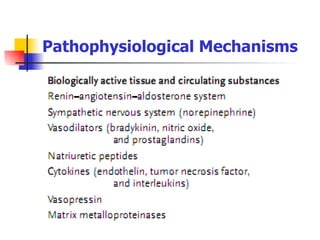
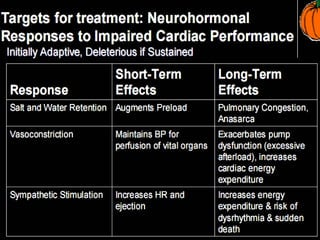
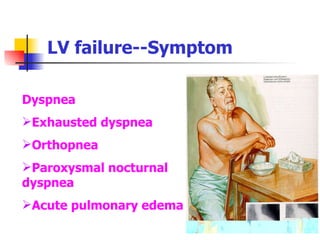
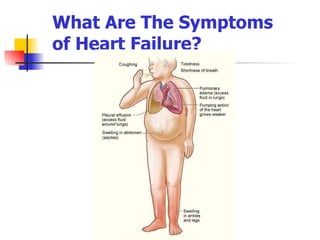
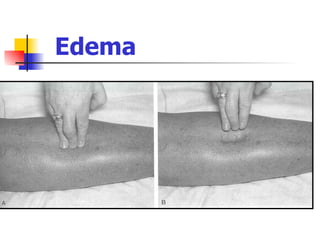
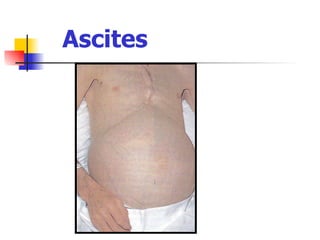
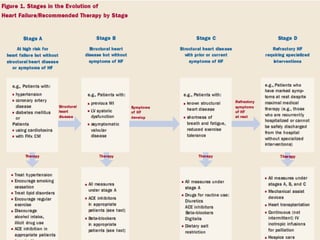
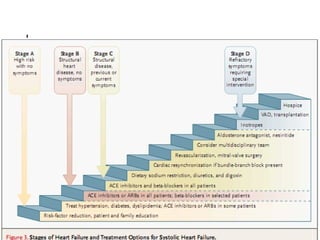
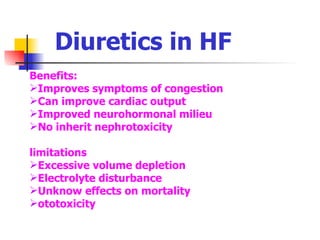
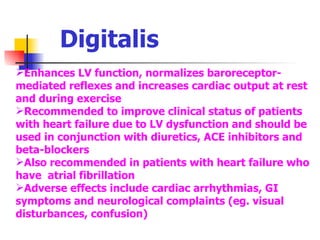
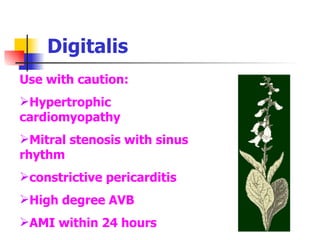
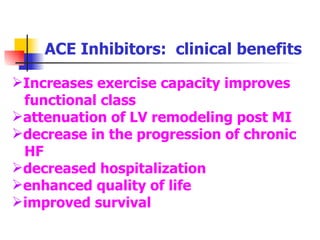
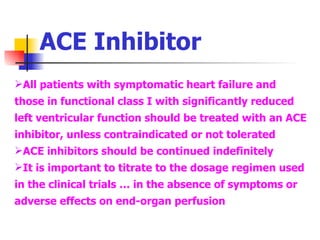
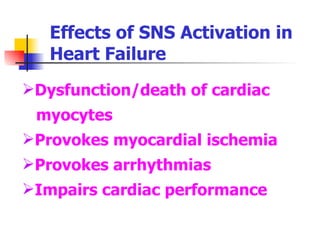
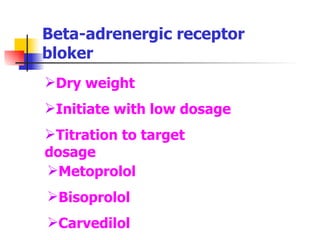
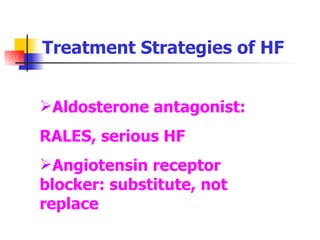
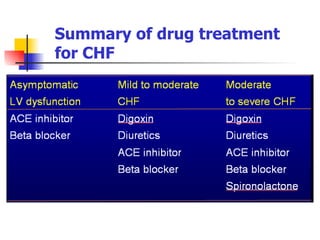
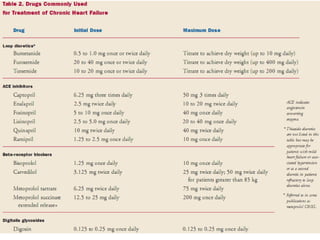
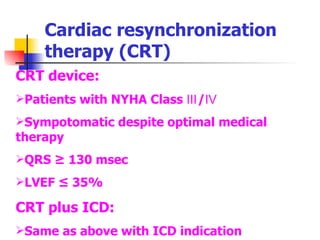
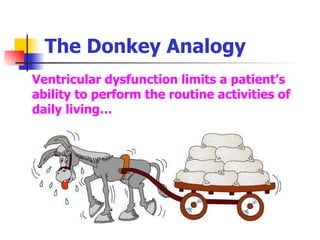
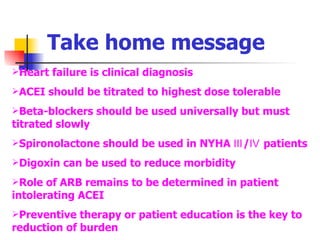
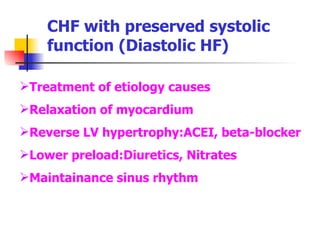
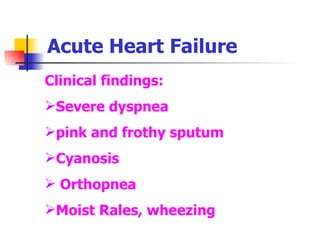
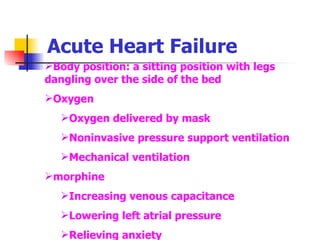
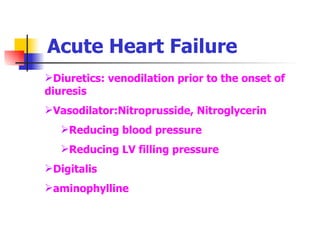
Heart failure is a condition where the heart cannot pump enough blood to meet the body's needs. It affects over 5 million Americans. The prevalence increases with age, reaching nearly 10% in those over 80. Symptoms include fatigue, shortness of breath, swelling, and more. Treatment focuses on reducing cardiac workload through diuretics, beta blockers, ACE inhibitors, and other drugs. Device therapies like CRT can also help certain patients. Lifestyle changes and strict medication adherence are important for managing the condition.