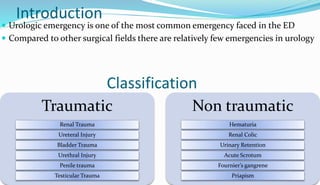
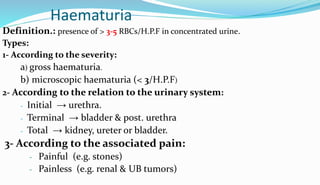
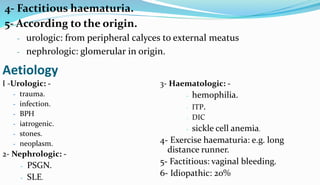
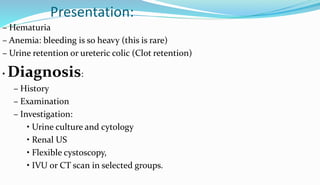
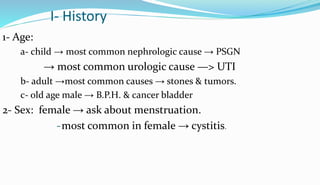
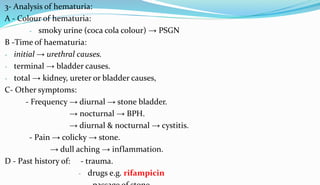
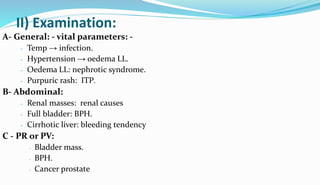
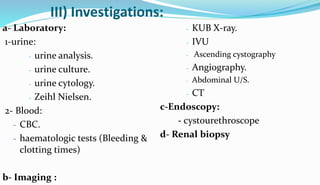
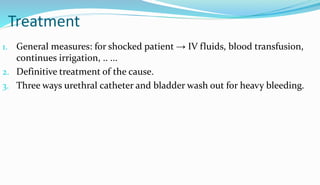
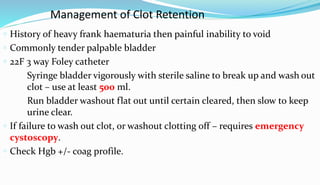
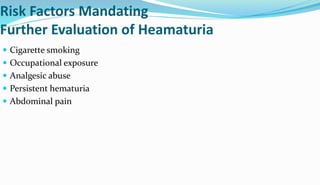
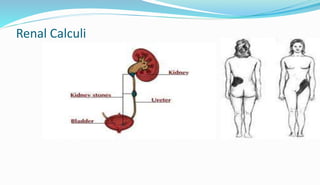
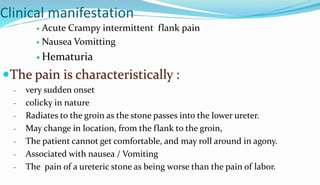
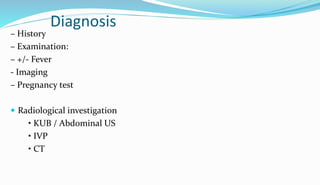
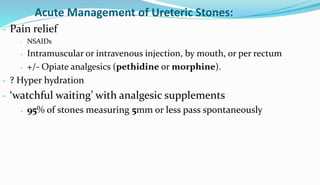
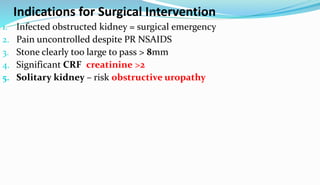
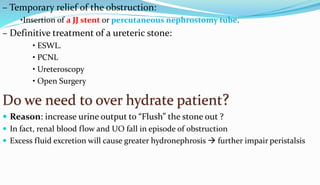
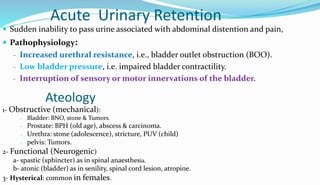
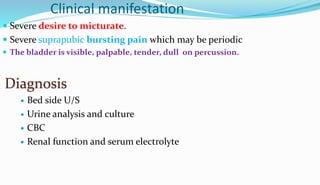
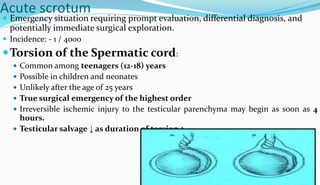
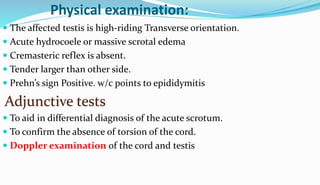
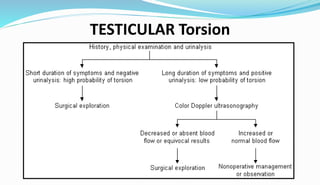
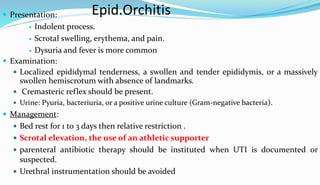
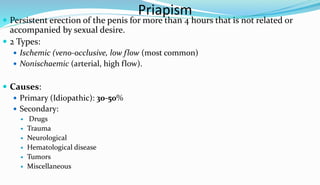
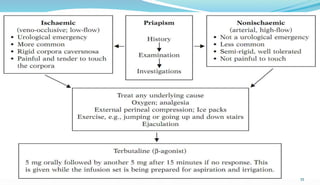
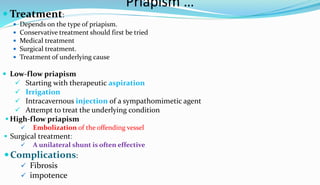
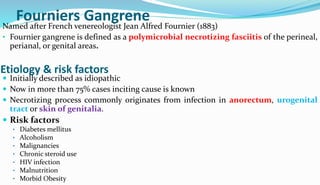
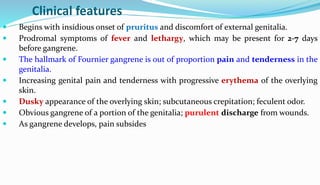
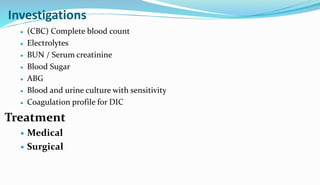
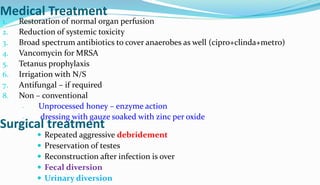
Heyria Hussien's document discusses various non-traumatic urologic emergencies including hematuria, renal colic, urinary retention, acute scrotum, Fournier's gangrene, and priapism. It provides details on the presentation, diagnosis, and management of each condition. Hematuria is discussed in depth including causes, evaluation, and treatment depending on severity and origin. Renal colic caused by kidney stones is described as a common urologic emergency presenting with severe flank pain. Urinary retention can be acute or chronic, with acute retention requiring immediate catheterization. Acute scrotum requires prompt evaluation to differentiate potentially life-threatening testicular torsion from other conditions like epid