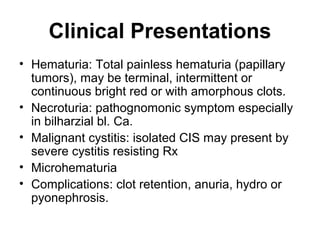
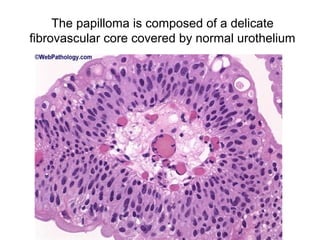
1. Bladder tumors can be epithelial like papillomas or carcinomas, or mesenchymal like leiomyomas or sarcomas.
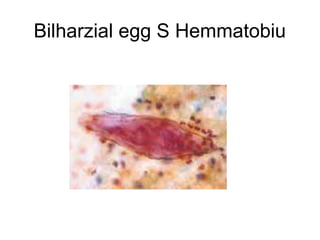
2. In Egypt, bladder cancer is most common in males, with a male to female ratio of 3:1 and peak incidence between ages 30-50 due to bilharziasis.
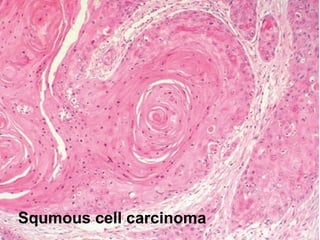
3. Bilharzial bladder carcinoma presents at a younger age, with higher male predominance and more squamous cell carcinoma histology compared to non-bilharzial bladder cancer.