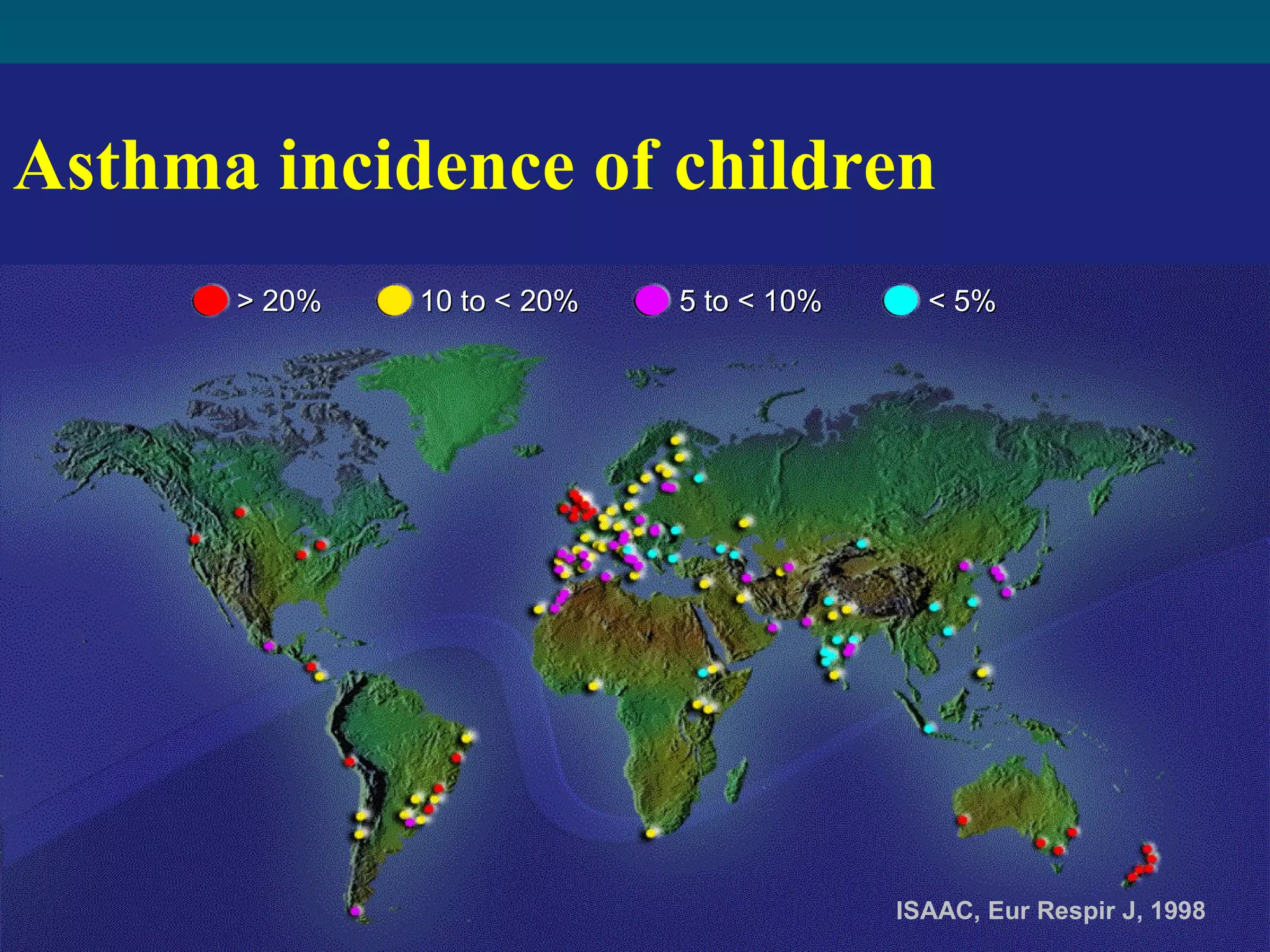
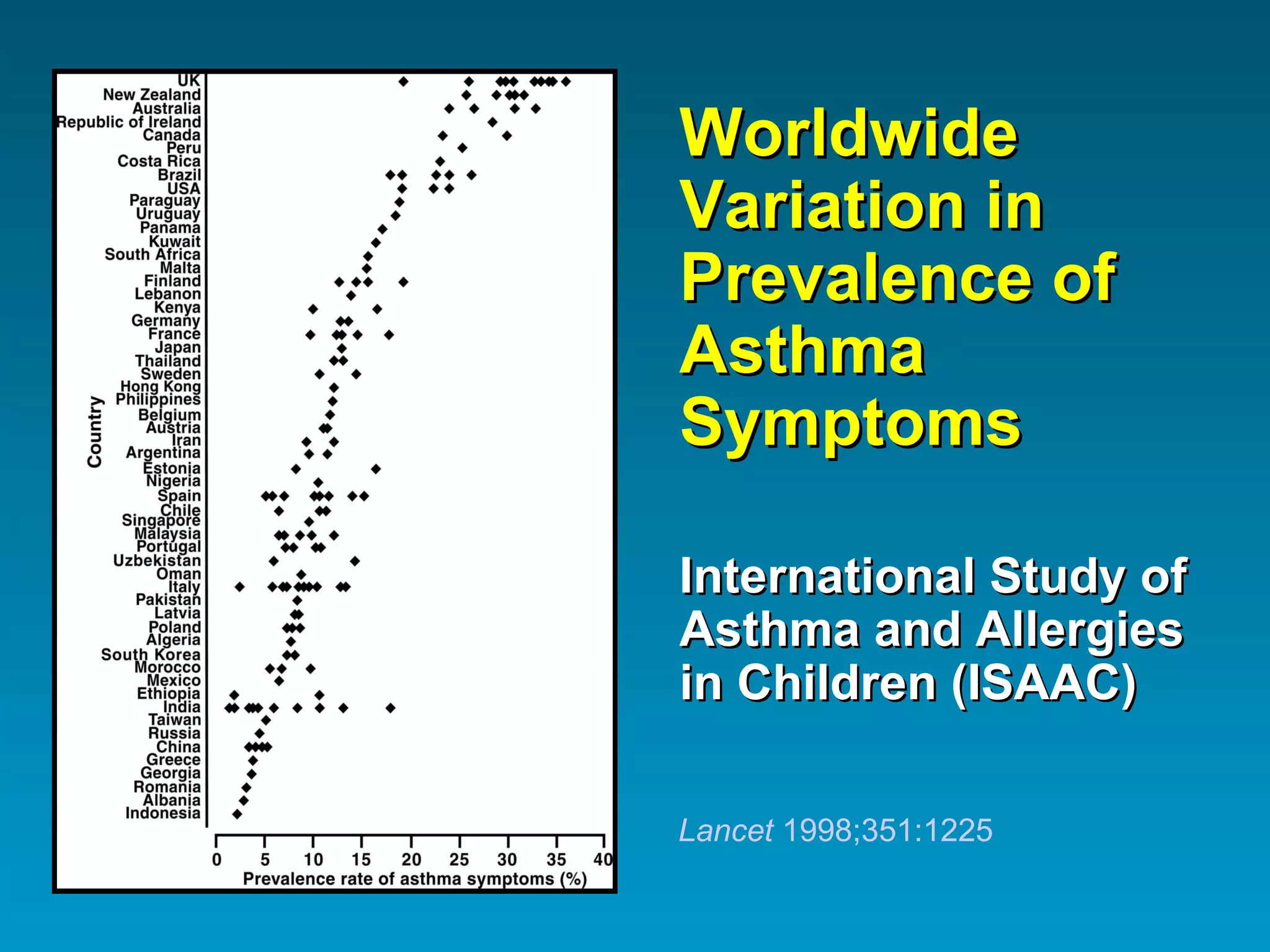
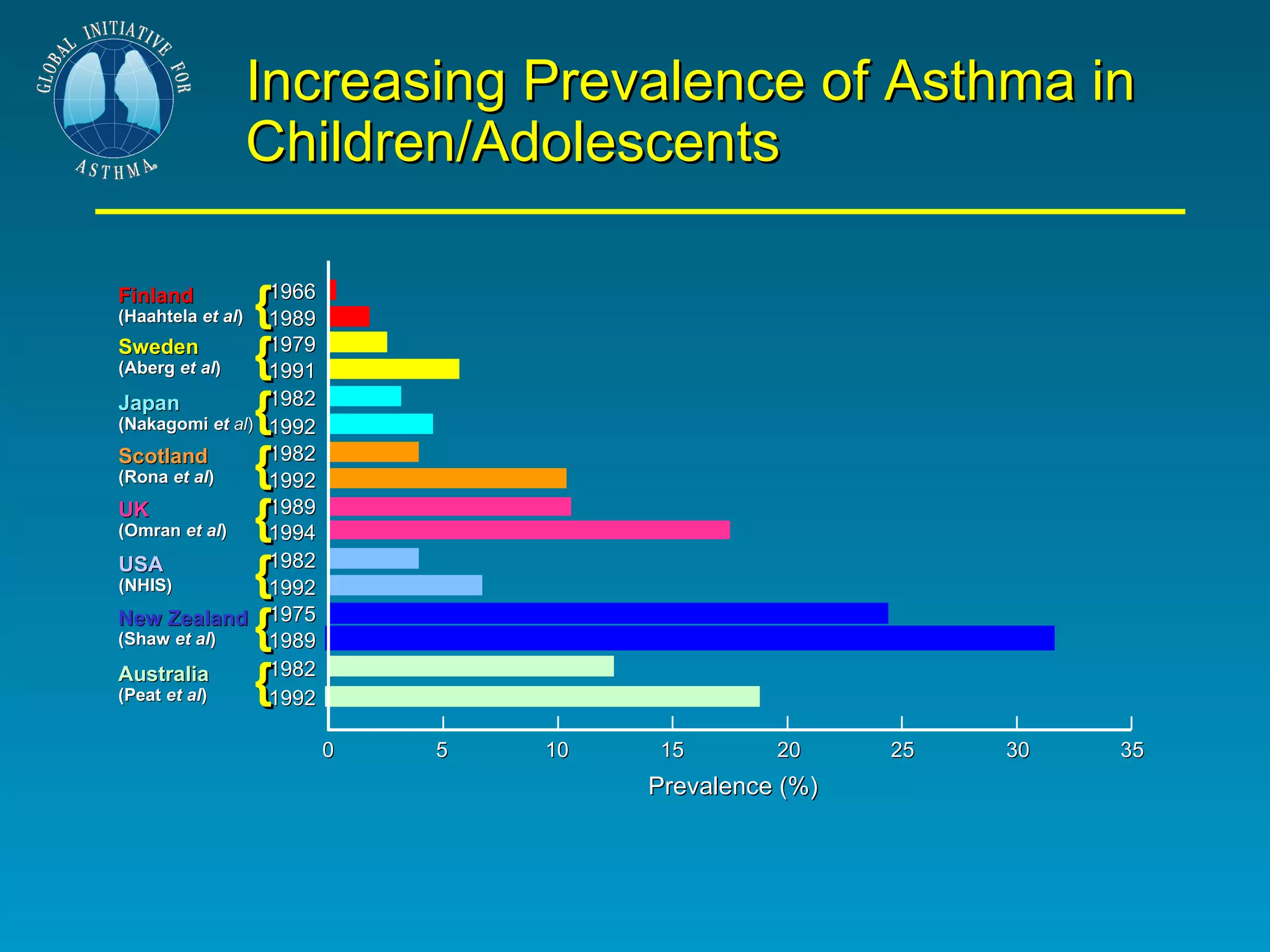
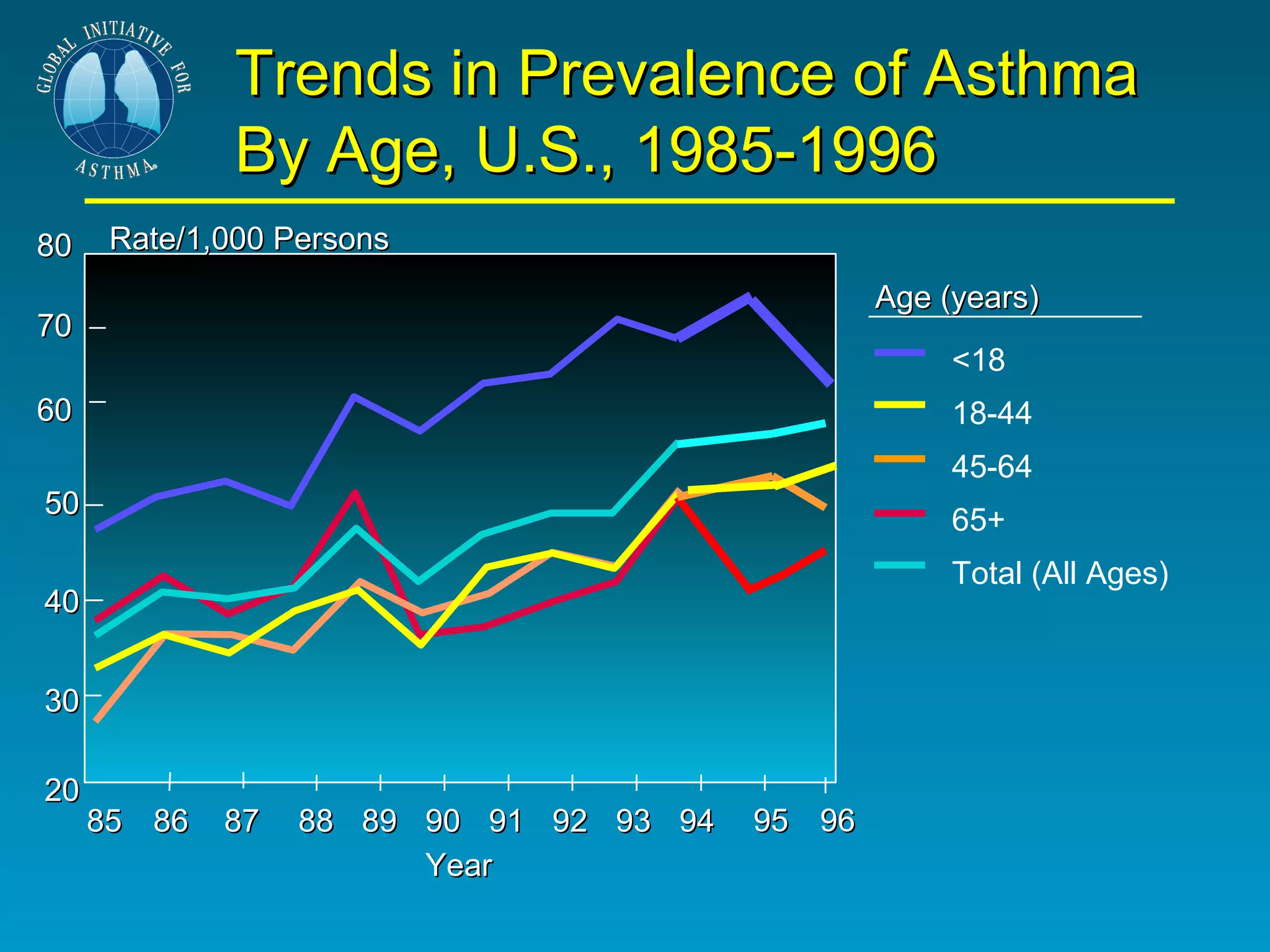
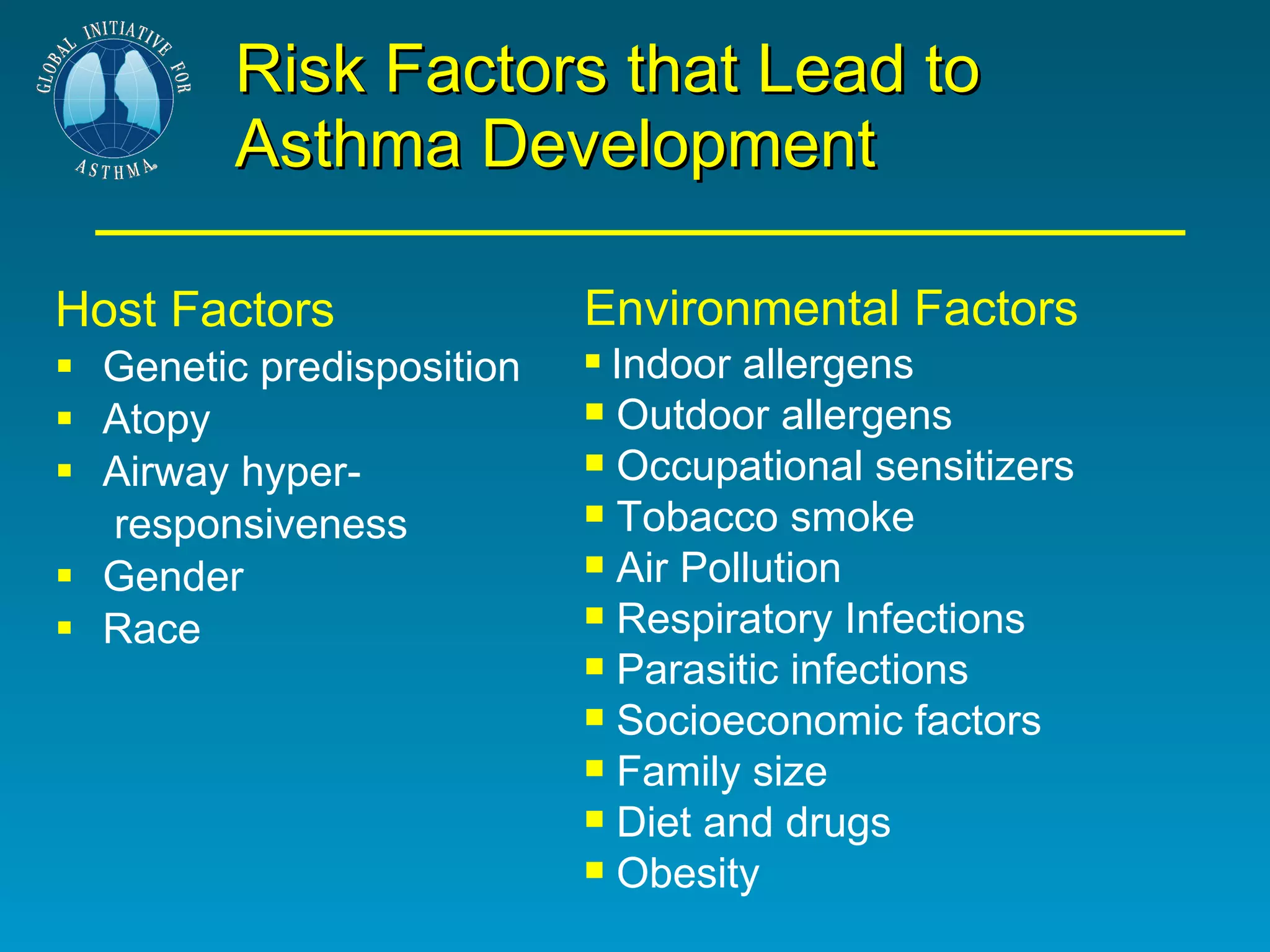
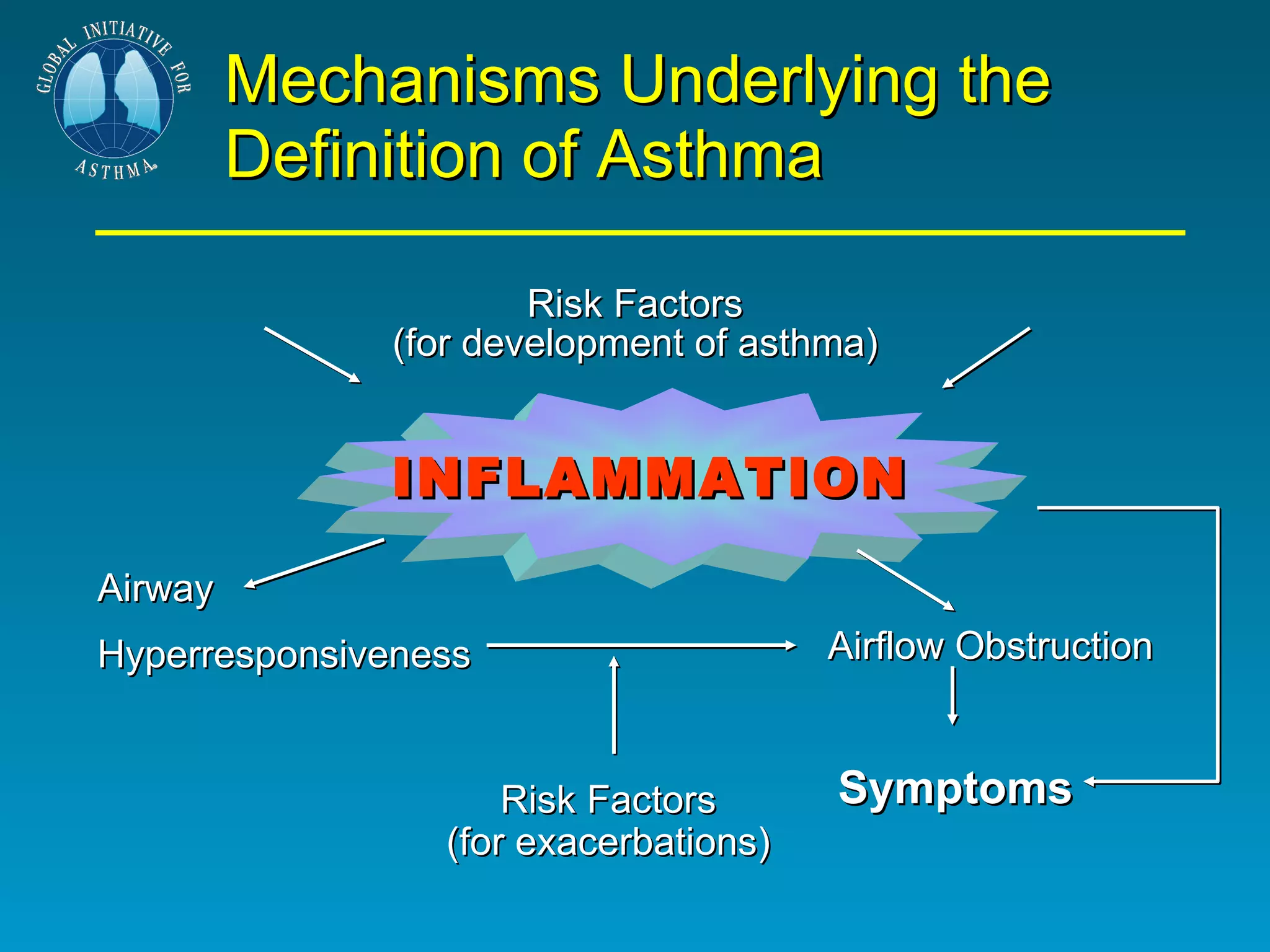
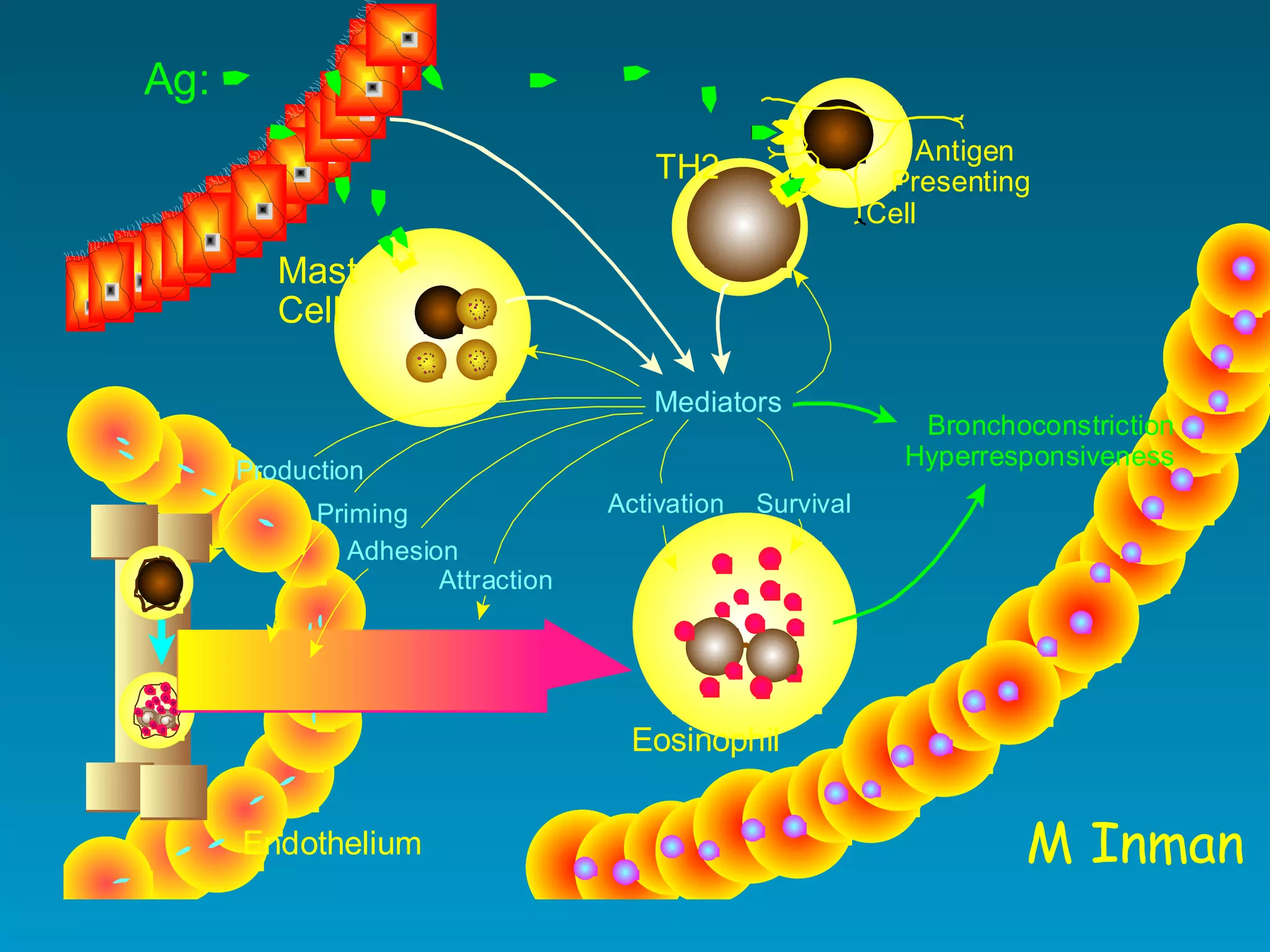
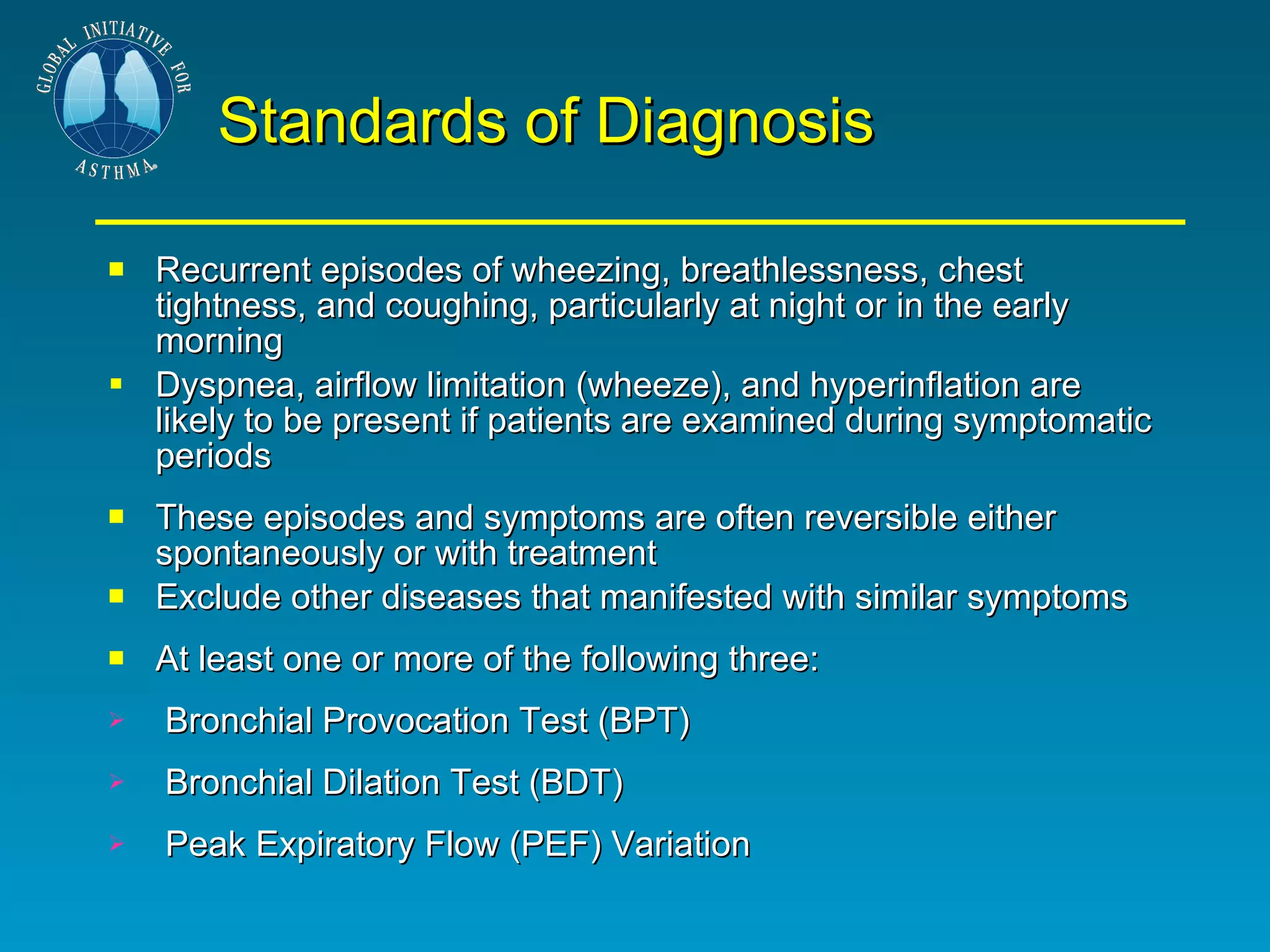
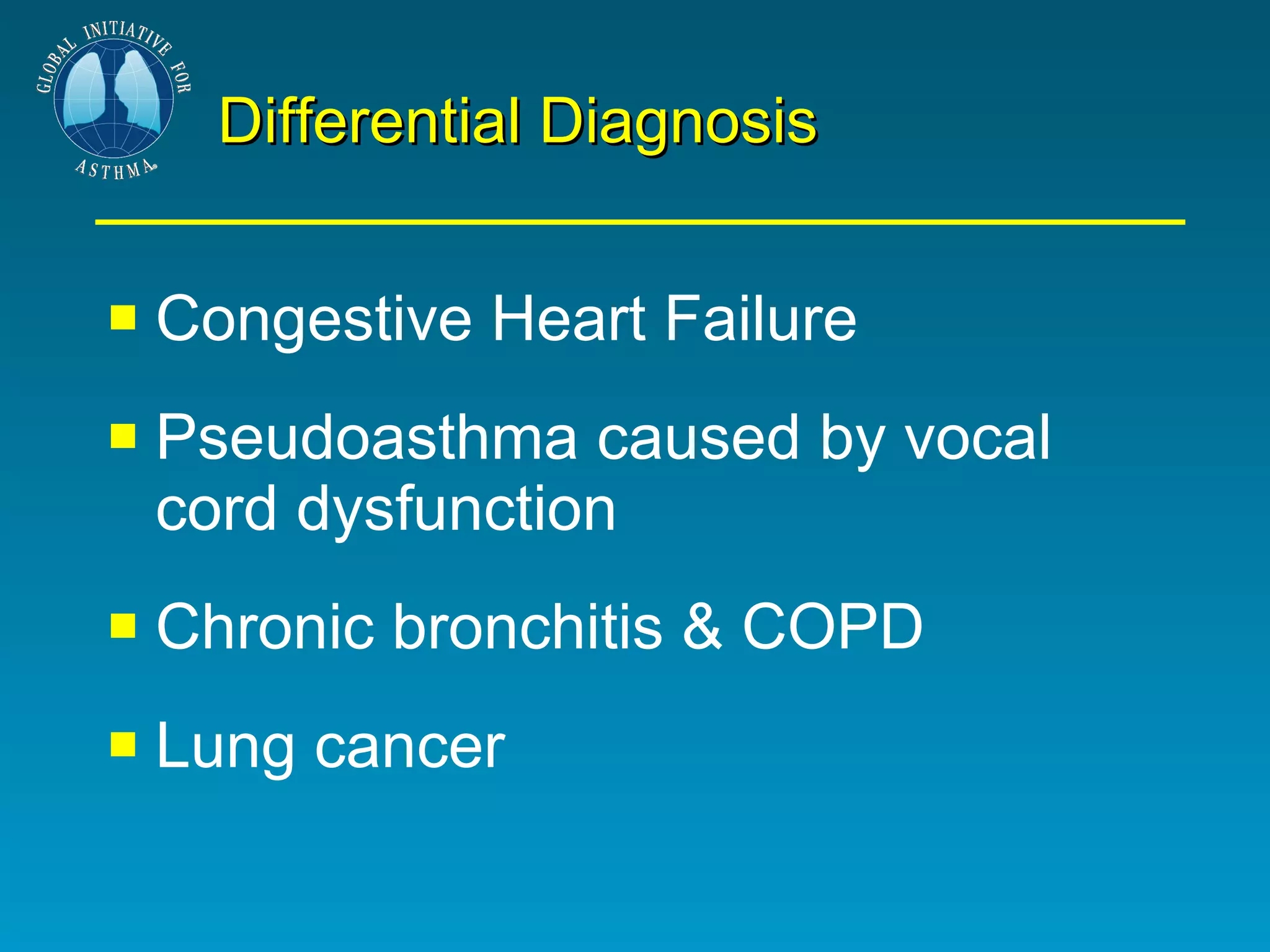
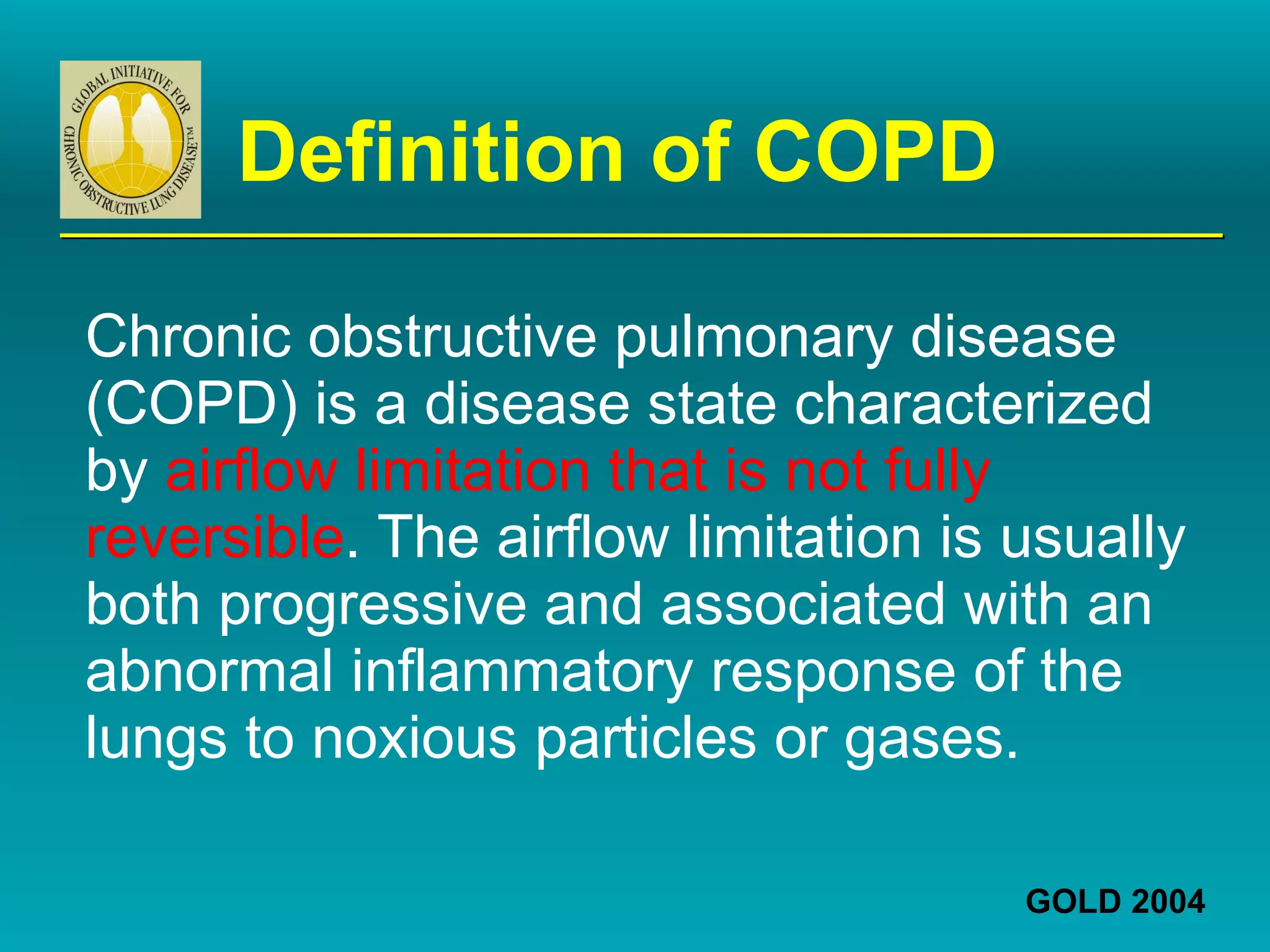
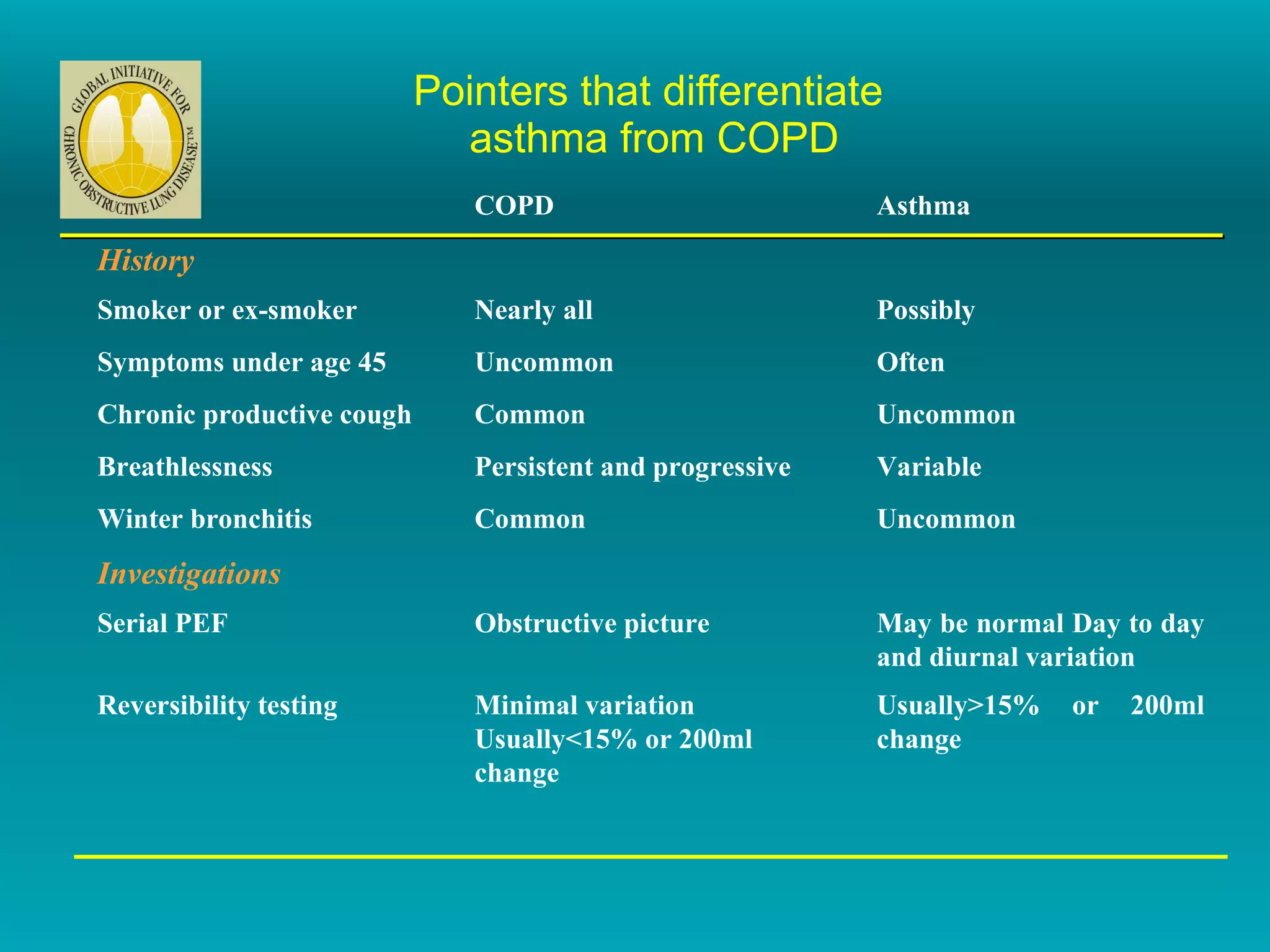
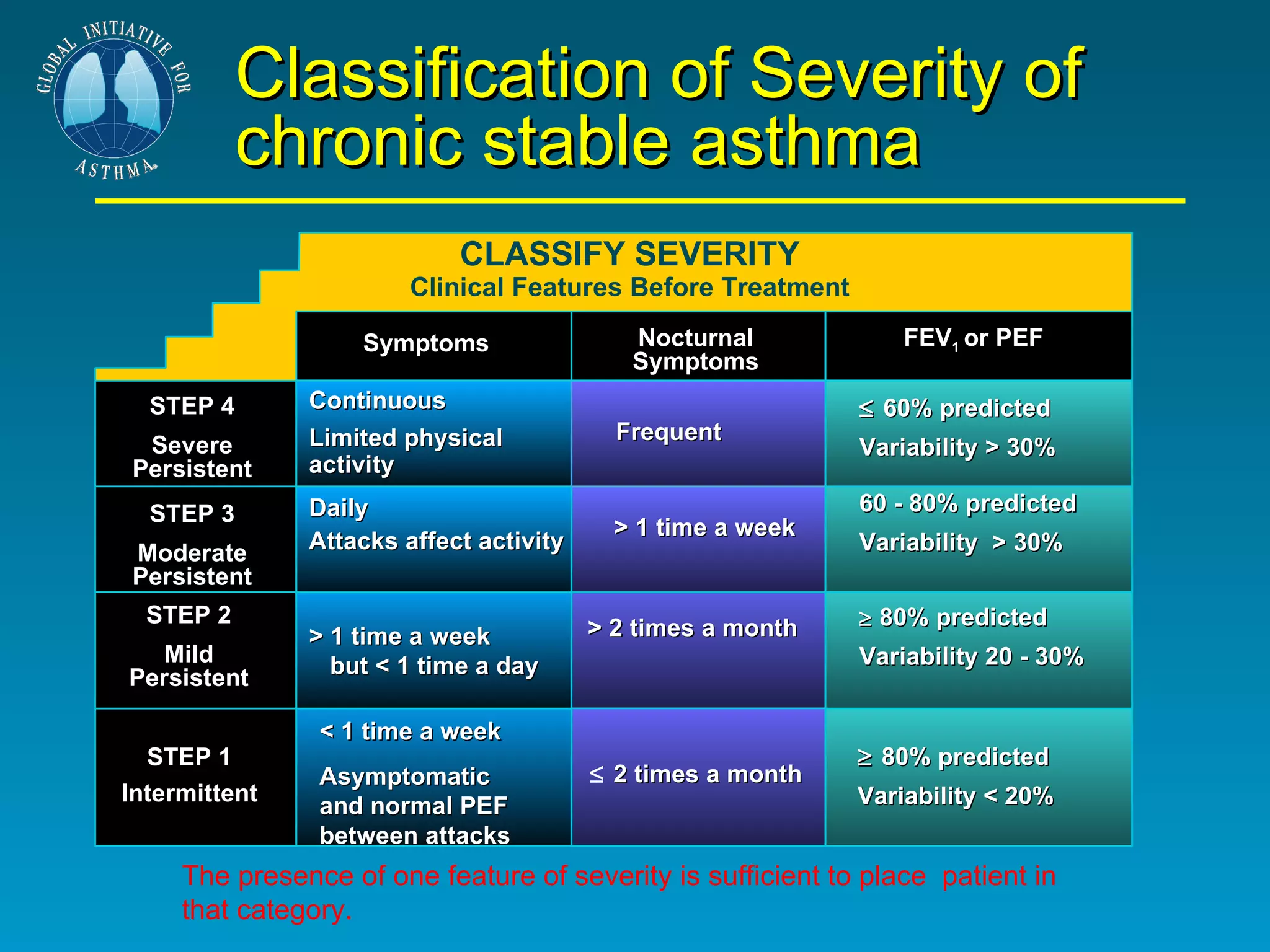
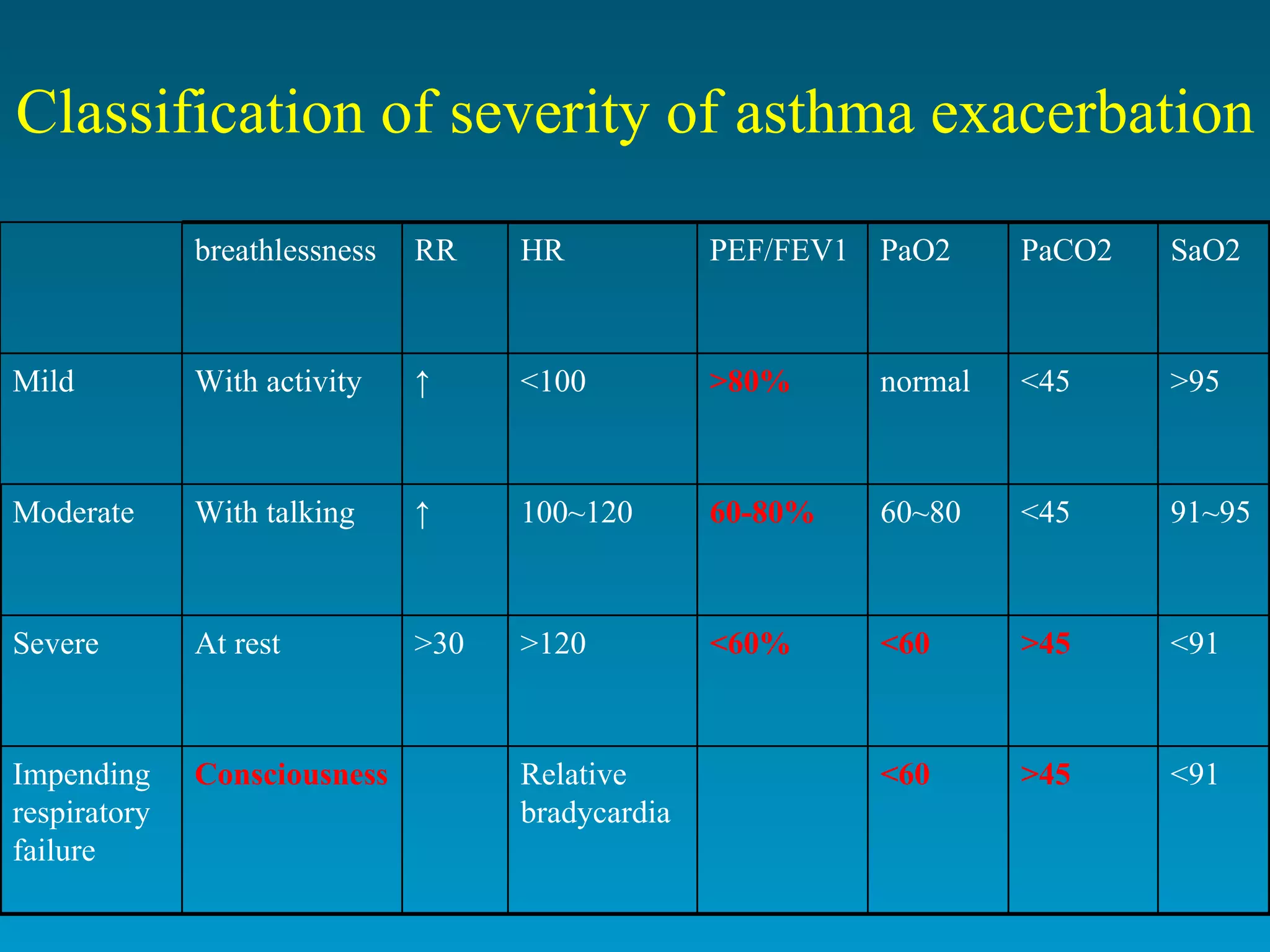
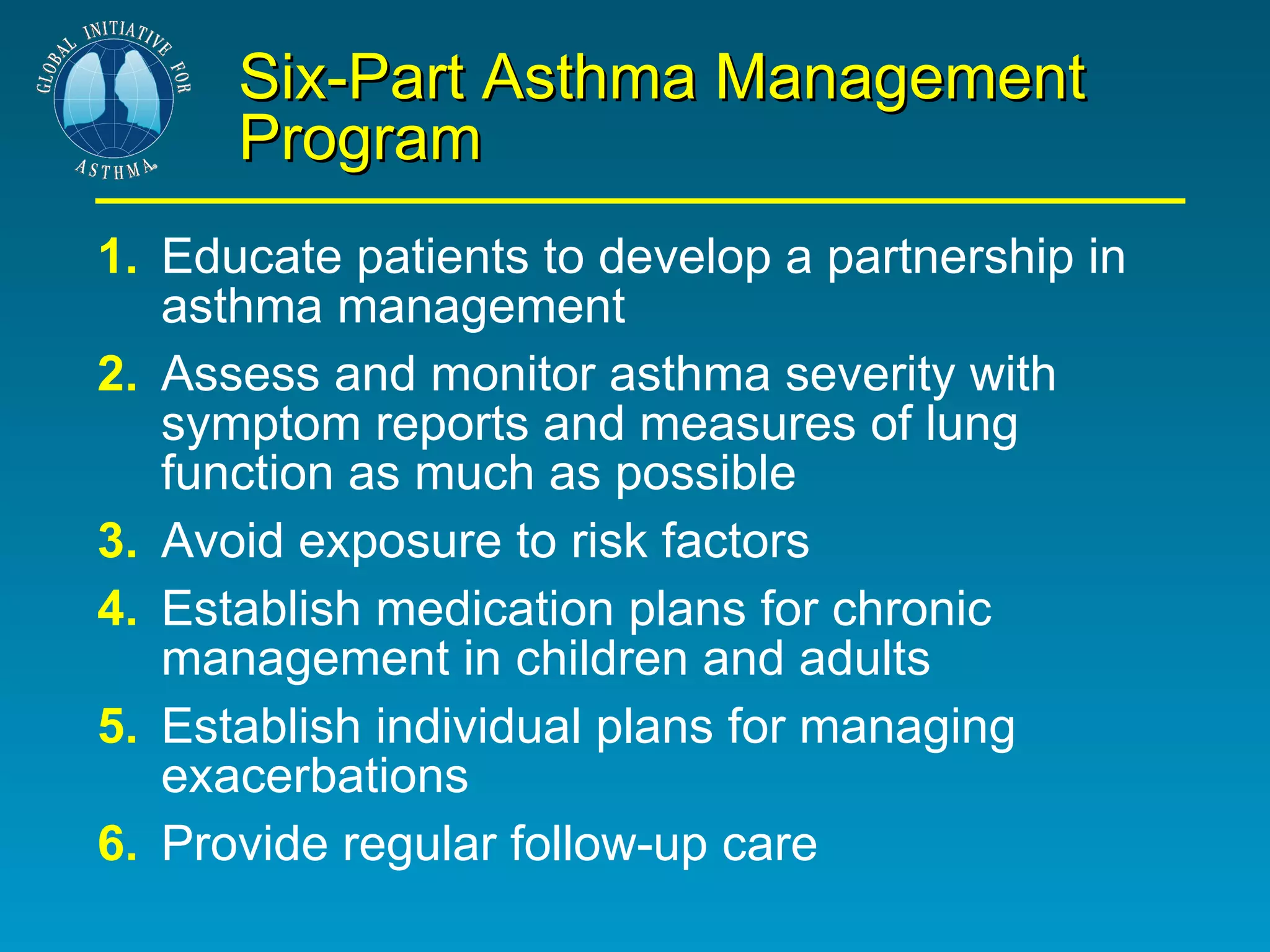
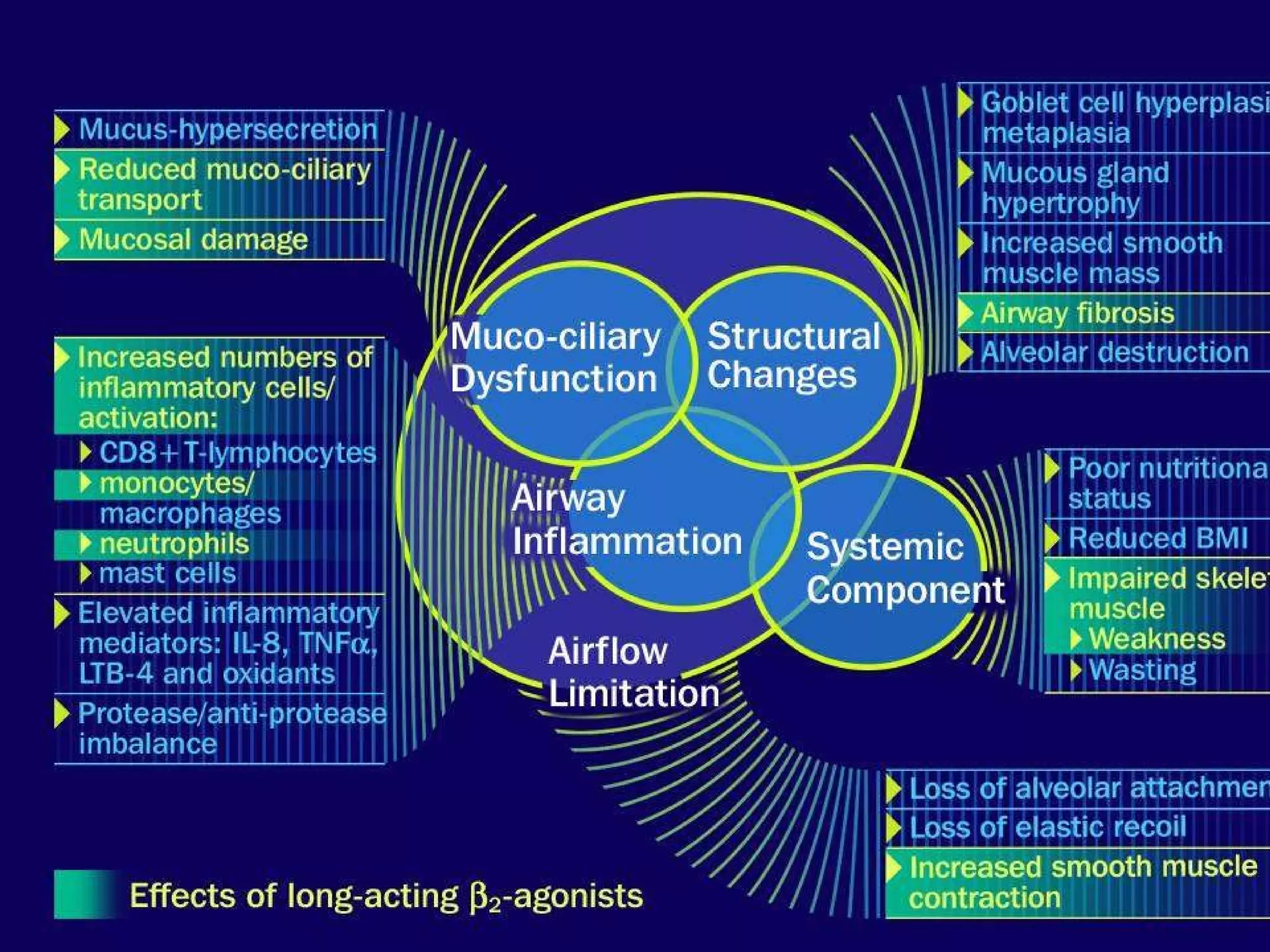
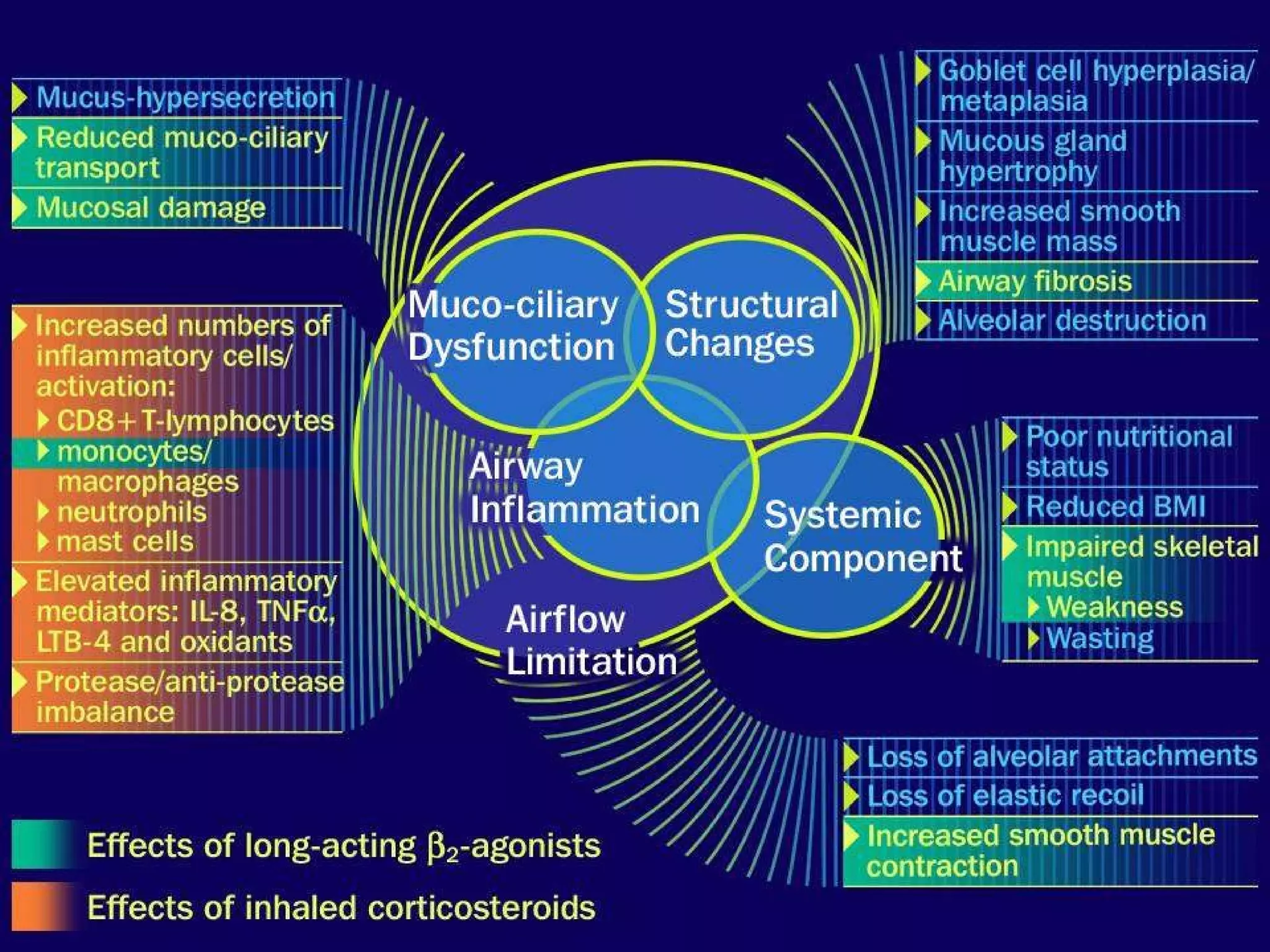
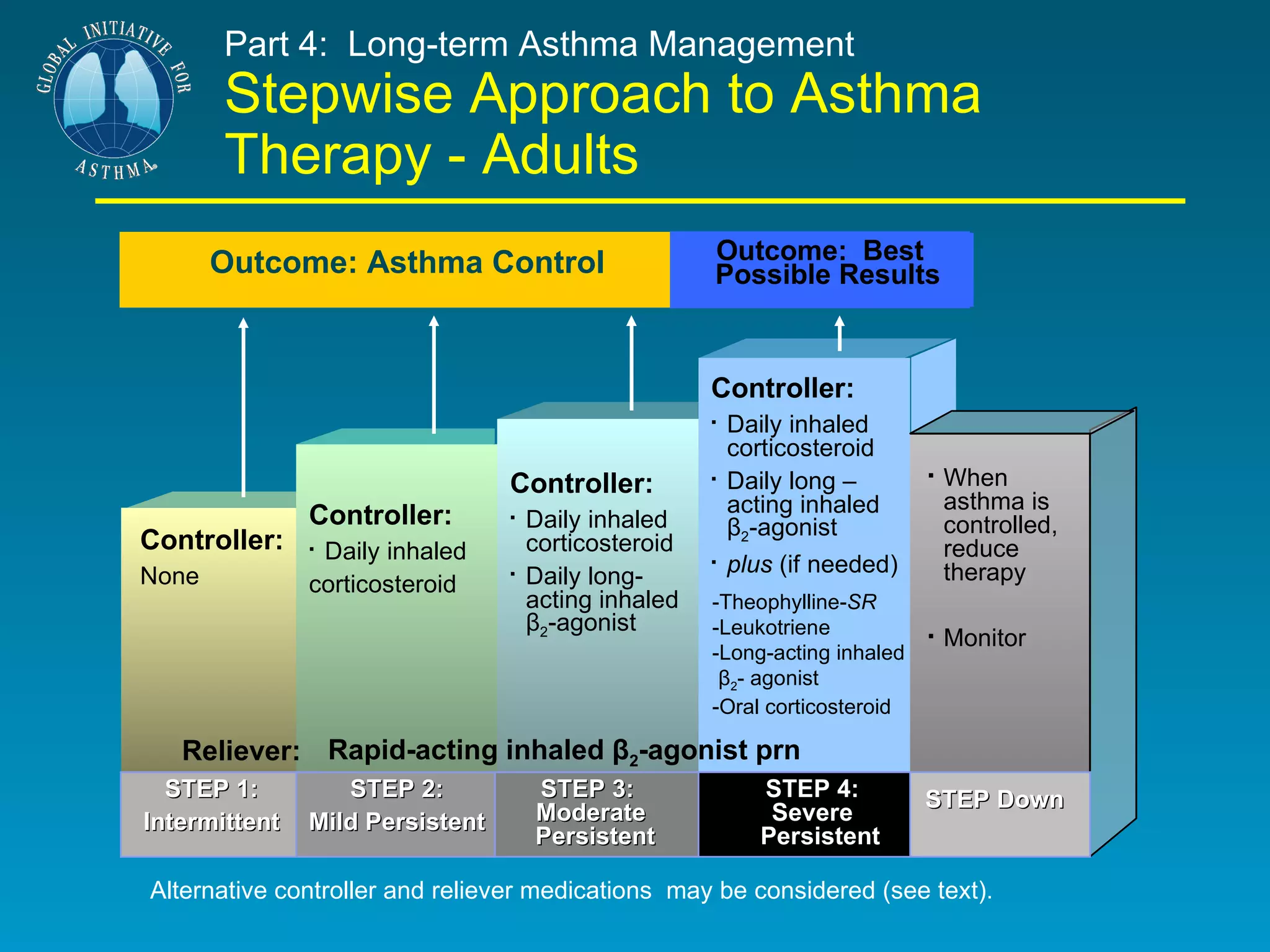
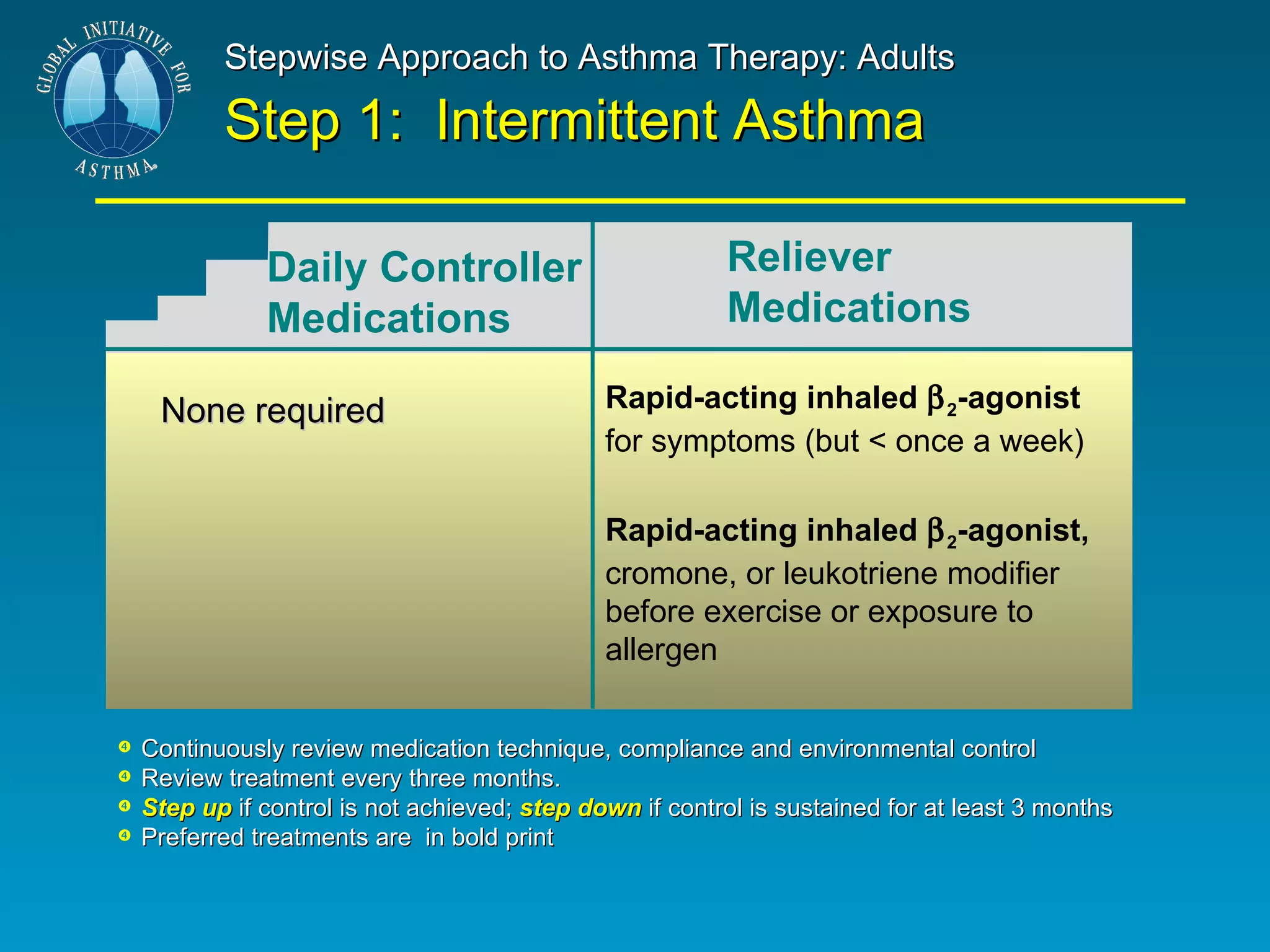
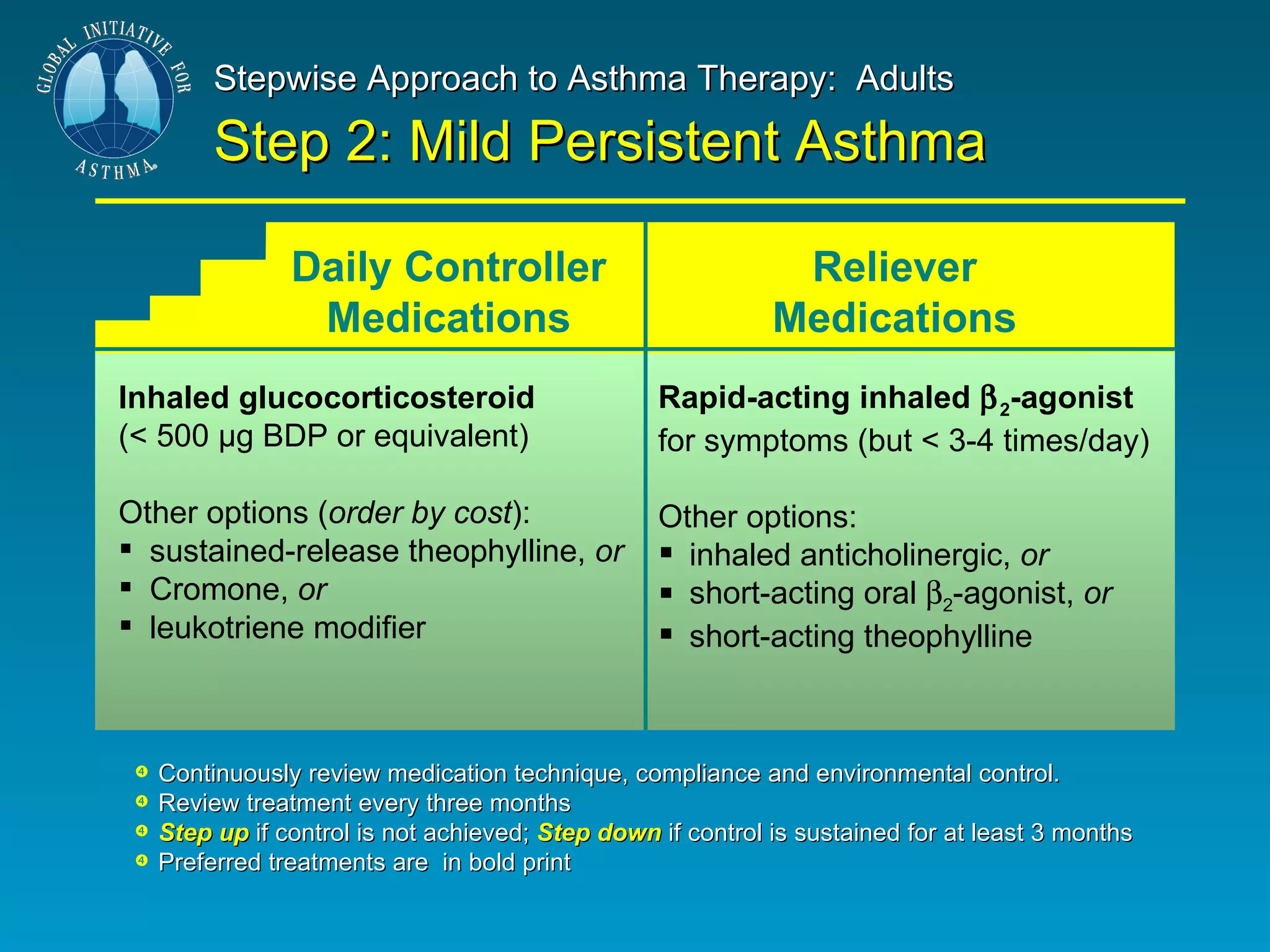
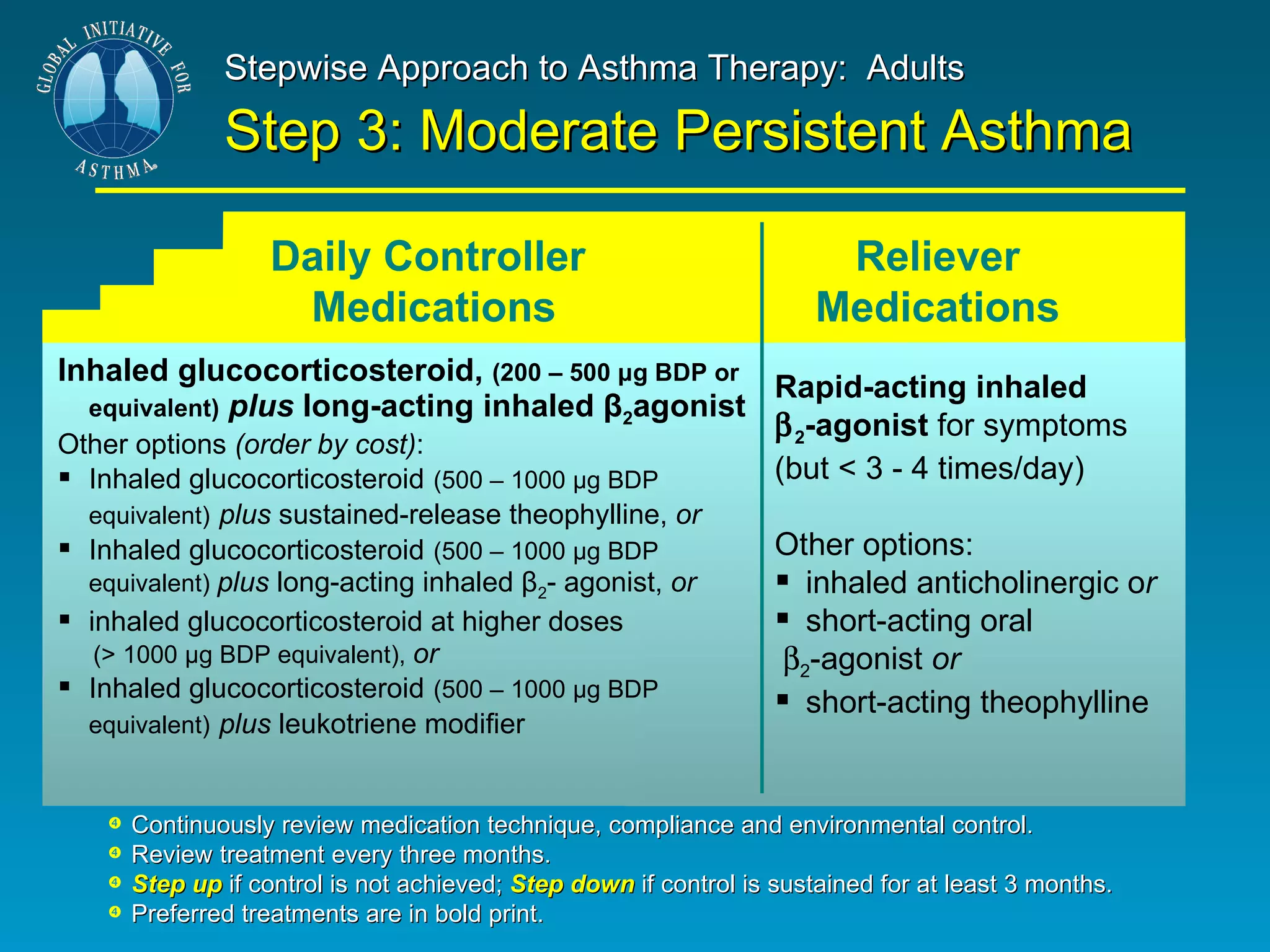
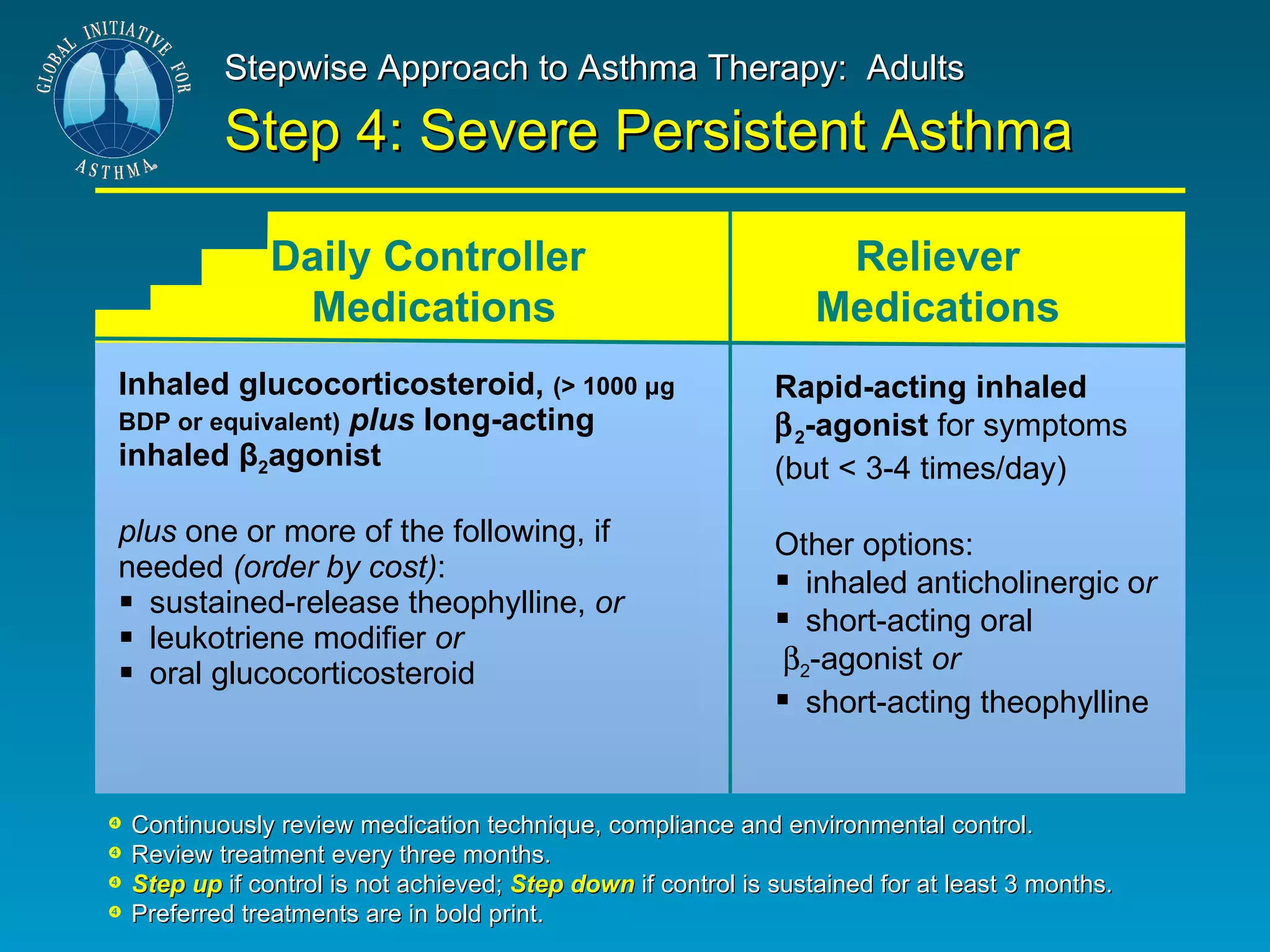
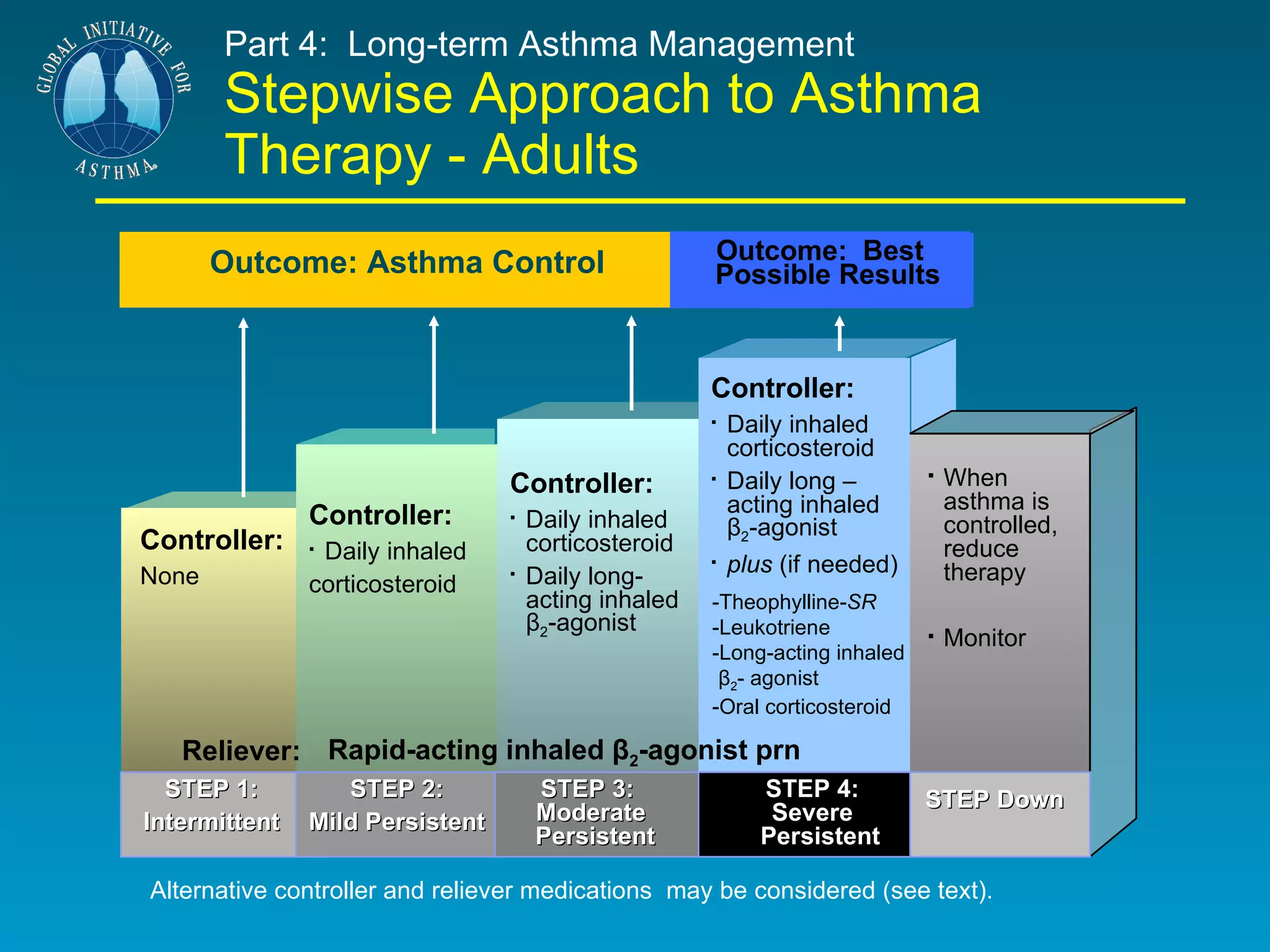
The document discusses asthma, including its definition, epidemiology, risk factors, pathogenesis, diagnosis, classification, and management. It provides details on defining asthma as a chronic inflammatory airway disease characterized by variable airflow obstruction and hyperresponsiveness. Key points include that asthma is increasing worldwide, especially in children, and its severity varies depending on symptoms, lung function measurements, and medication needs. A six-part management plan is outlined focusing on education, monitoring, avoiding triggers, long-term medication plans, managing exacerbations, and follow-up care.