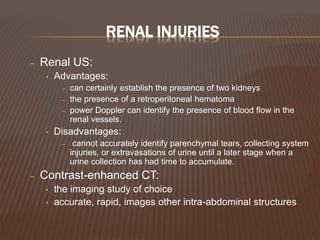
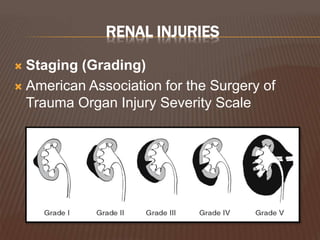
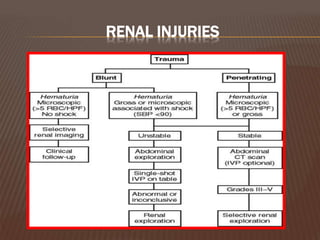
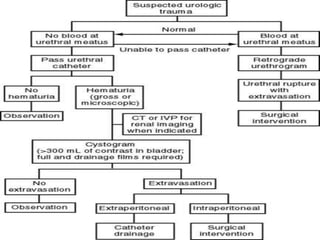
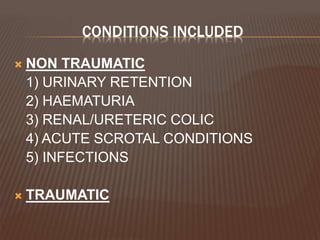
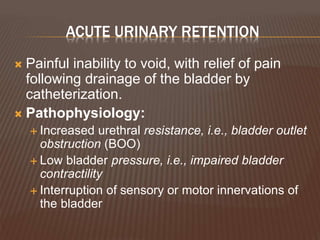
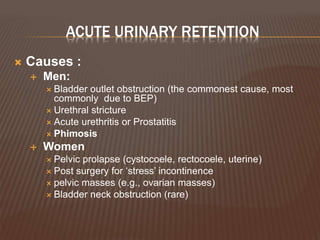
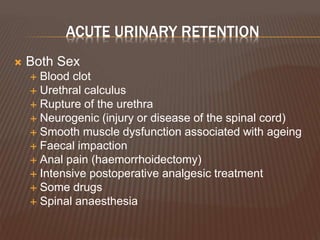
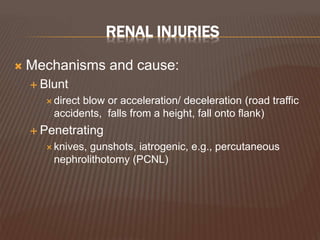
This document discusses various acute urological conditions that commonly present as emergencies. It covers non-traumatic conditions like urinary retention, hematuria, renal colic, and infections as well as traumatic injuries. For each condition, it describes the typical presentation, important distinguishing features, investigations, differential diagnoses, and initial management approach. It provides a useful overview of how to evaluate and treat many urgent urological problems.









![RENAL INJURIES
• Indications for renal imaging:
– Macroscopic hematuria
– Penetrating chest, flank, and abdominal wounds
– Microscopic [>5 red blood cells (RBCs) per high
powered field] or dipstick hematuria a
hypotensive patient (SBP <90mmHg )
– A history of a rapid acceleration or deceleration
– Any child with microscopic or dipstick hematuria
who has sustained trauma.](https://image.slidesharecdn.com/acuteurologicalconditions-130121123140-phpapp01/85/Acute-urological-conditions-36-320.jpg)