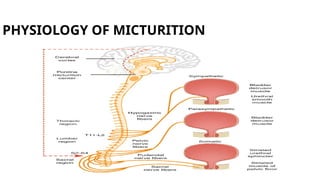
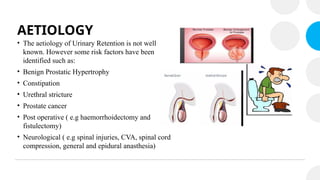
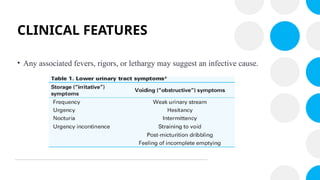
The document discusses acute urinary retention (AUR), defined as a sudden inability to urinate despite normal urine production. It covers the classification, anatomy, physiology, epidemiology, risk factors, clinical features, diagnostic methods, management strategies, and potential complications associated with AUR. Management primarily involves urethral catheterization, and surgical interventions may be needed for recurrent cases or underlying causes.