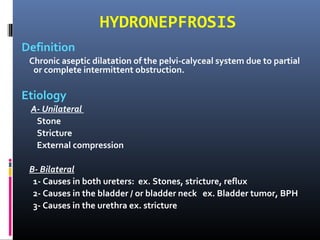
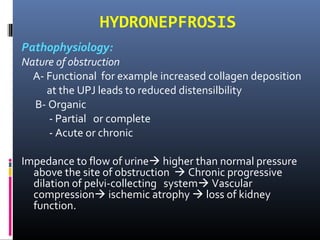
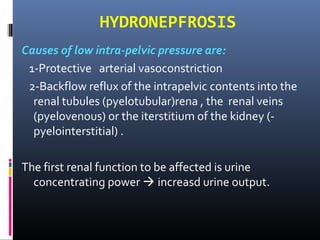
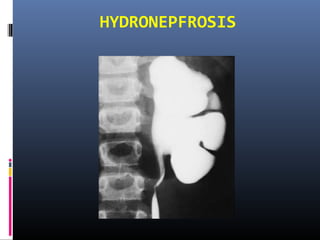
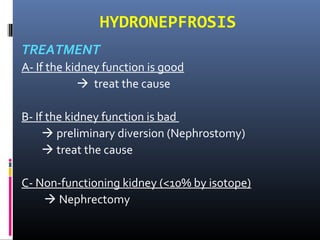
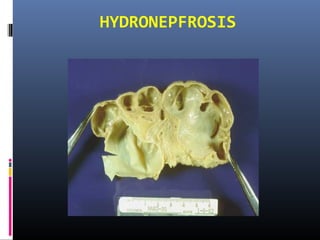
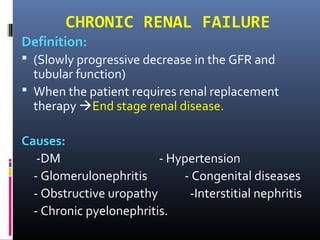
This document defines and describes hydronephrosis, which is the chronic dilatation of the pelvi-calyceal system due to partial or complete intermittent obstruction of urine flow. It discusses the etiology, pathophysiology, clinical presentation, investigations, and treatment of hydronephrosis. Treatment involves treating the underlying cause if kidney function is good or performing nephrostomy or nephrectomy if function is impaired. The role of the urologist is to rule out correctable obstructions and perform surgery for obstructive causes of chronic renal failure.