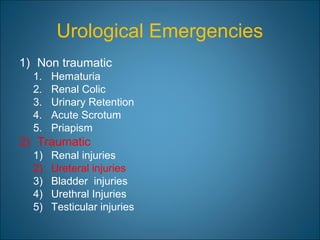
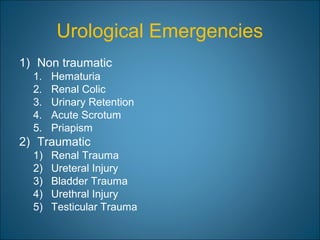
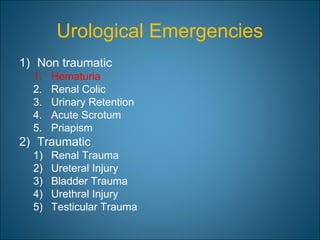
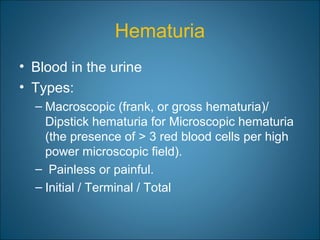
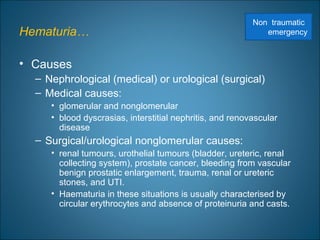
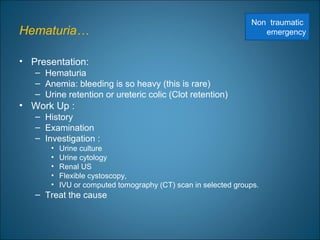
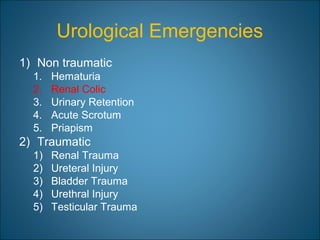
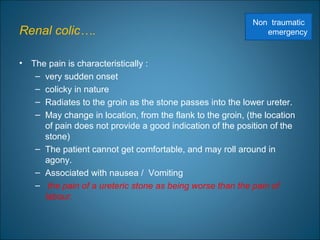
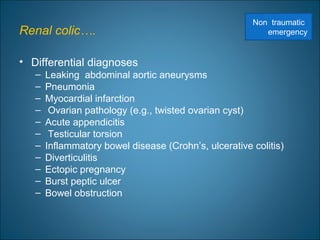
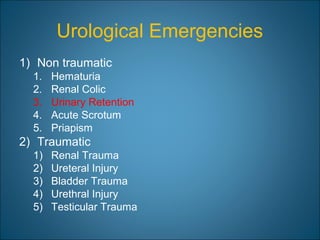
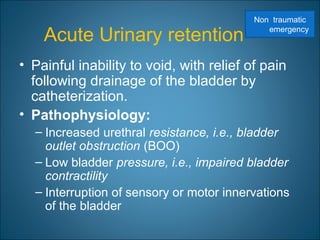
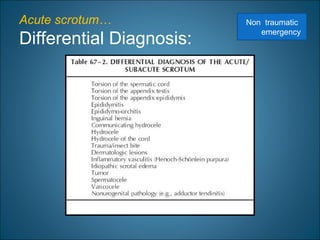
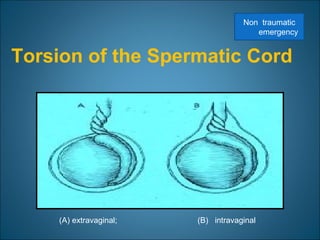
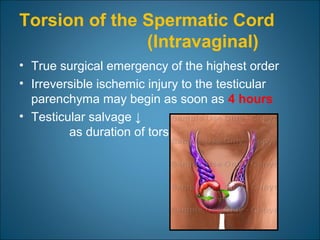
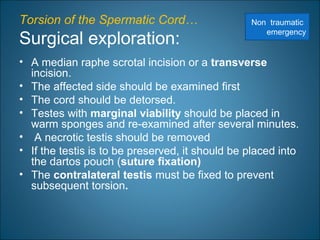
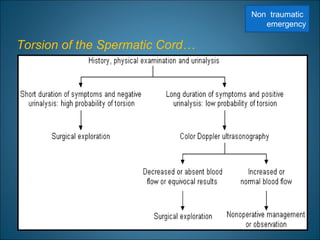
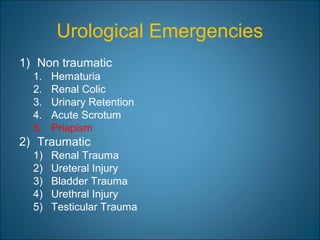
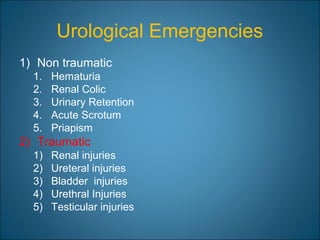
This document discusses genitourinary emergencies. It identifies the main non-traumatic emergencies as hematuria, renal colic, urinary retention, acute scrotum, and priapism. For each emergency, it describes the causes, presentations, differential diagnoses, and treatment approaches. In particular, it provides detailed information on the evaluation and management of testicular torsion, which is considered a true surgical emergency requiring prompt diagnosis and potential exploration to salvage the testis.

![Renal injuries…
• Indications for renal imaging:
– Macroscopic hematuria
– Penetrating chest, flank, and abdominal wounds
– Microscopic [>5 red blood cells (RBCs) per high
powered field] or dipstick hematuria a
hypotensive patient (SBP <90mmHg )
– A history of a rapid acceleration or deceleration
– Any child with microscopic or dipstick hematuria
who has sustained trauma.
Traumatic
emergency](https://image.slidesharecdn.com/3urologicalemergency-130625140801-phpapp02/85/3-urological-emergency-52-320.jpg)