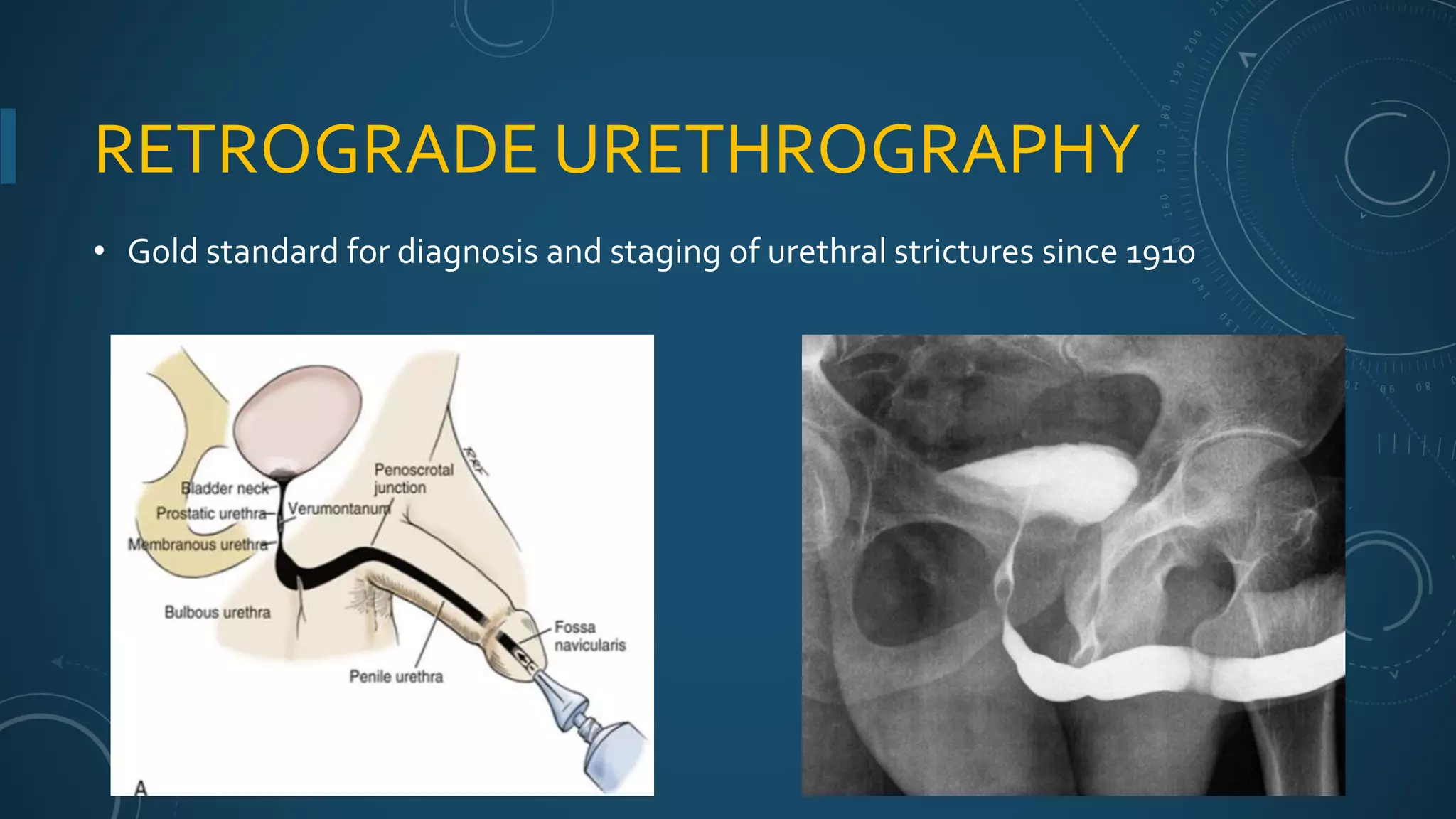
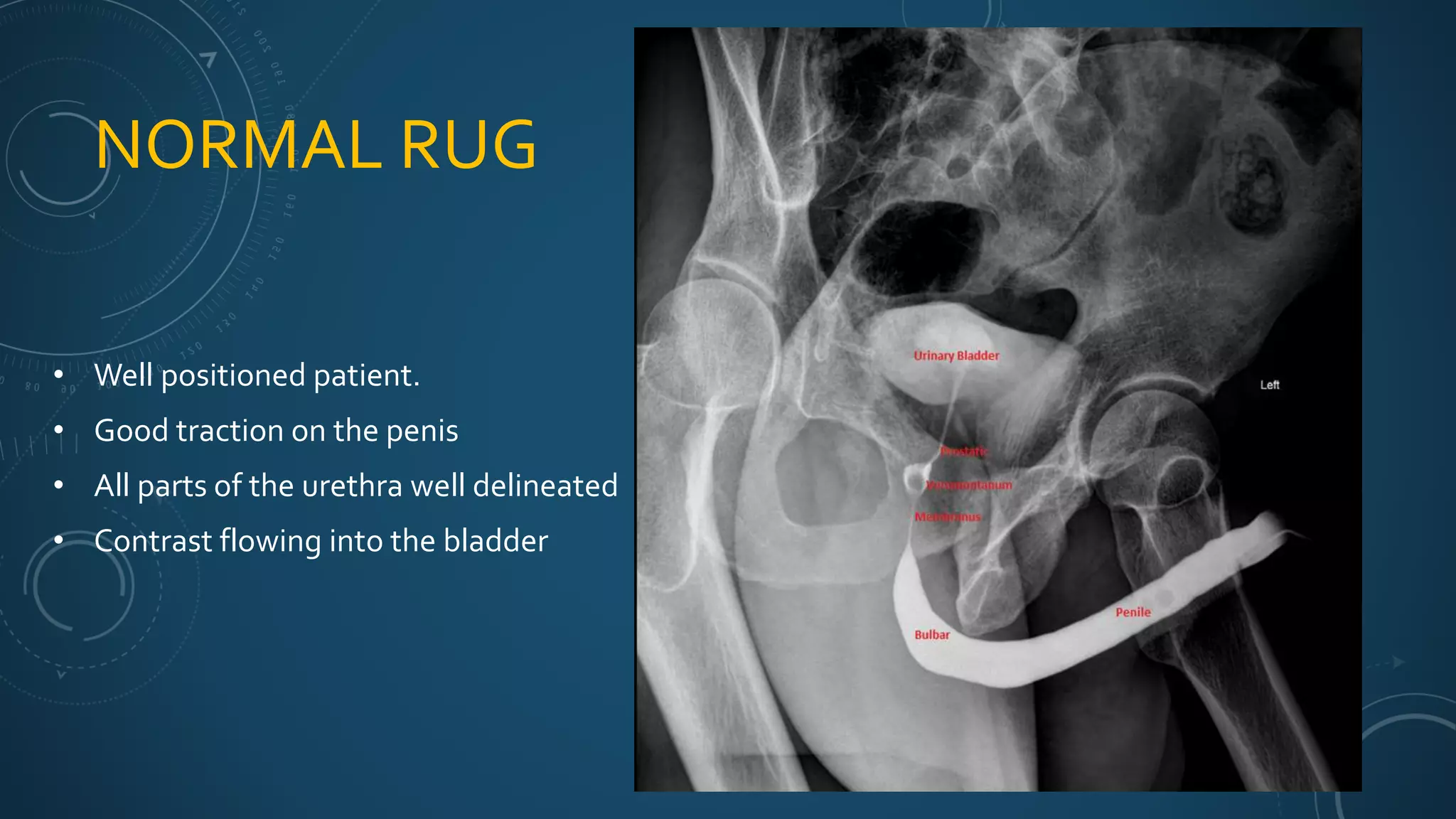
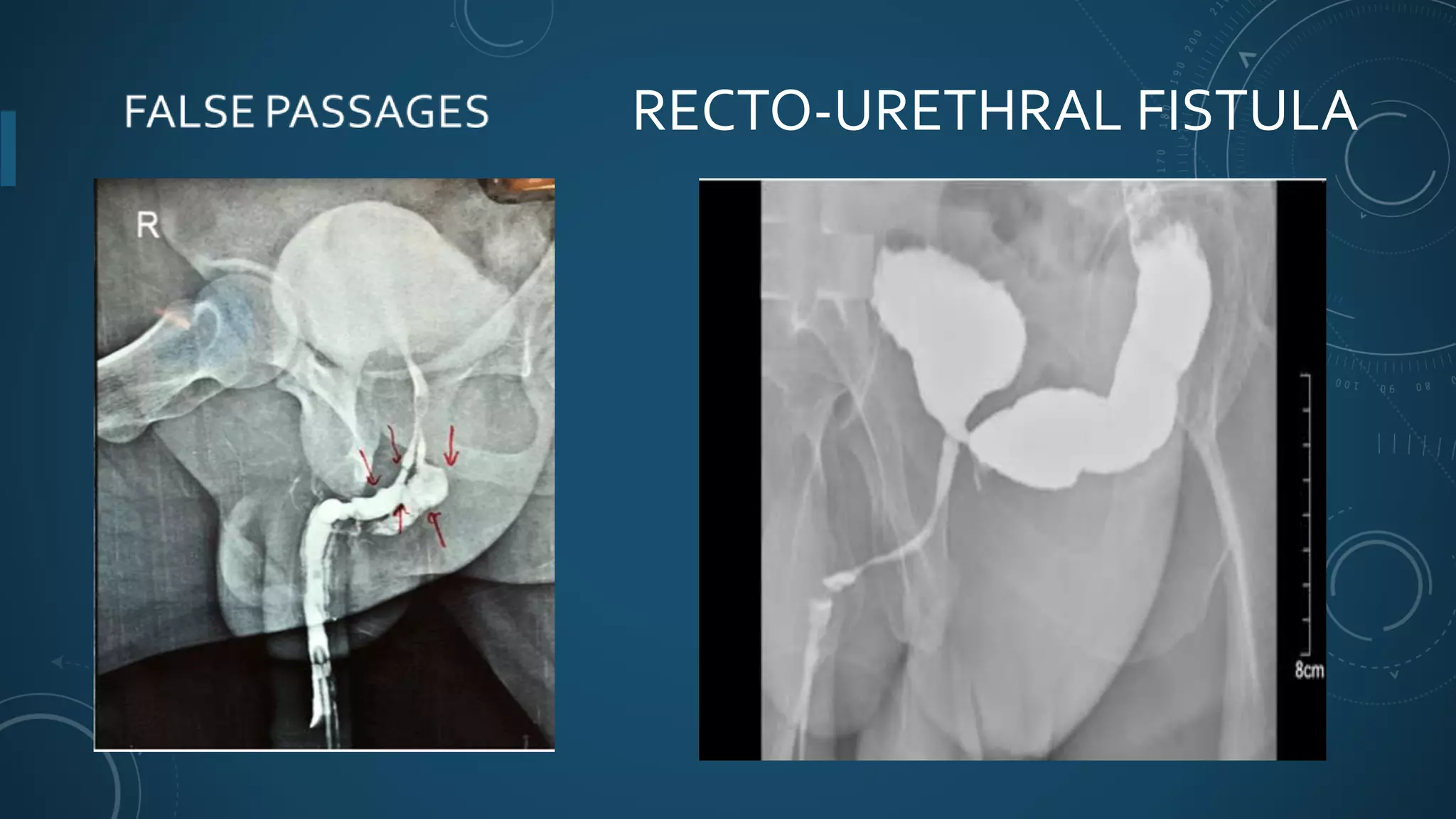
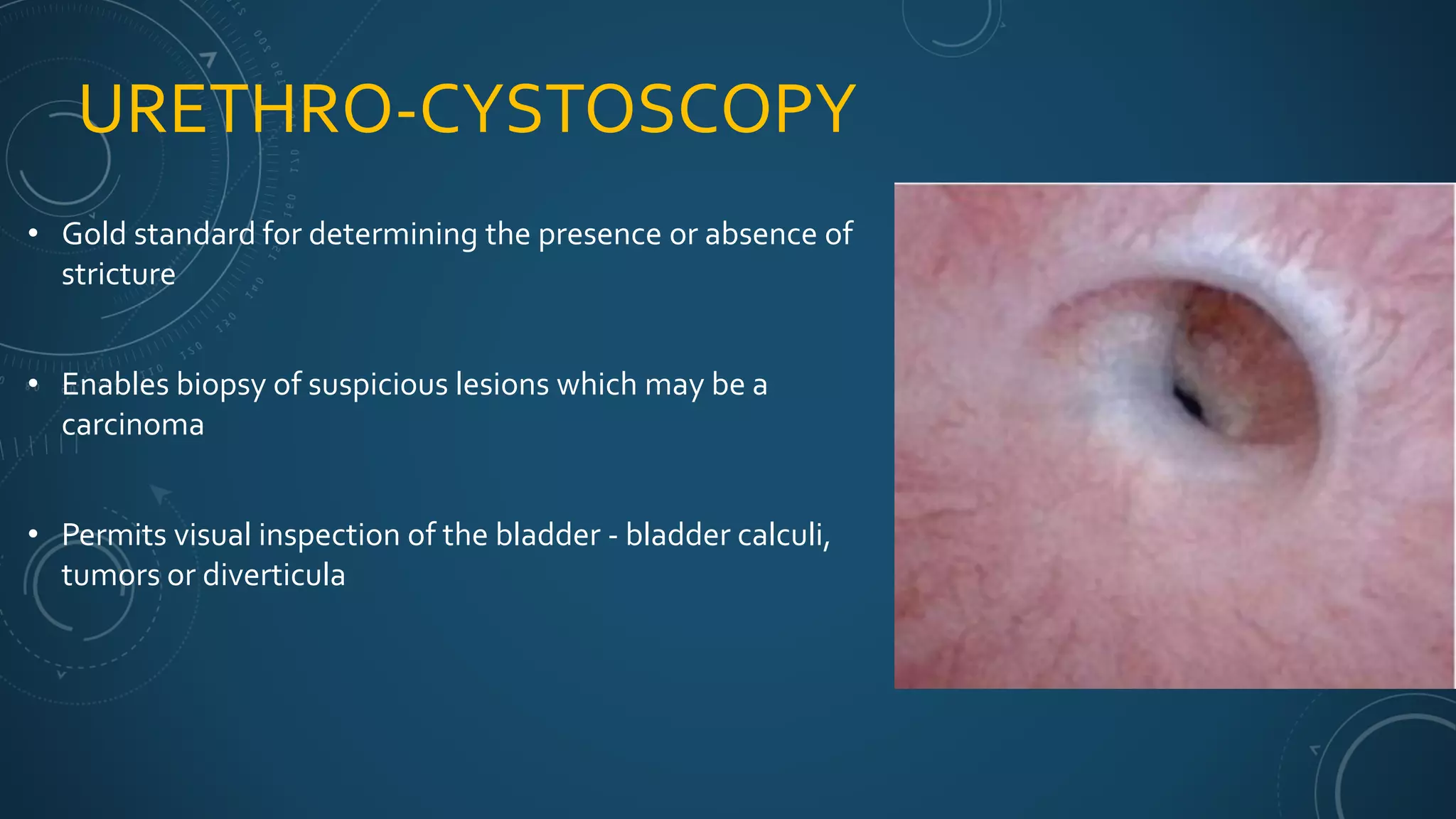
This document discusses urethral strictures, which are narrowings of the urethra caused by scarring. It covers the anatomy and epidemiology of urethral strictures and their various causes including iatrogenic, traumatic, inflammatory, and idiopathic factors. Diagnostic tests like retrograde urethrography and treatments options are outlined, including dilation, direct vision internal urethrotomy, and urethroplasty surgery. Urethroplasty is considered the gold standard treatment but has the highest success rate for short, simple strictures.