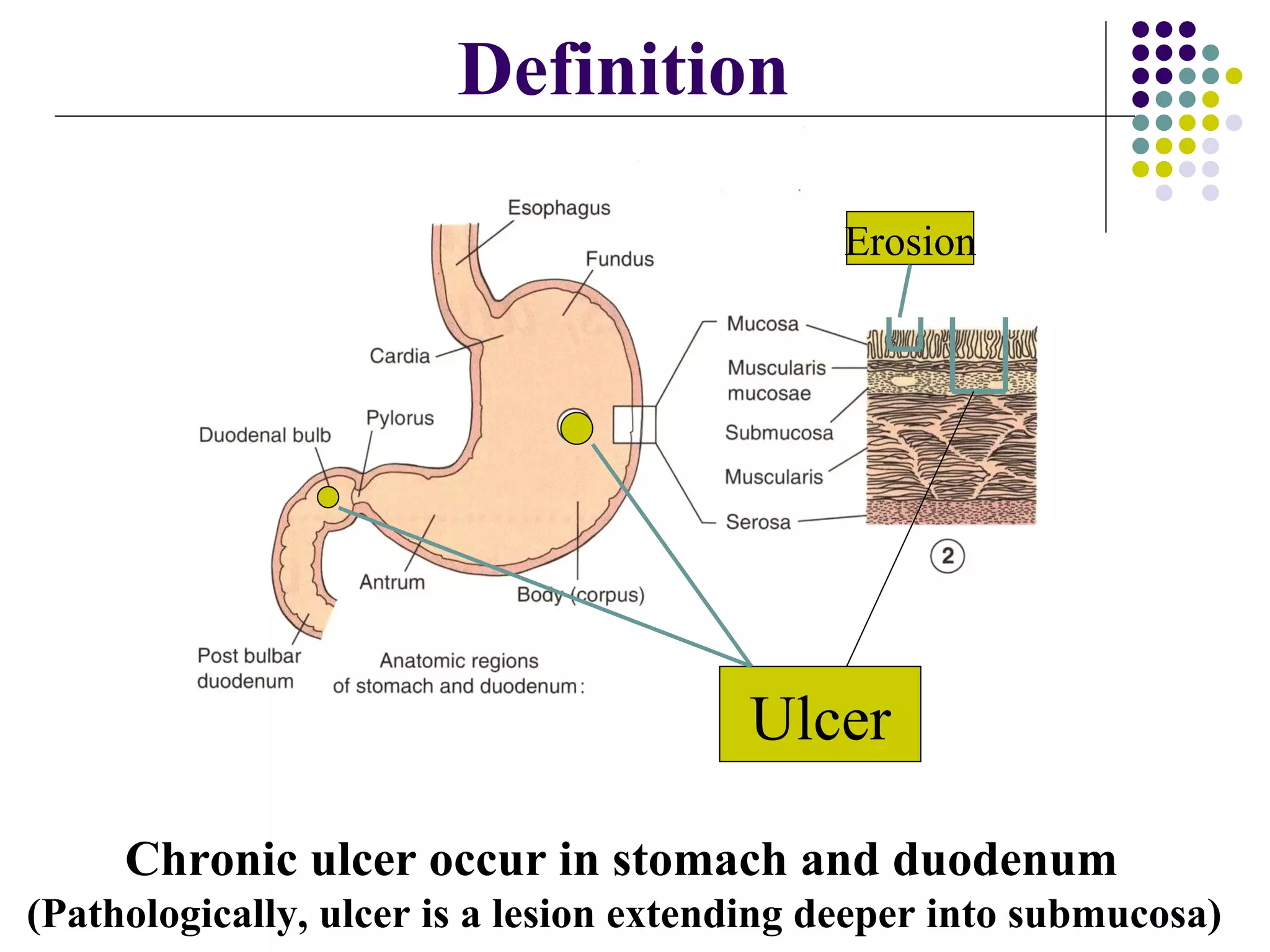
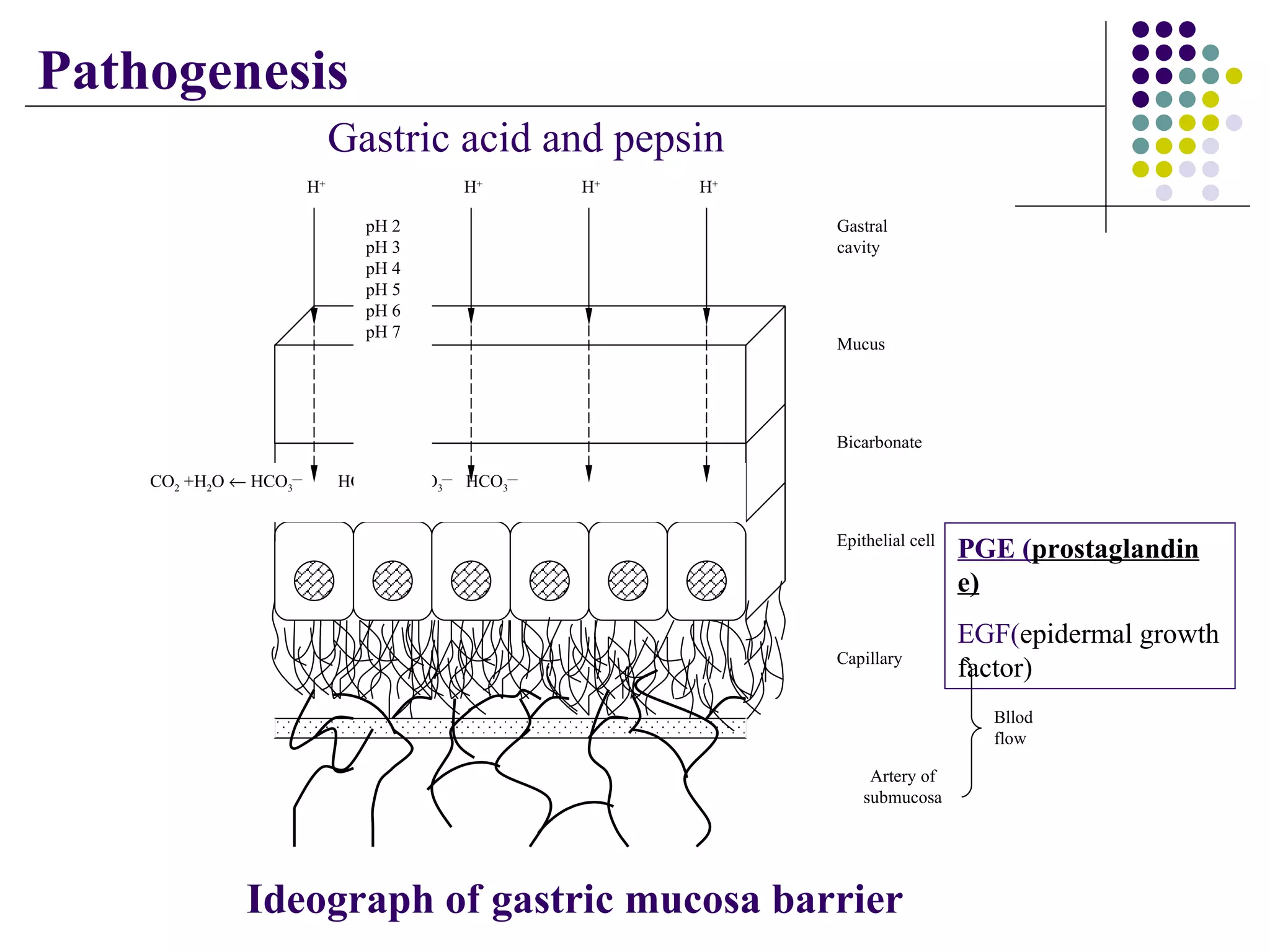
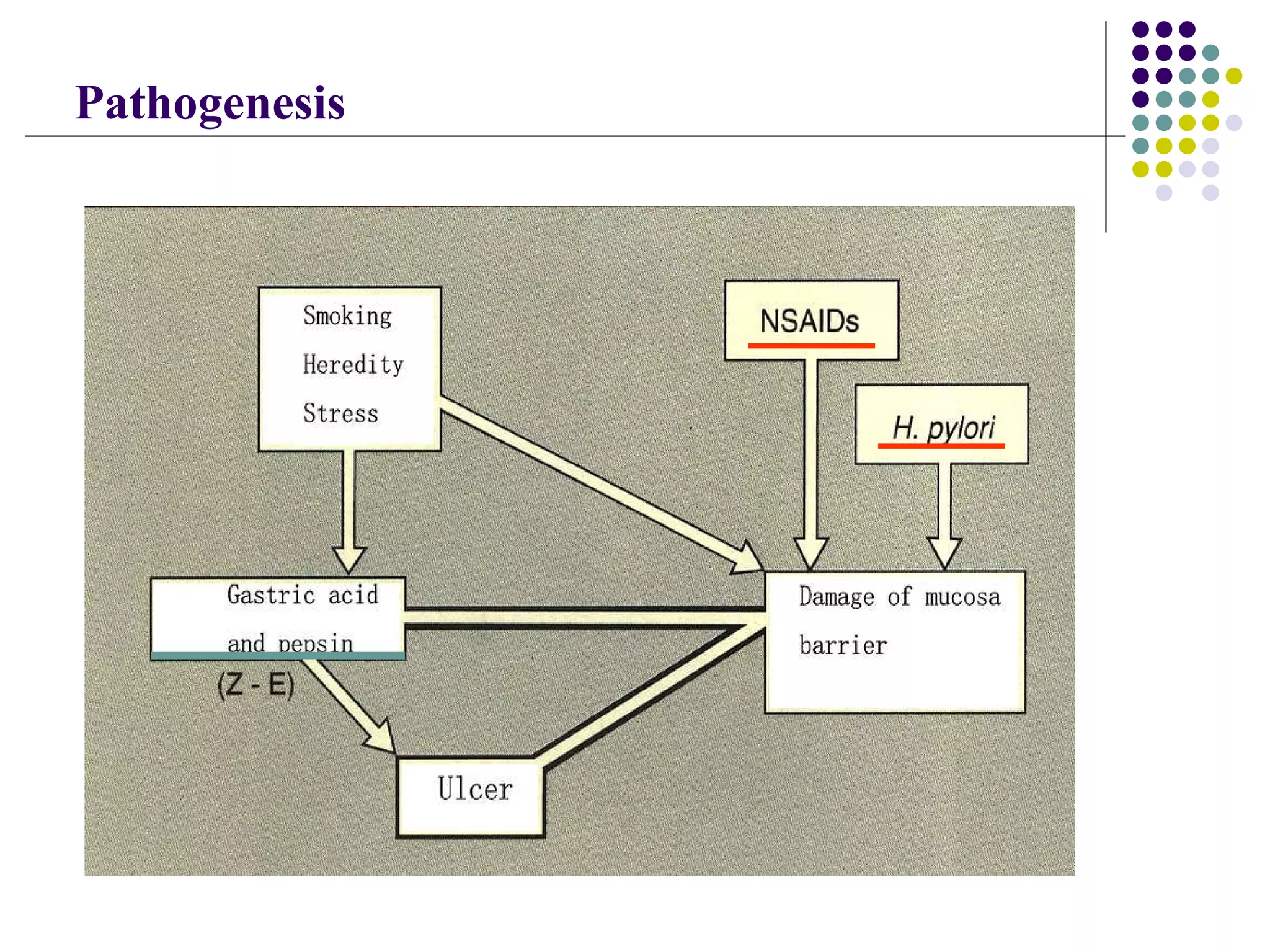
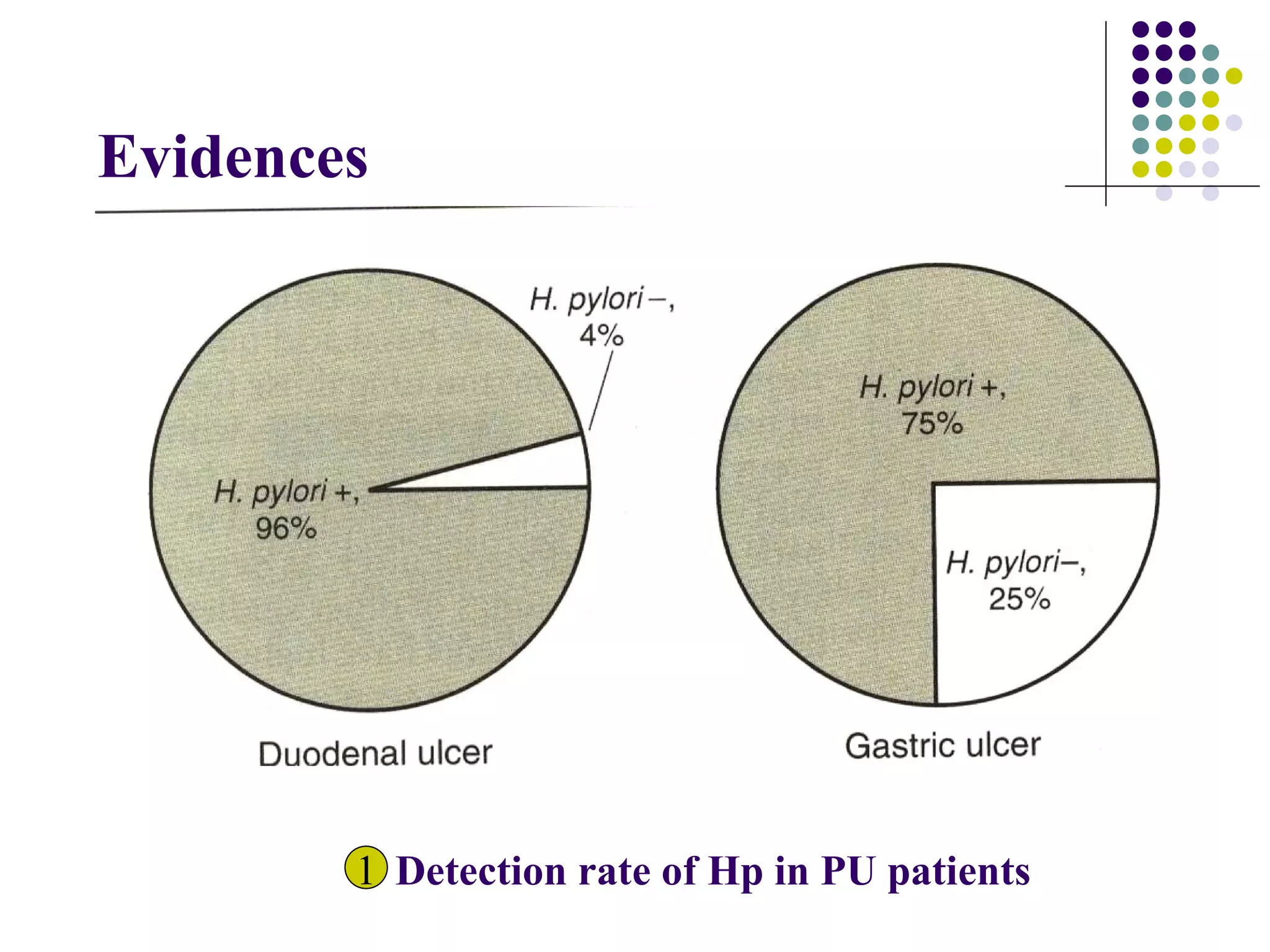
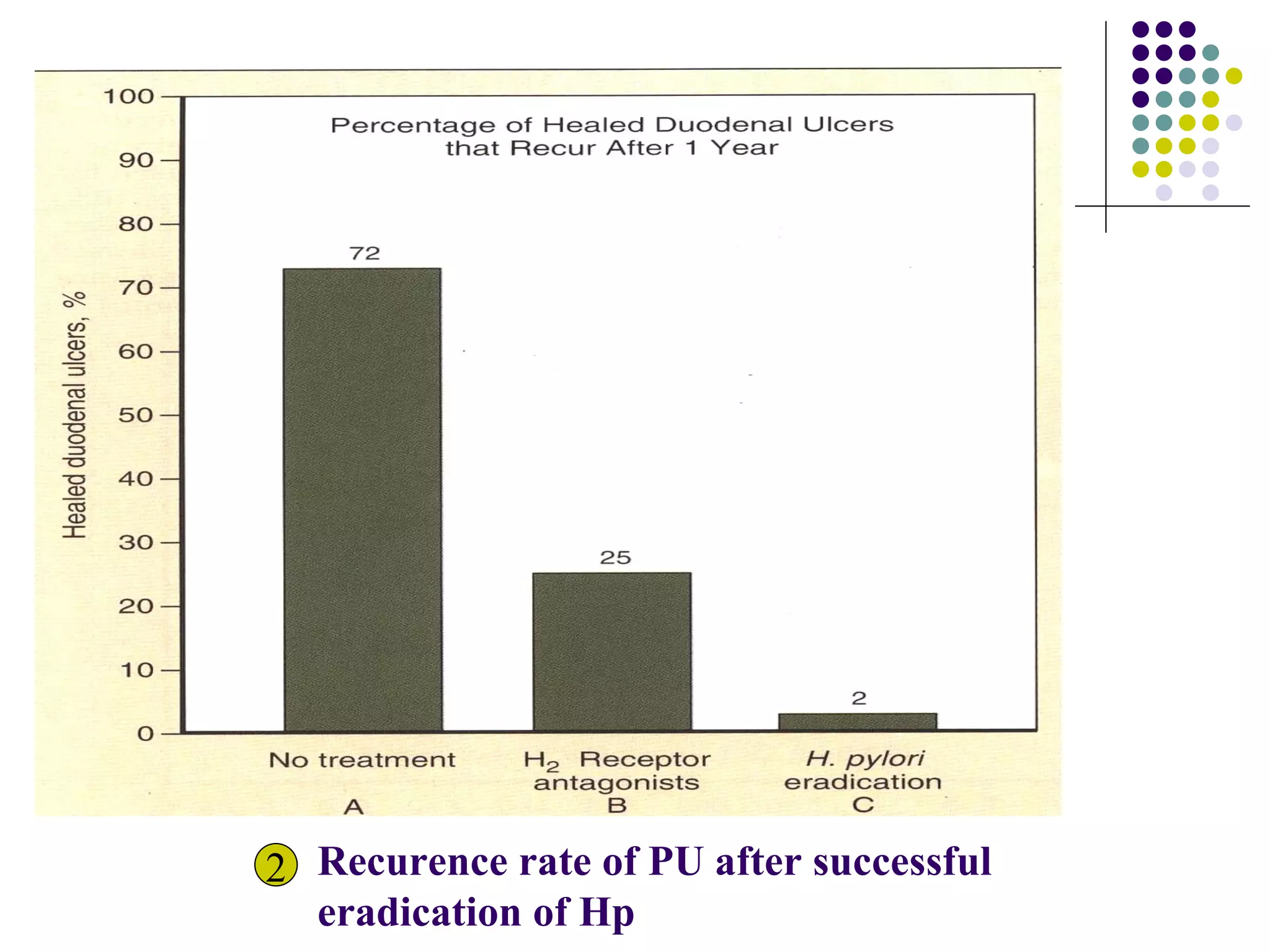
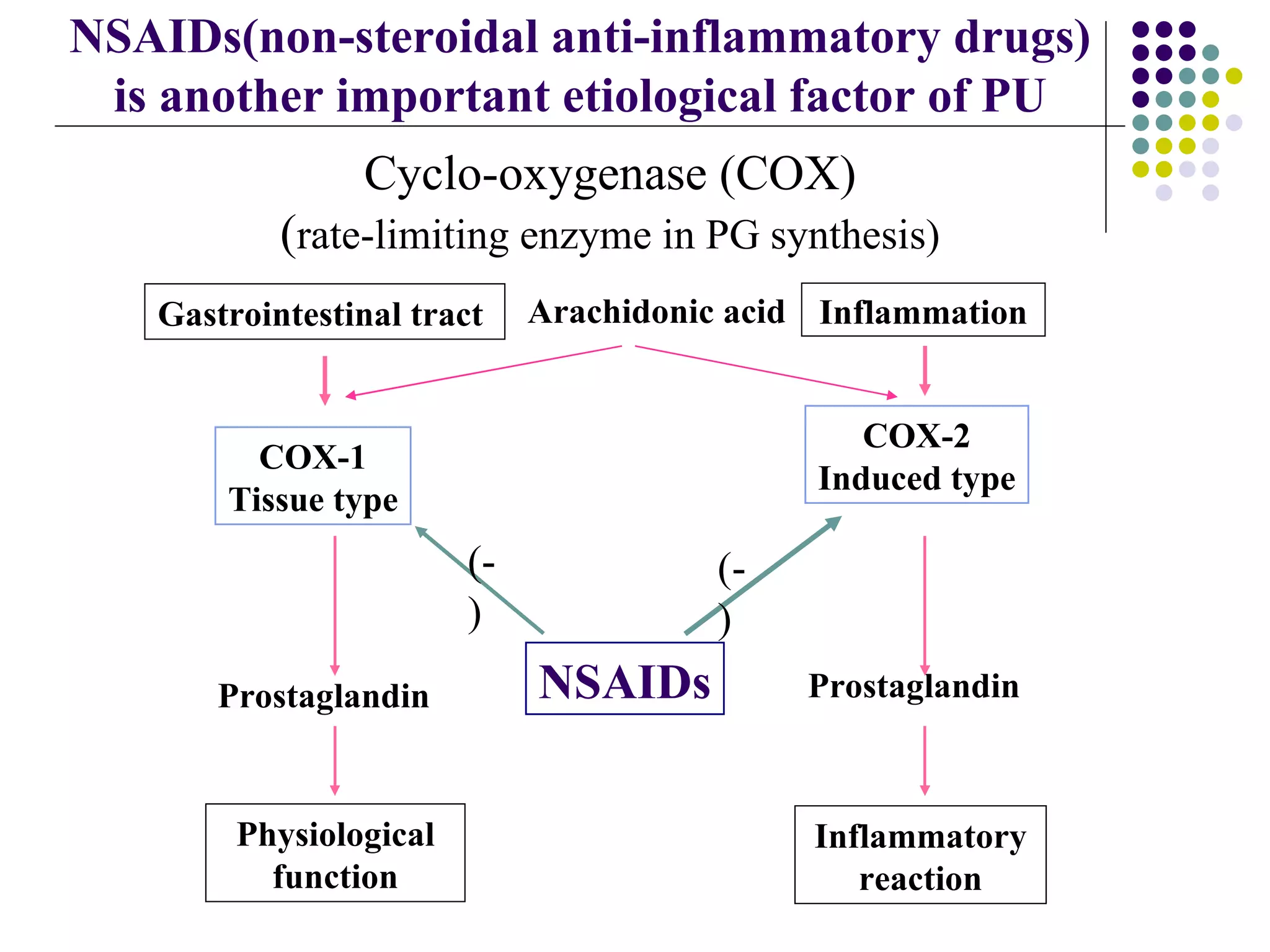
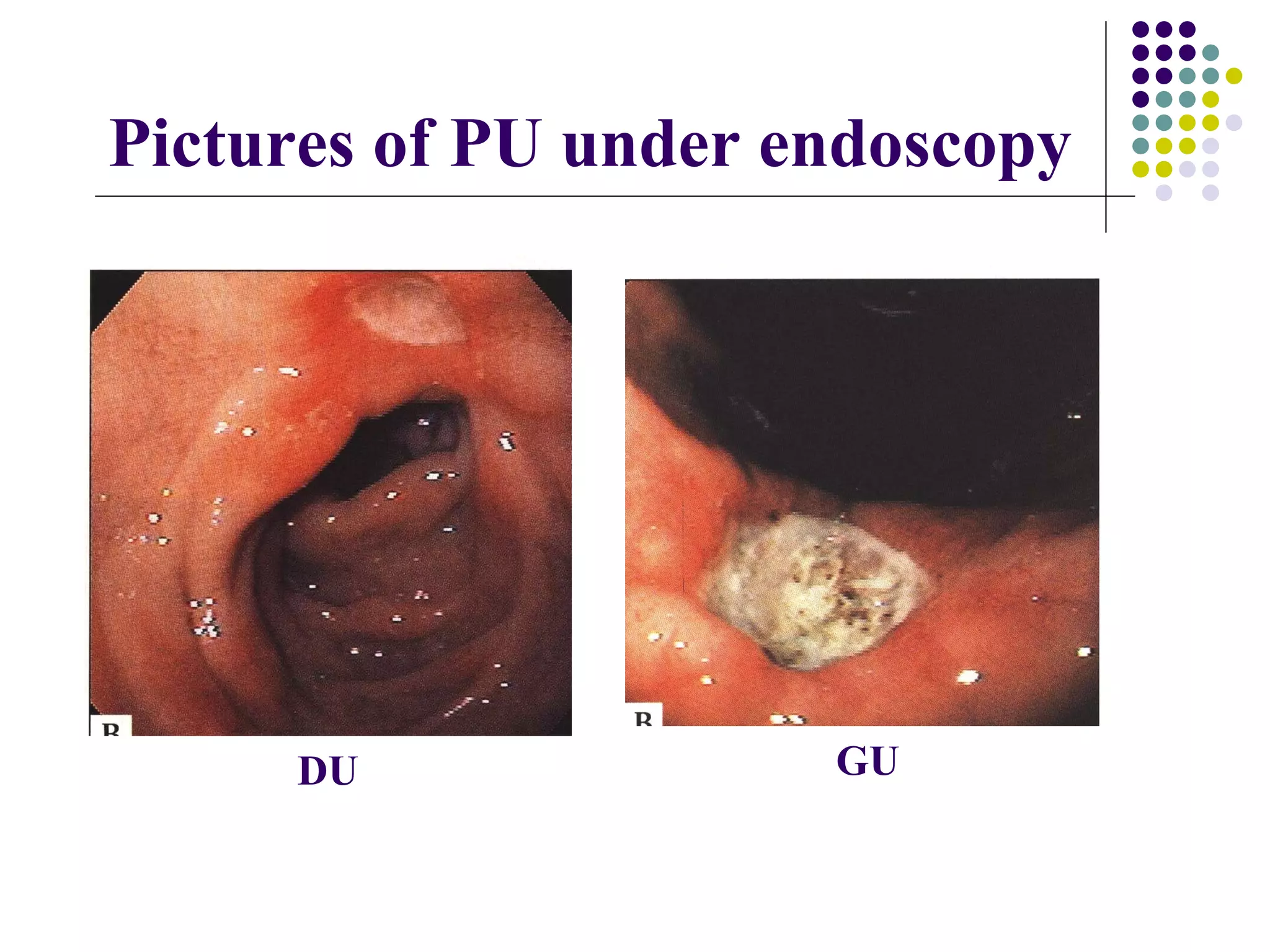
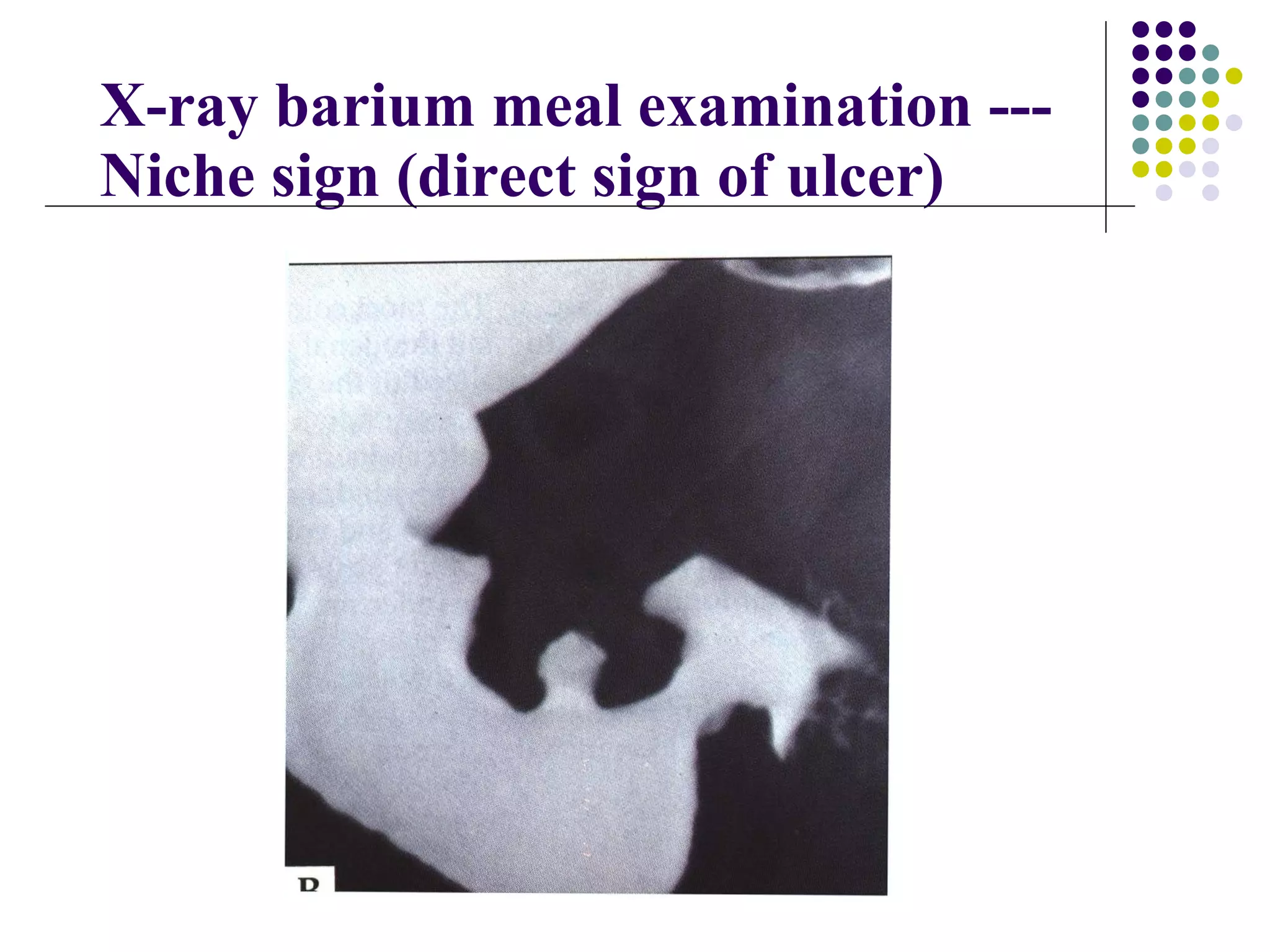
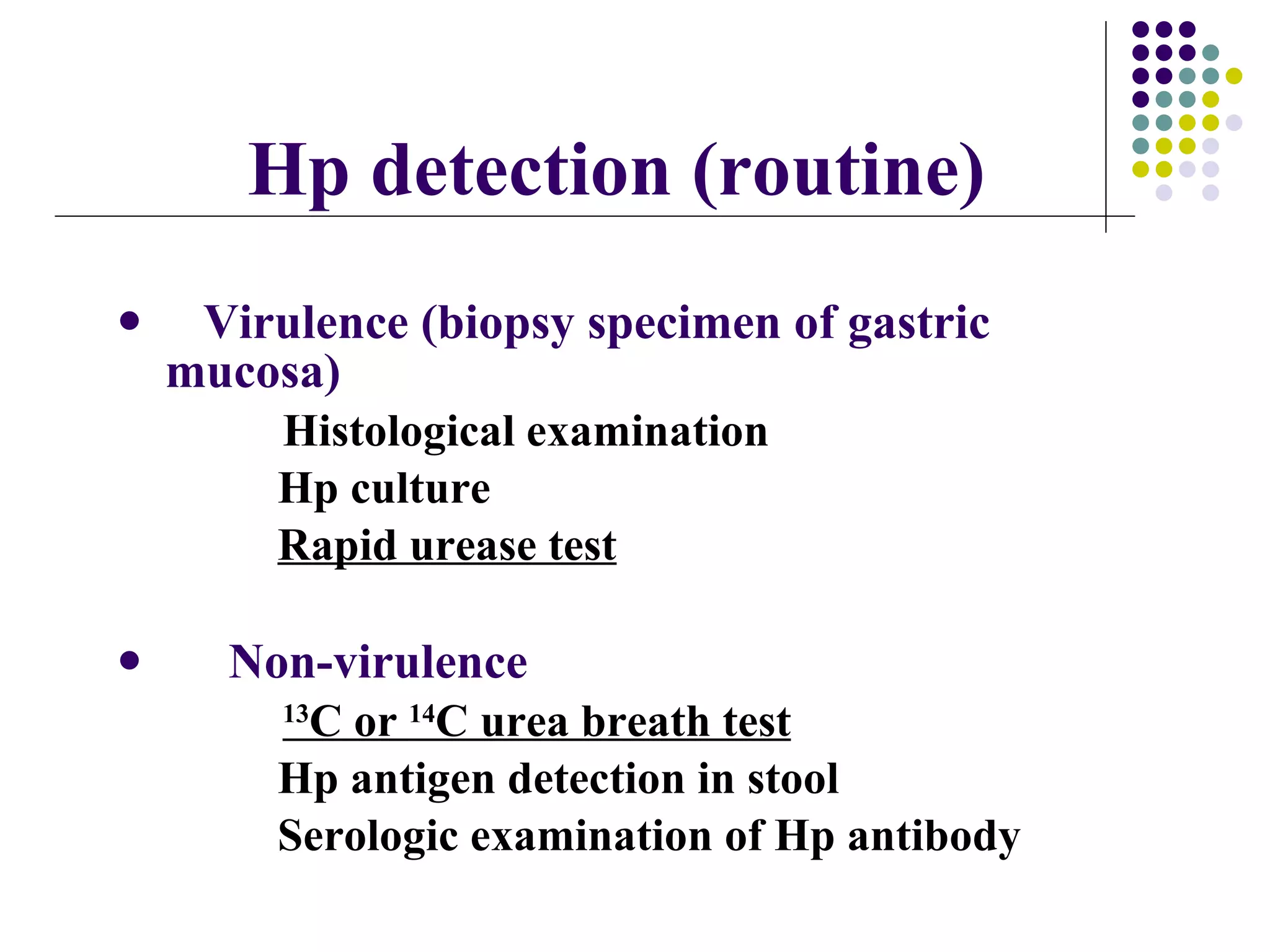
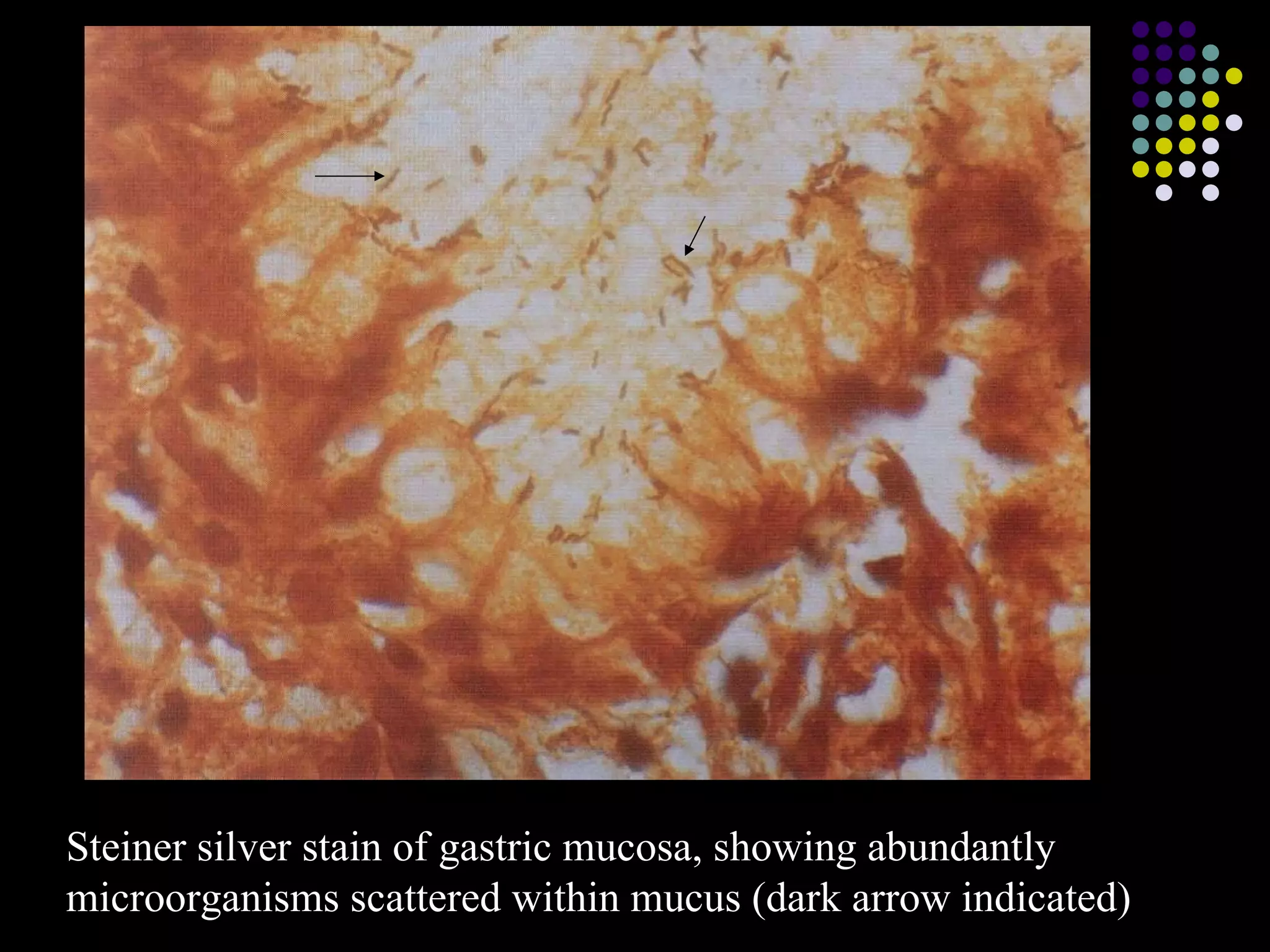
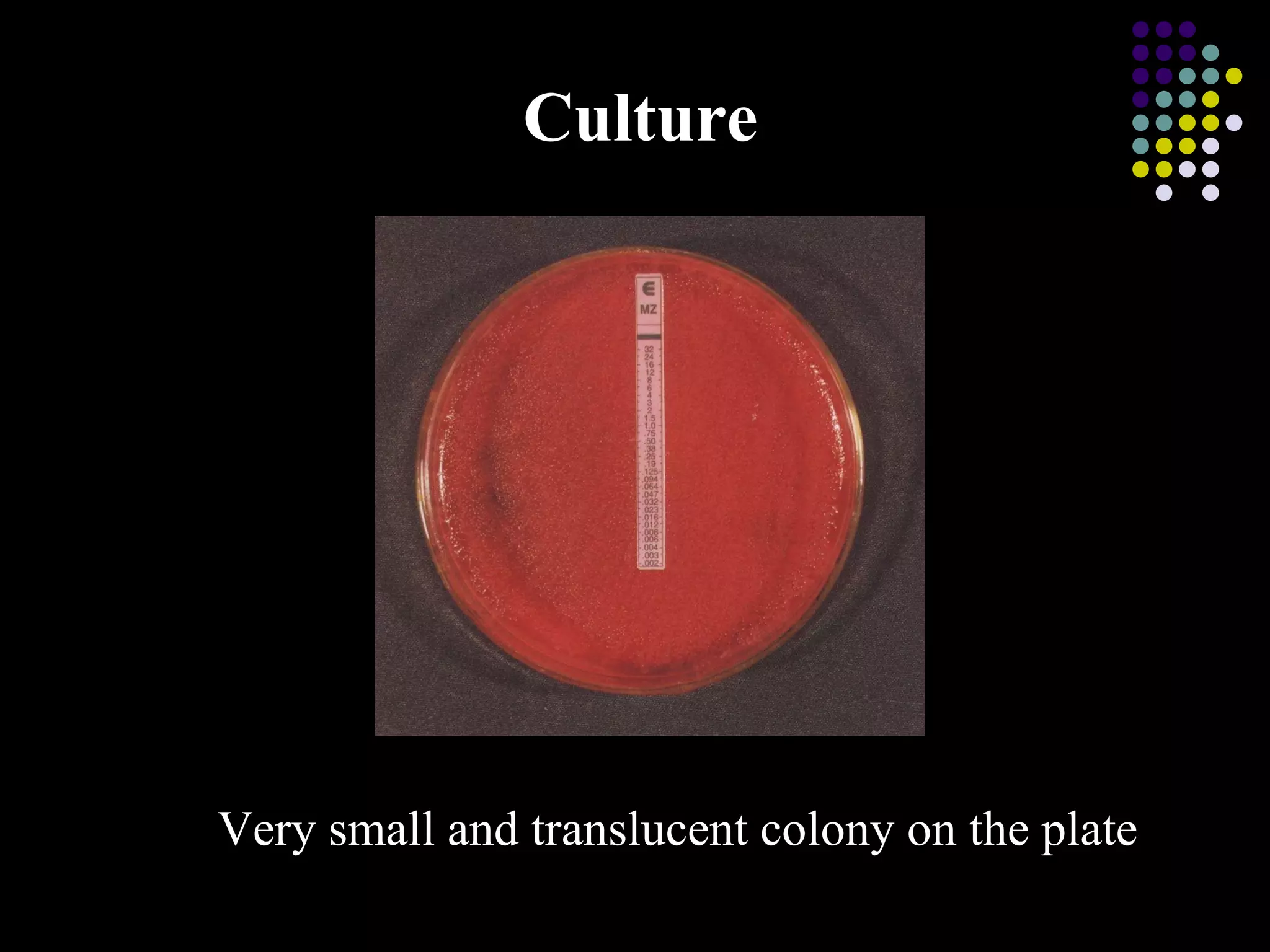
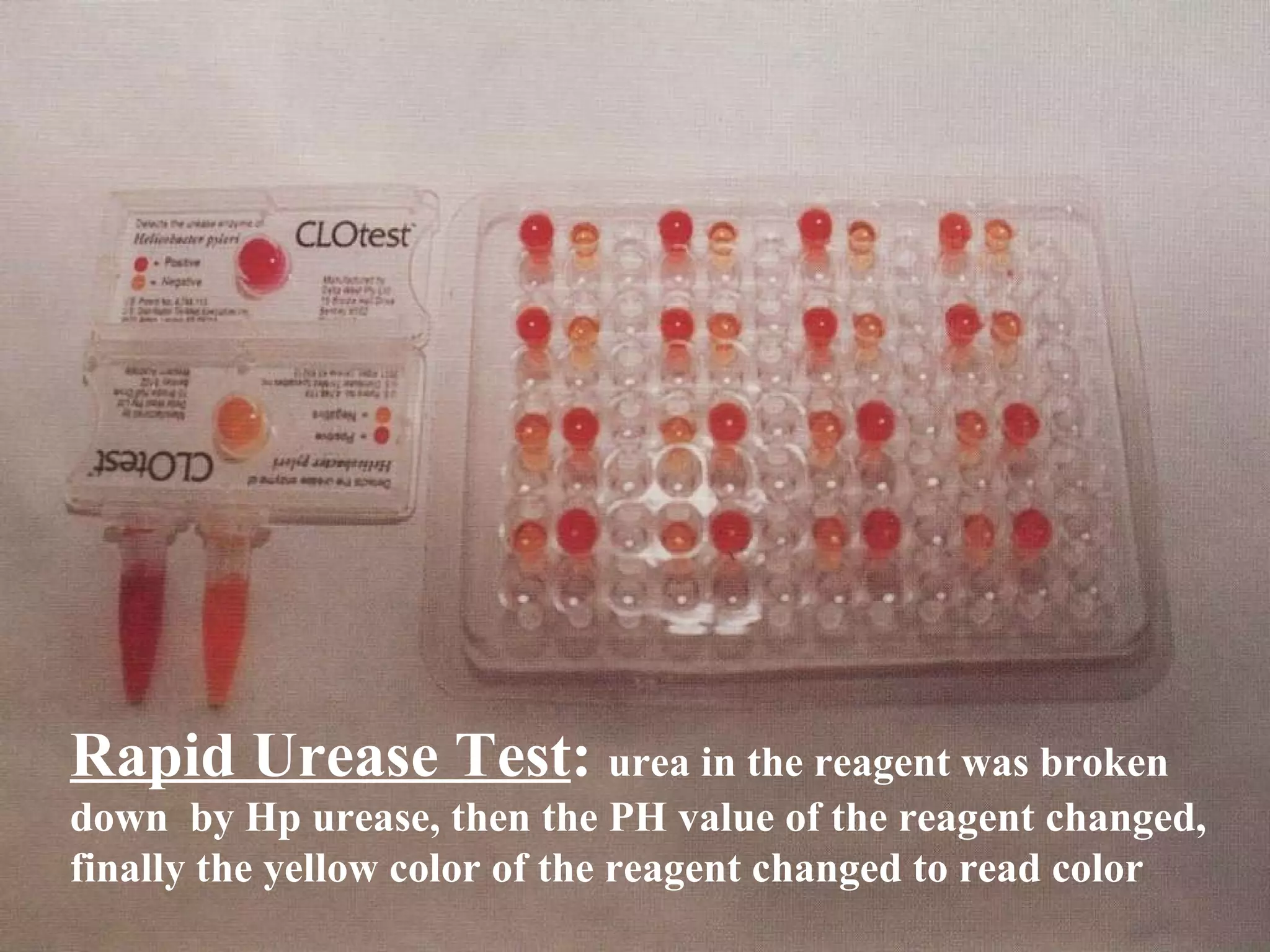
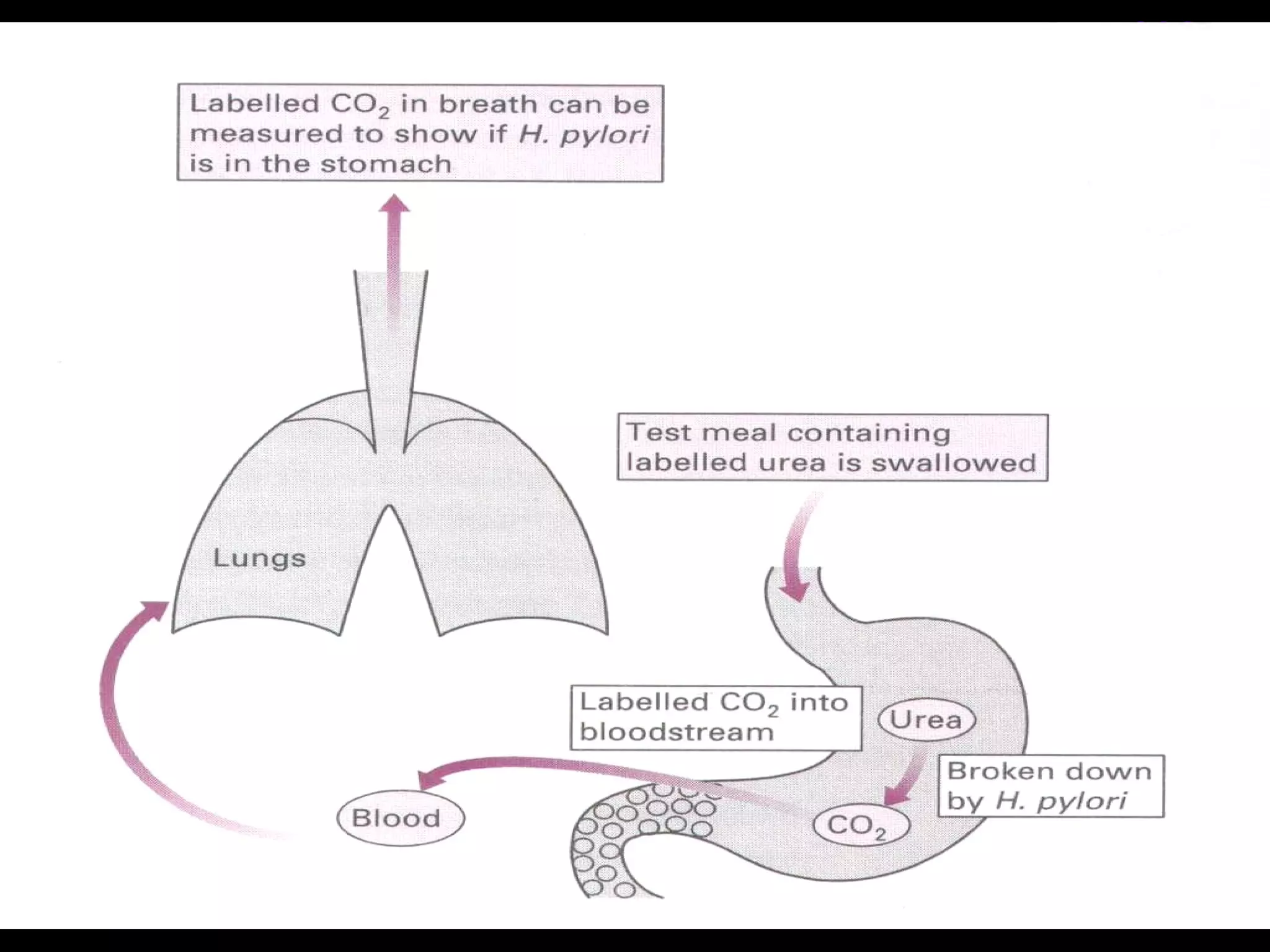
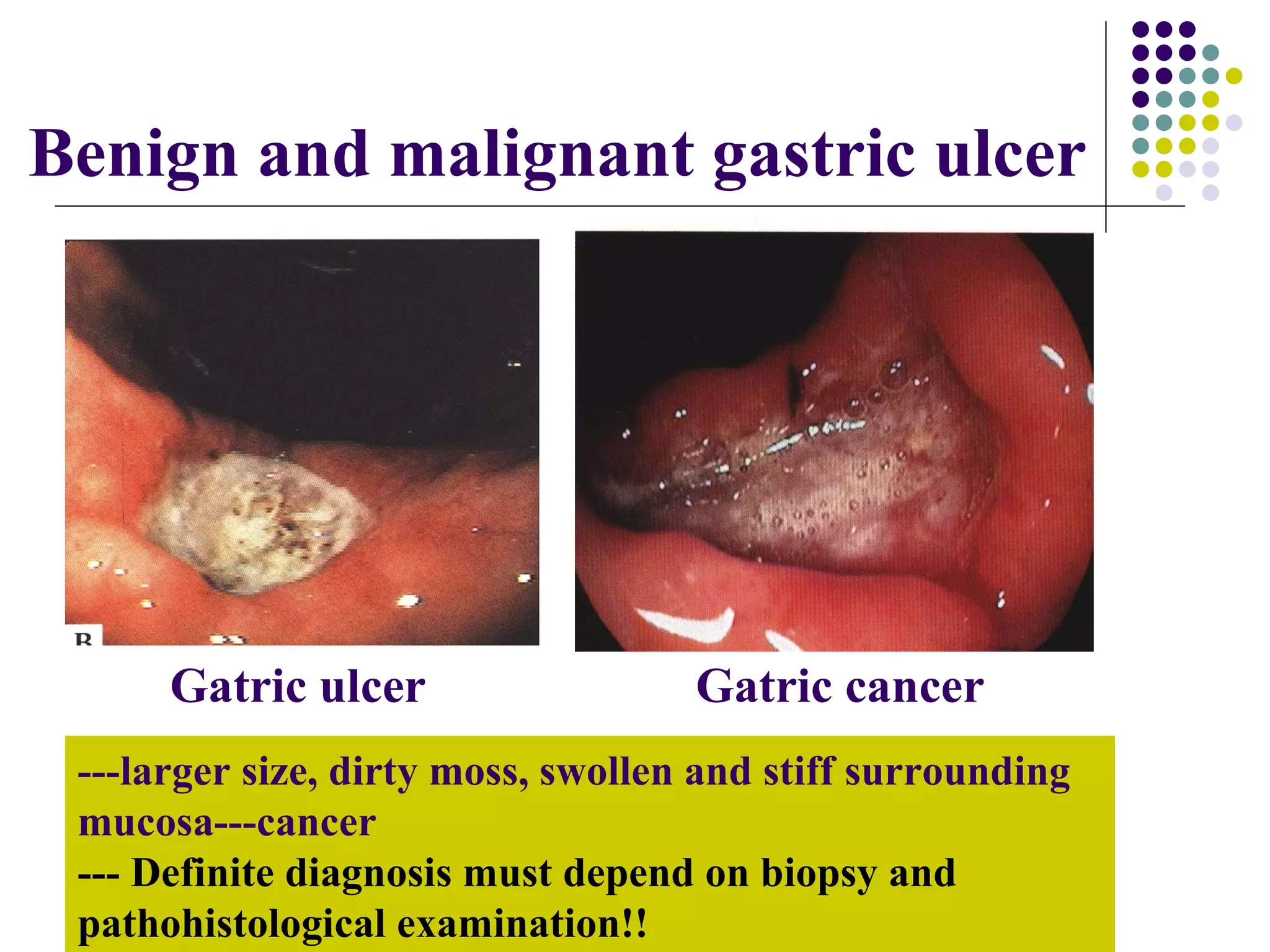
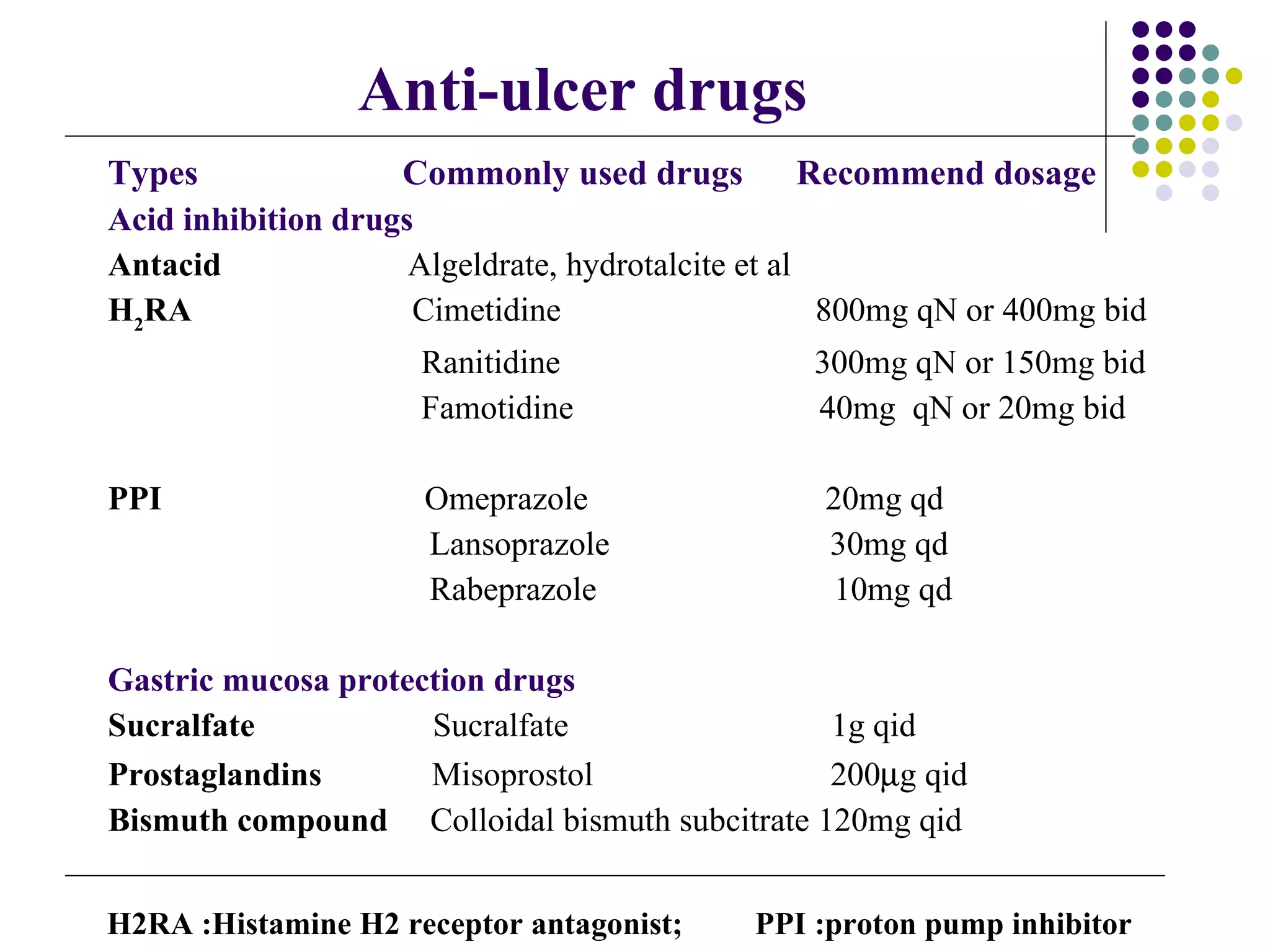
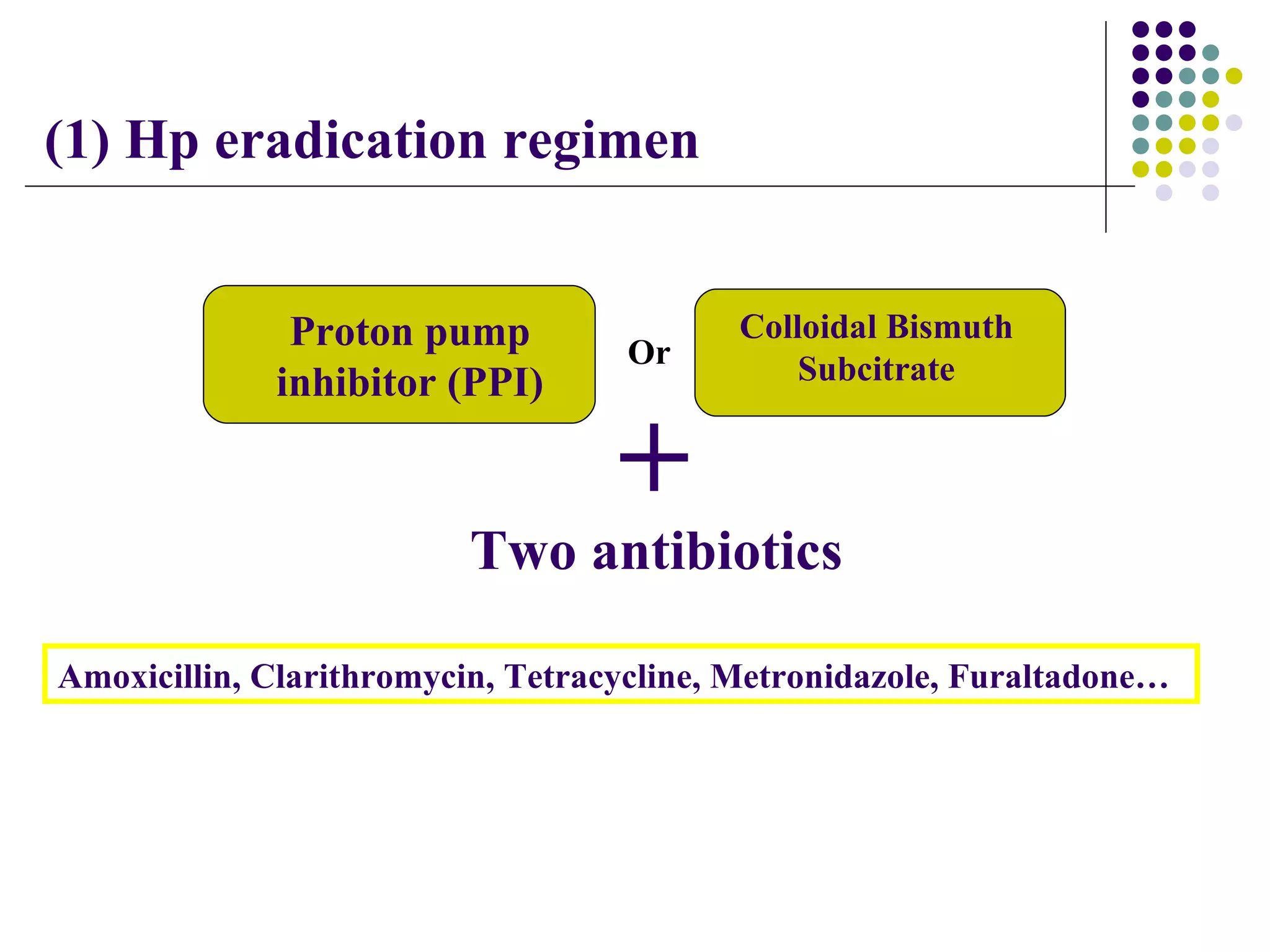
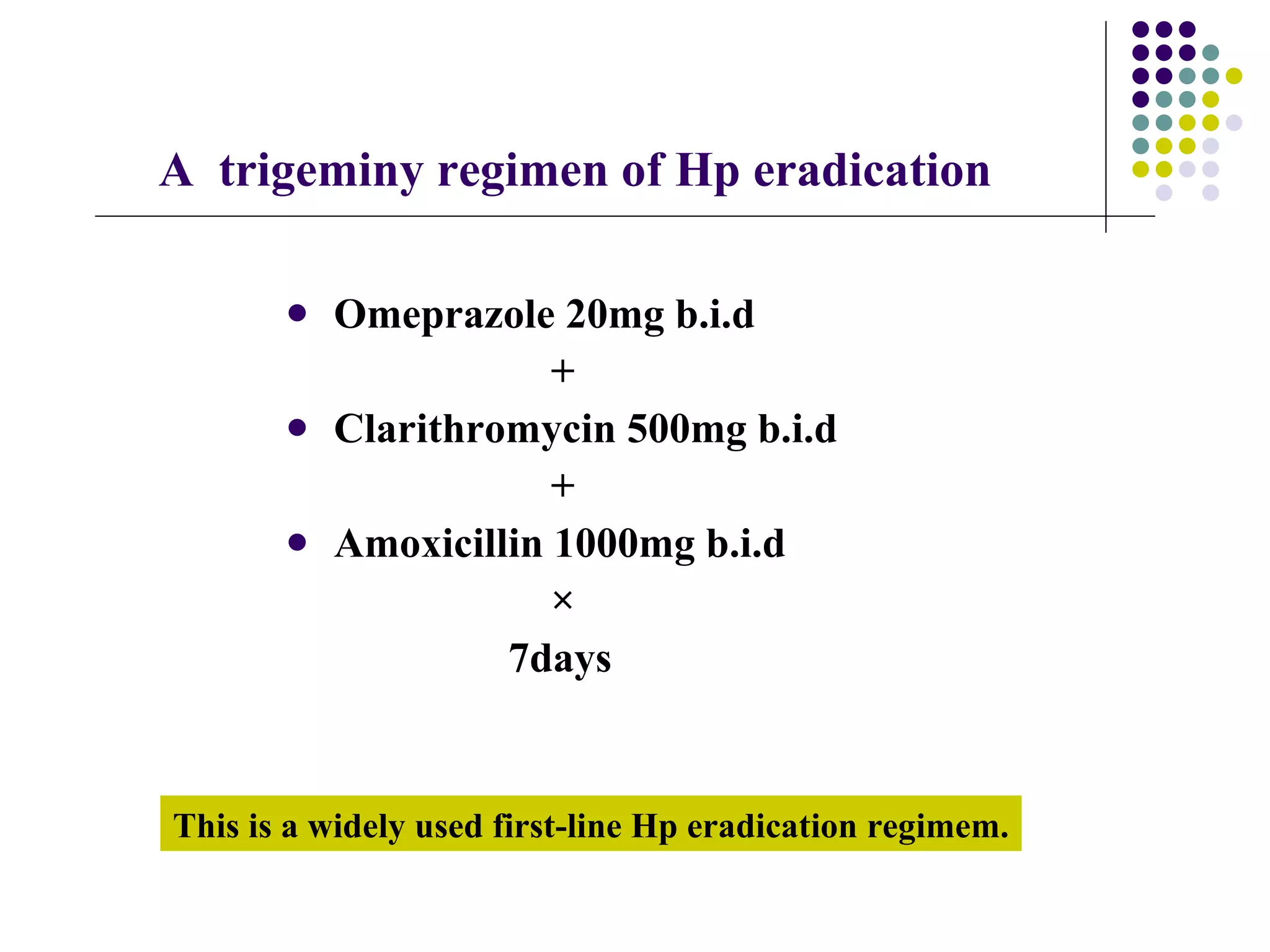
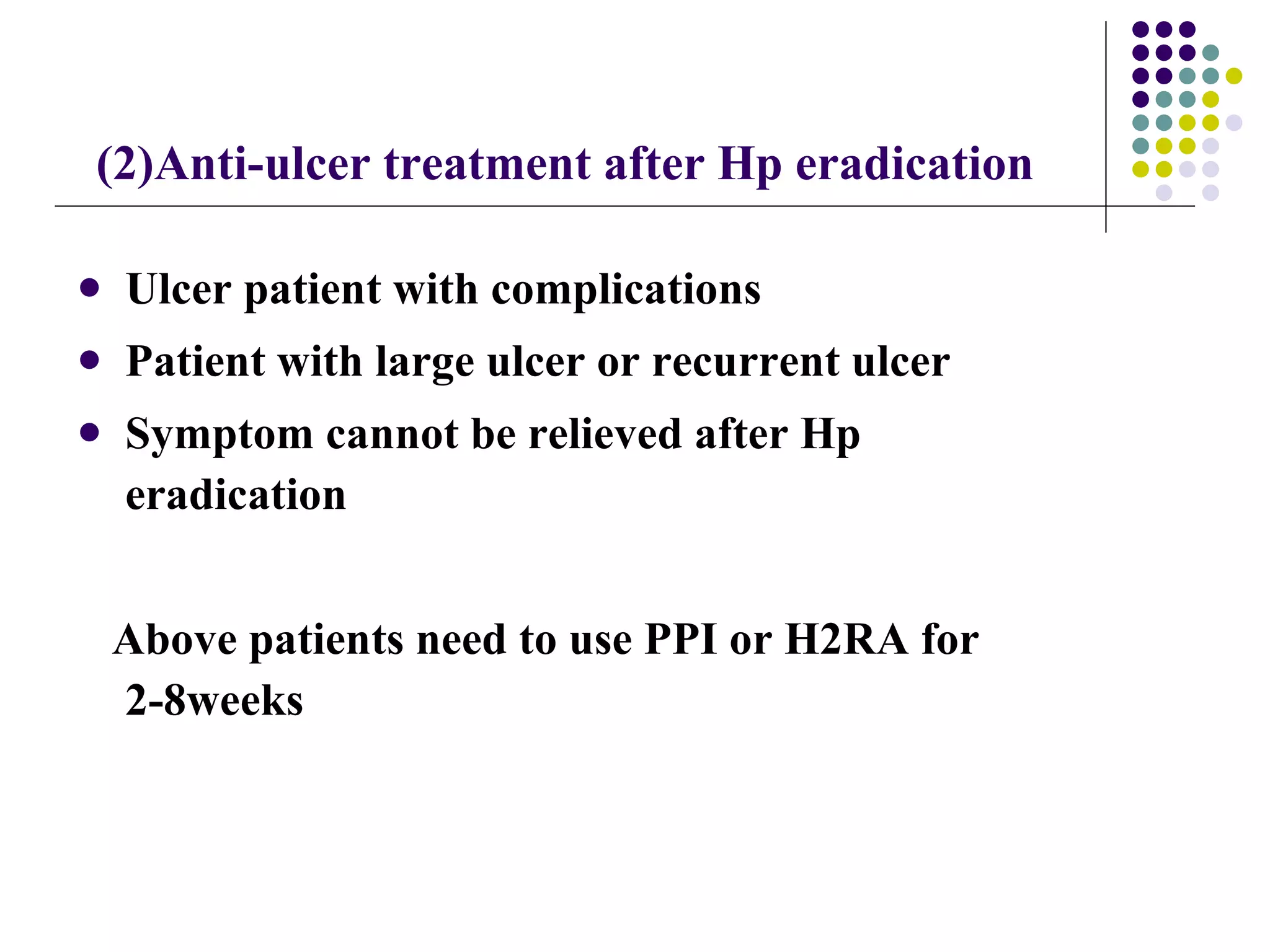
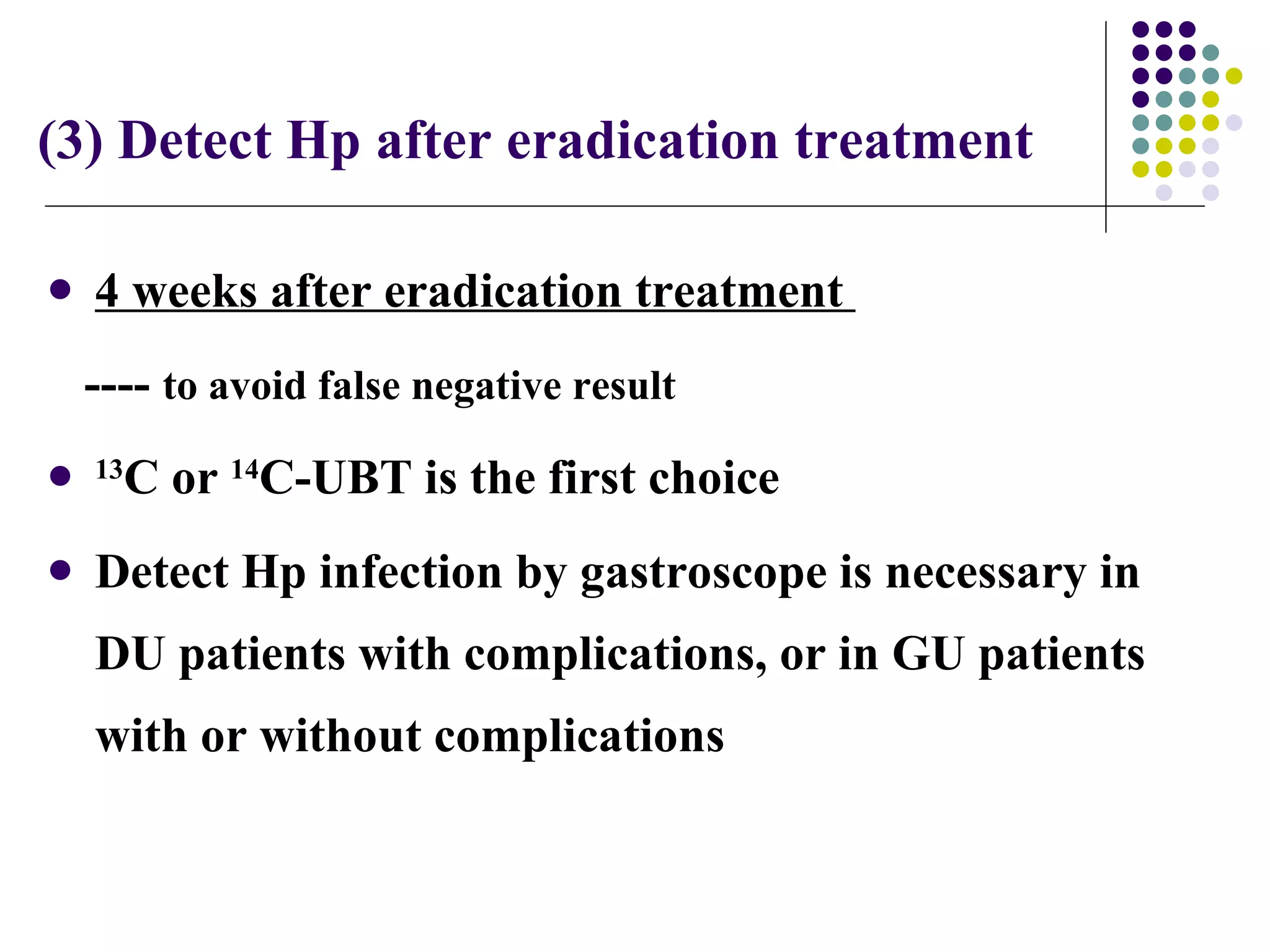
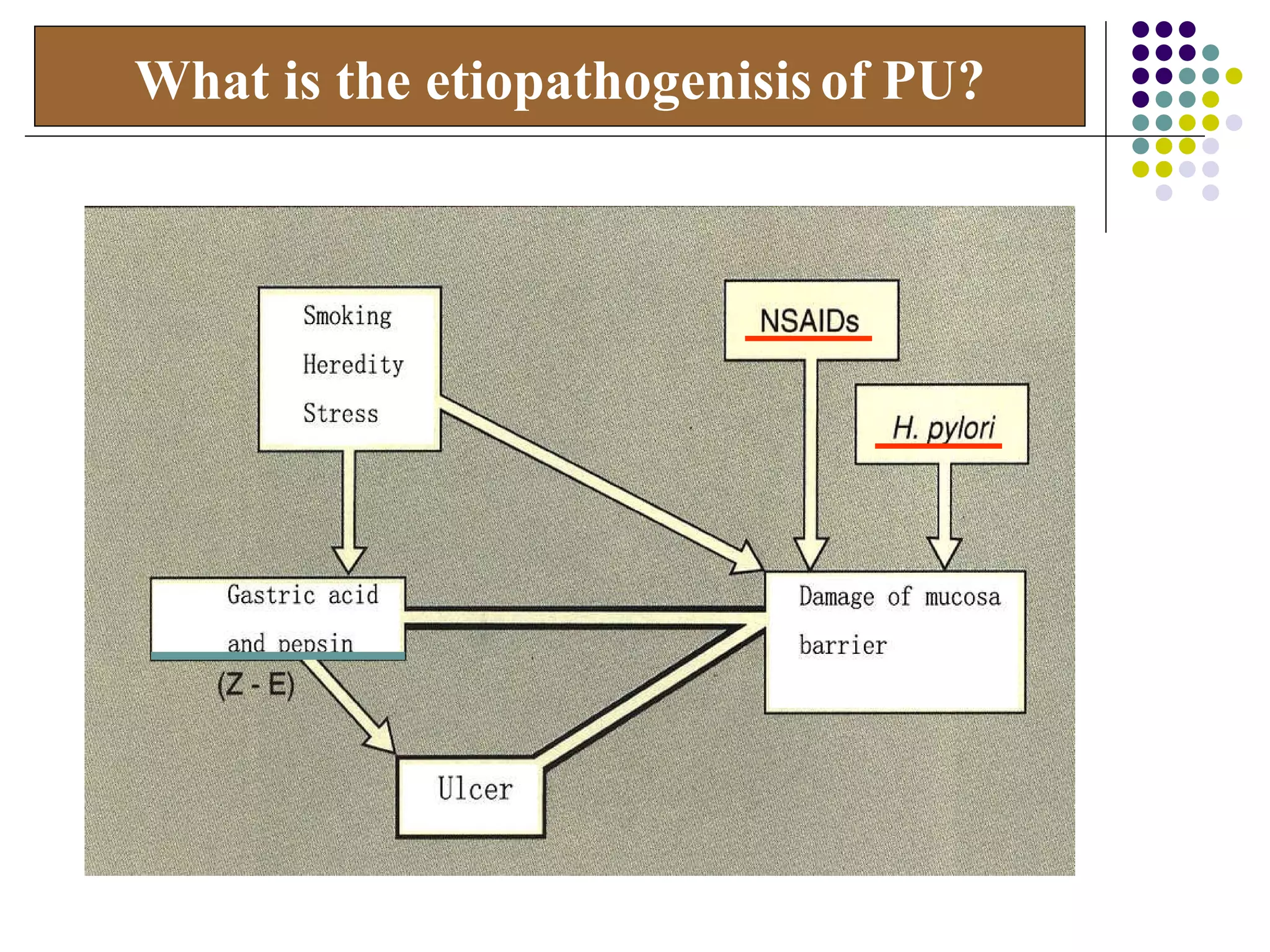
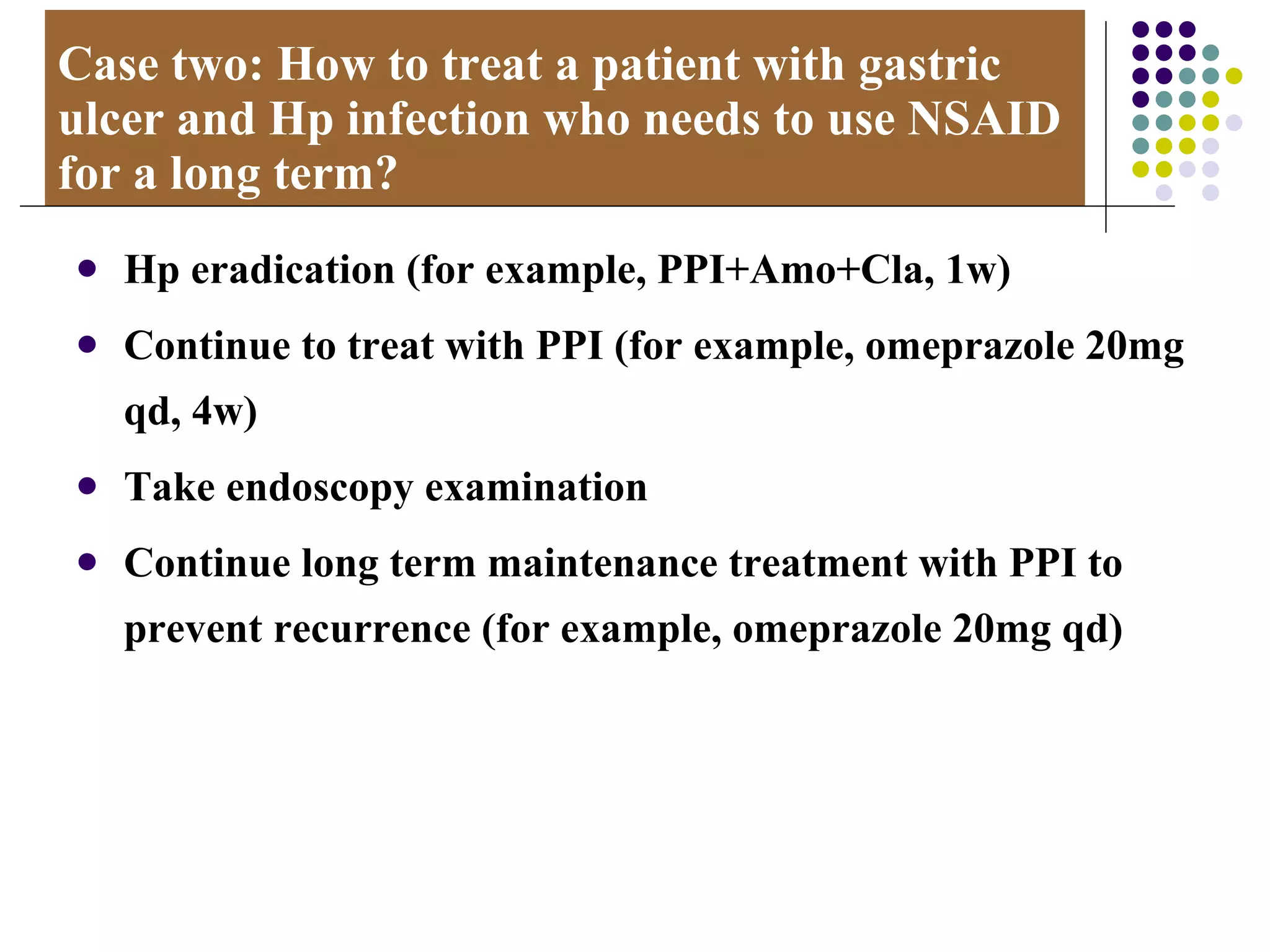
Peptic ulcer disease is caused by Helicobacter pylori (Hp) infection and nonsteroidal anti-inflammatory drug (NSAID) use. Definitive diagnosis is by endoscopy, which can detect ulcers and test for Hp. Common complications are bleeding, perforation, and pyloric obstruction. Treatment involves eradicating Hp, relieving symptoms with anti-ulcer drugs, and preventing recurrence with long-term proton pump inhibitor use.