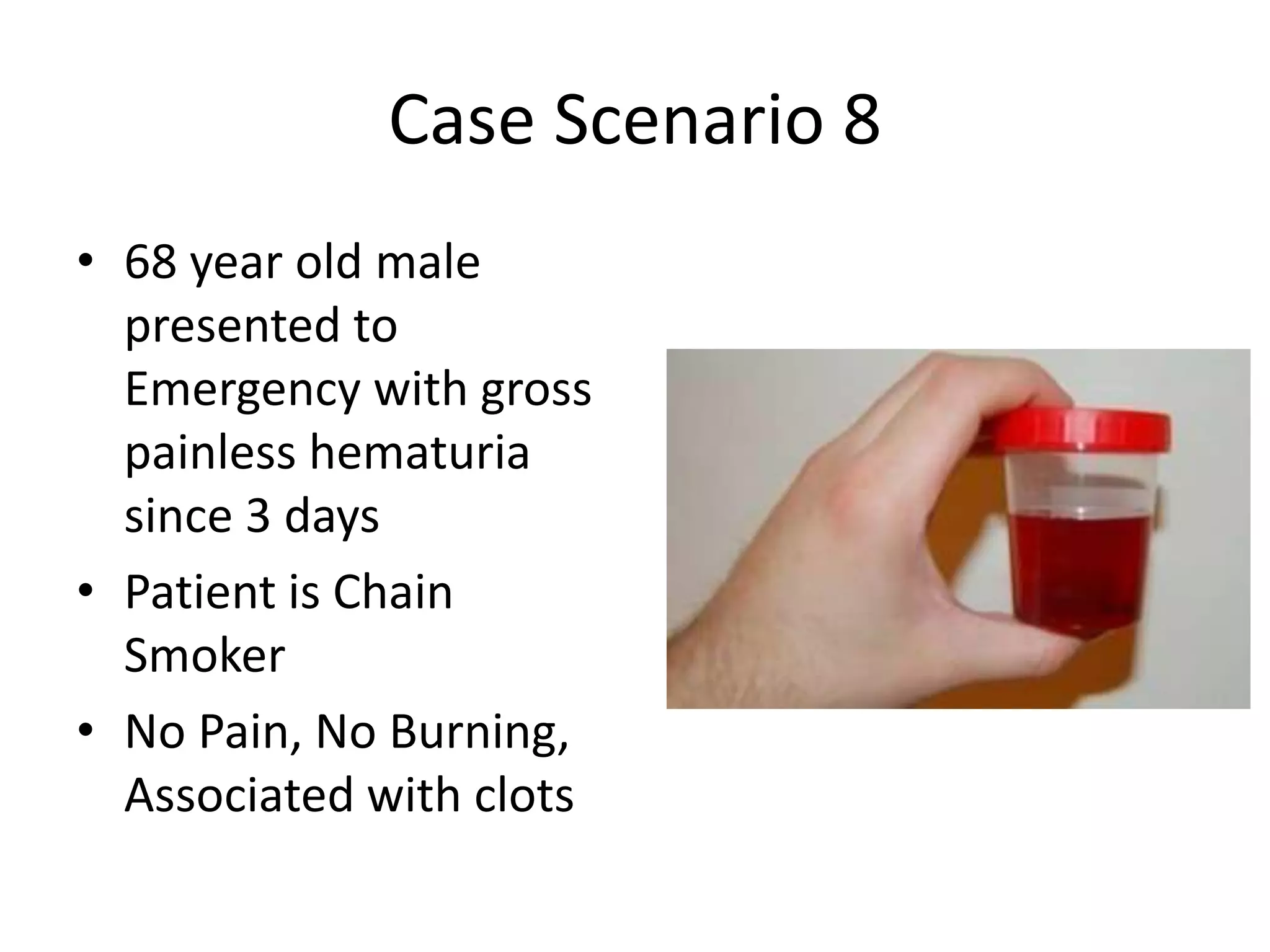
The document discusses various acute emergencies in urology, detailing conditions like acute and chronic urinary retention, acute urinary tract infections, renal stones, and hematuria through case scenarios. It emphasizes management protocols, differential diagnoses, examination techniques, and the necessity of investigations such as ultrasounds and CT scans. The document also outlines specific treatment strategies, including catheterization, pain relief measures, antibiotic use, and when to consider surgical interventions.