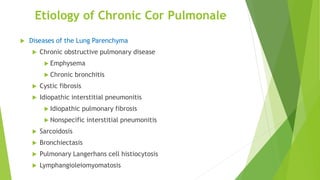
Group 3: Pulmonary hypertension due to lung disease and/or hypoxia; these
disorders include chronic obstructive pulmonary disease (COPD), which is the
most common cause of for pulmonale. There have been studies correlating
the degree of hypoxia with the severity of cor pulmonale. Other disorders
that can result in cor pulmonale in this group include interstitial lung disease
(ILD) and obstructive sleep apnea (OSA)](https://image.slidesharecdn.com/corpulmonale-240616191230-75ed4866/85/Seminar-presentation-on-cor-pulmonale-pptx-8-320.jpg)