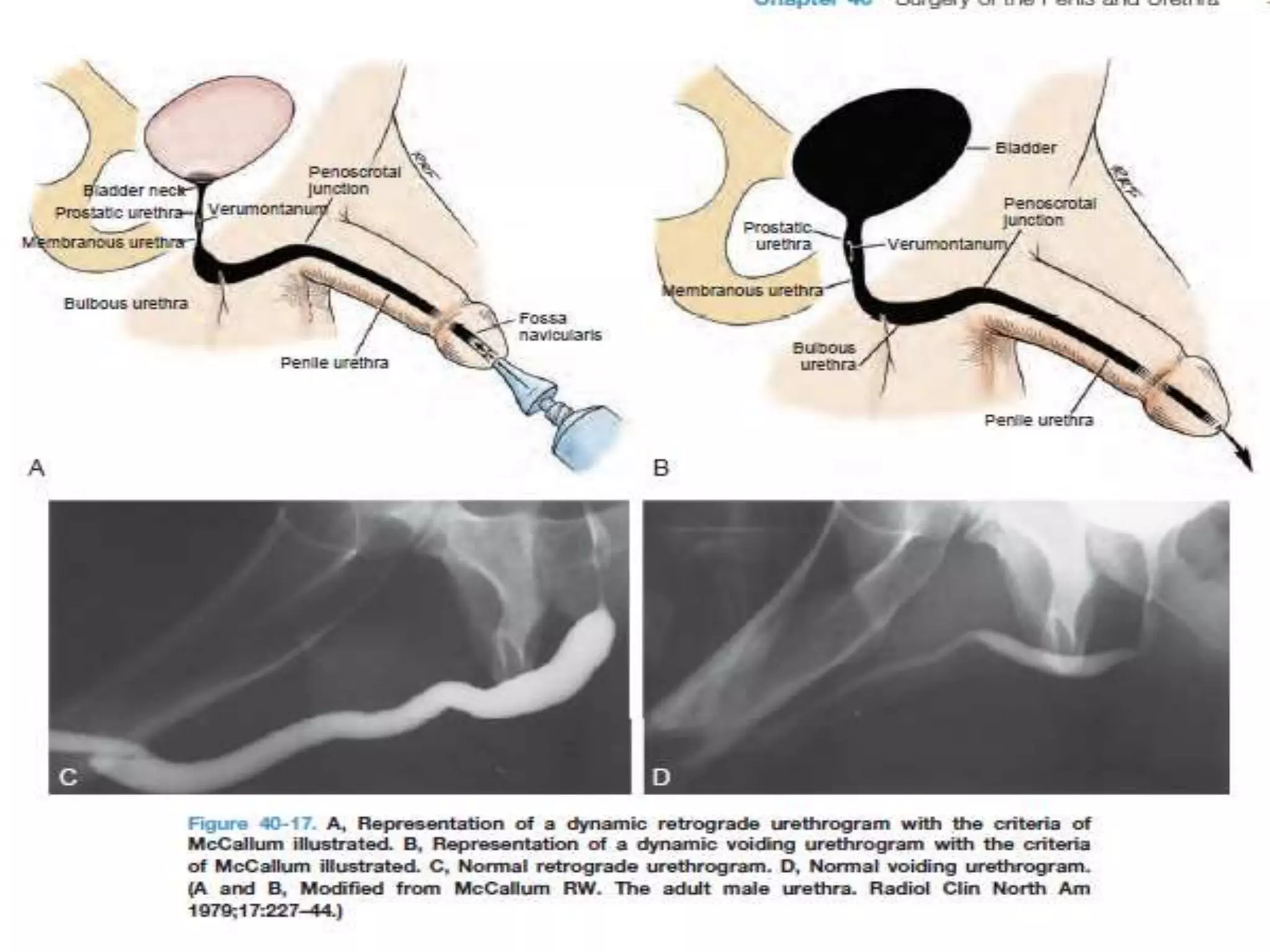
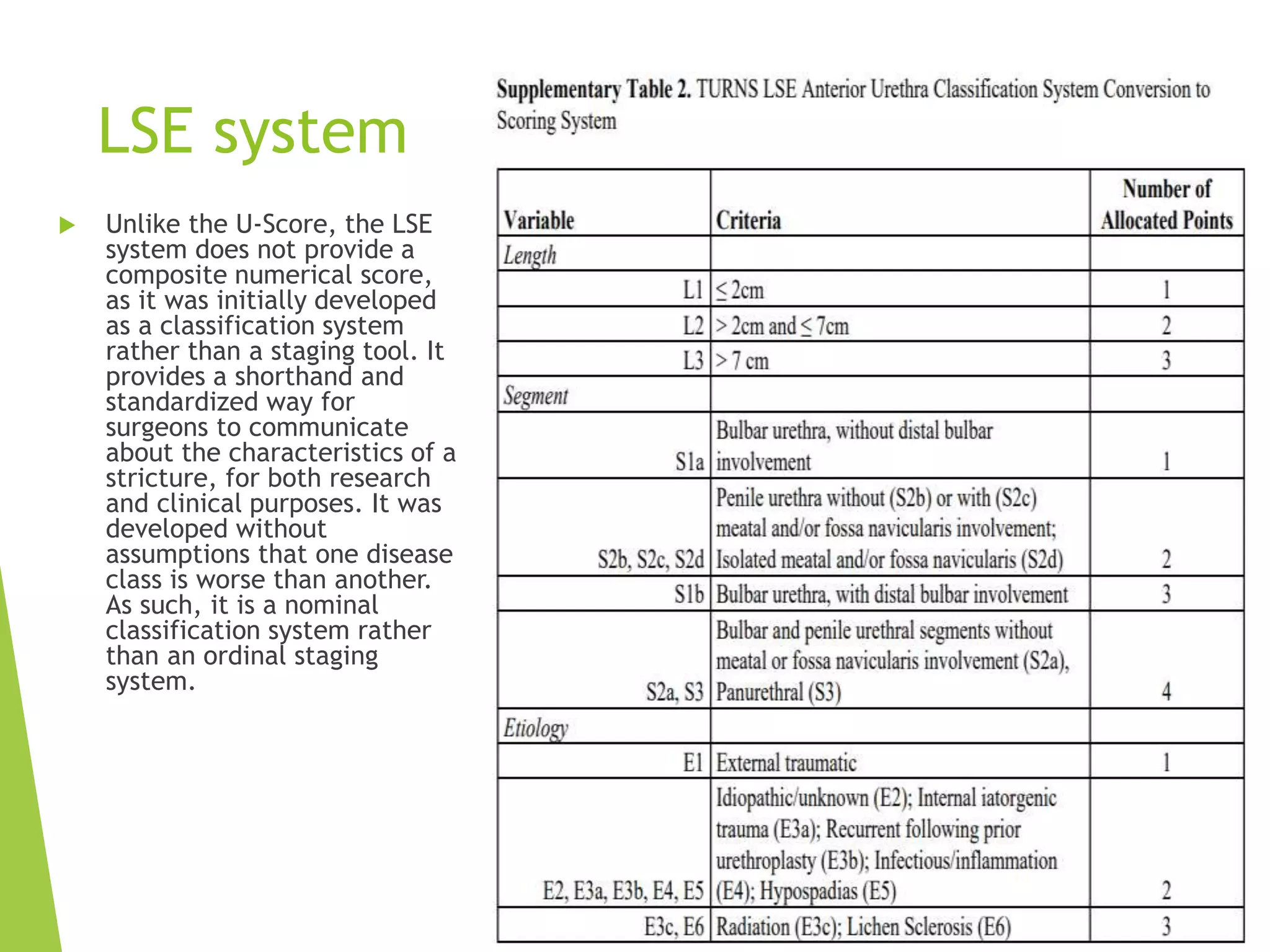
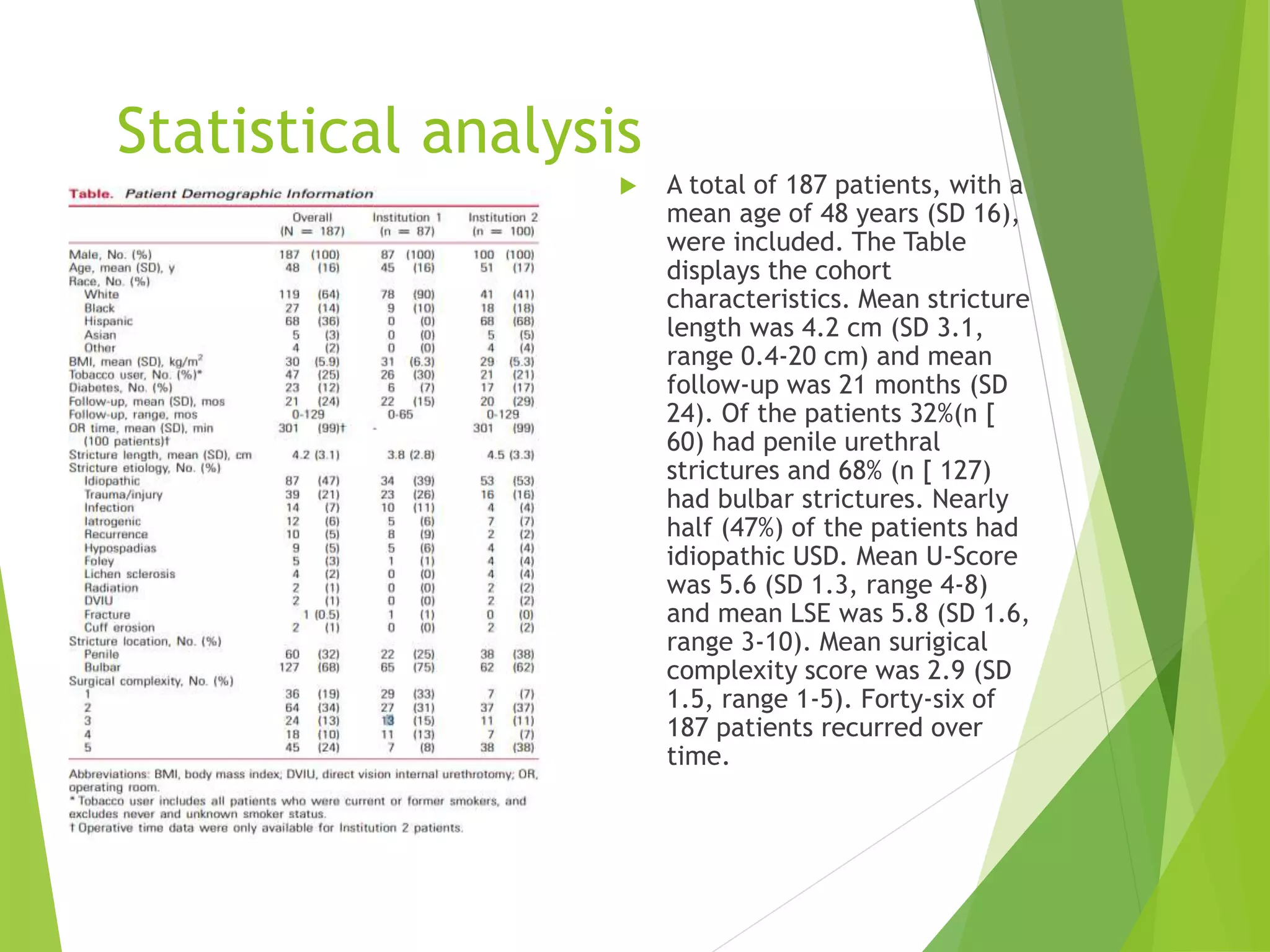
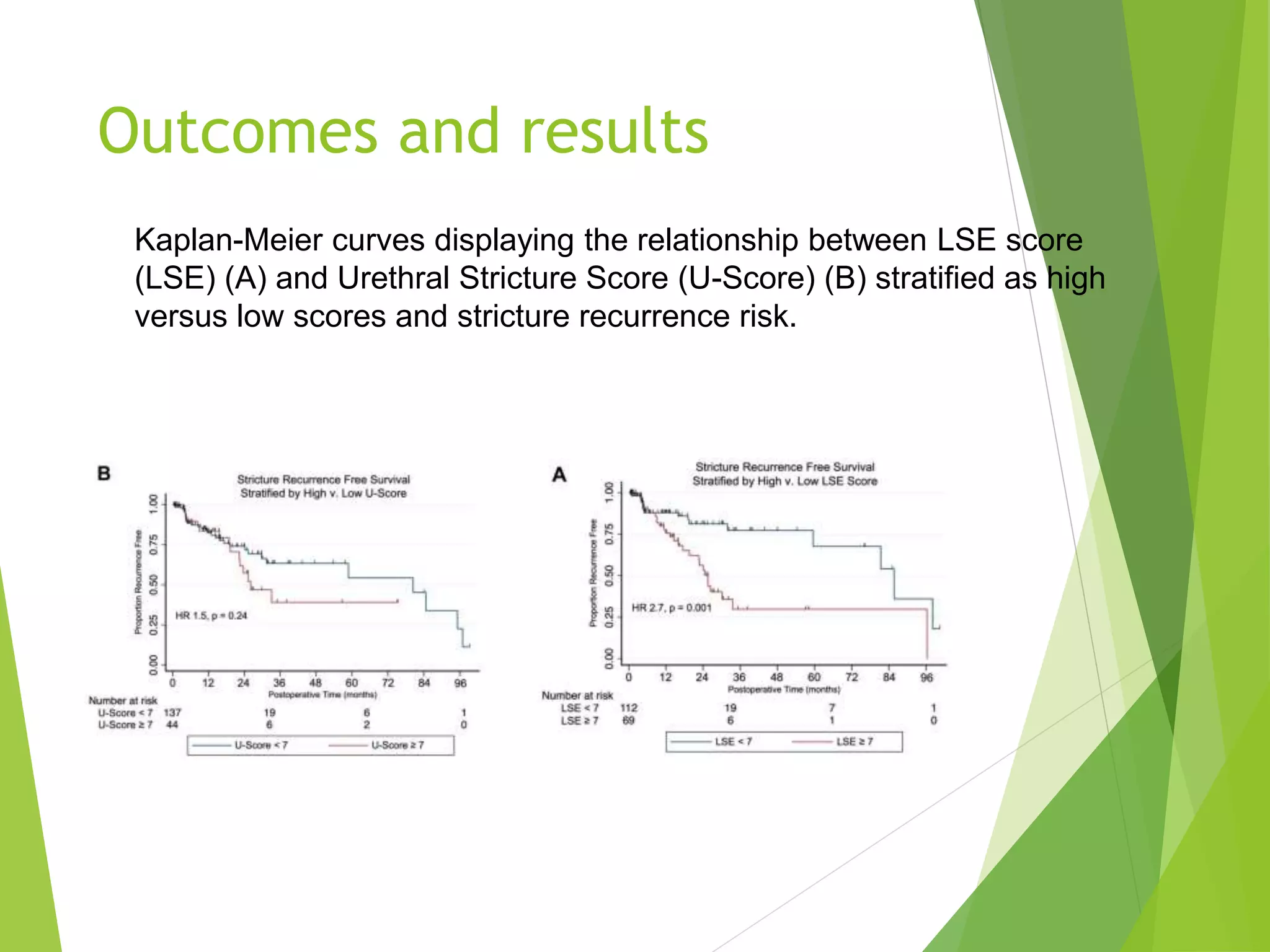
The document discusses urethral stricture, its anatomy, etiology, pathogenesis, clinical features, and treatment options. It also evaluates scoring systems (u-score and lse) used for characterizing stricture severity in a study conducted at Columbia University, highlighting their association with surgical complexity and recurrence risk. The findings indicate that while both scoring systems correlate with surgical complexity, only the lse score is significantly linked to stricture recurrence risk.